Abstract
Purpose
To illustrate the impact on the validity of trial results due to excluding patients from a randomized controlled trial for whom no deferred consent could be obtained after randomization because study procedures had already been finished.
Methods
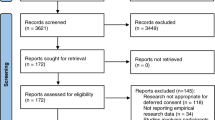
The unadjusted and adjusted primary outcome measures of a recent randomized controlled multicentre study in the field of intensive care medicine were compared, including (n = 348) or excluding (n = 289) patients with missing deferred consent.
Results
Thirty-nine patients (11%) died early, before the patient or his/her proxy could be approached and consent be obtained. In another 20 patients (6%), it was not possible to inform proxies and ask consent within the period of study procedures. A significant treatment effect (p = 0.006) in the adjusted analysis became non-significant (p = 0.35) when the patients with missing deferred consent were excluded.
Conclusions
Exclusion of patients without obtained deferred consent can reduce statistical power, introduce selection bias, make randomization asymmetrical, decrease external validity and thereby jeopardize study results. This may have implications for emergency research in various disciplines.
Similar content being viewed by others
Introduction
Respect for individual autonomy, expressed in the concept of informed consent, is a basic ethical principle in research with humans. Many critically ill patients are unable to give consent as a consequence of mental incapacity, and this can be further complicated in emergency situations, in which treatment needs to be initiated without delay. Proxies are not always available in the first hours of hospital or intensive care admission or are too overwhelmed to understand the provided information to give valid consent. Deferred consent is an acceptable substitute in these emergency circumstances [1]. However, clinicians and investigators may encounter an important practical and ethical problem after enrolling patients under deferred consent: should the researcher use the study data if study procedures have already been finished before it was possible to inform the patient or his/her proxy and ask consent? This includes the situation in which the patient has died early.
The intention-to-treat principle implies that the primary analysis should include all subjects. Compliance with this principle would necessitate complete follow-up of all subjects for study outcomes. As patients who die early are the most severely ill, excluding them could reduce external validity, jeopardize the balance between study arms and influence the effect of the intervention [1, 2].
In an earlier discussion paper, we argued that deferred proxy consent is the preferable substitute for informed consent in emergency critical care research. In case of the situation when study procedures are finished or the patient dies before consent can be obtained, we recommend to use the study data that have already been obtained, provided sufficient privacy measures have been applied. Several arguments support this recommendation. First, using data of patients who died and for whom deferred consent was not yet obtained will not harm the patient or relatives. Second, confronting bereaved relatives to obtain consent after death of the patient is an additional burden. Third, using data will benefit future patients and society. Fourth, the Dutch Central Committee on Research involving Human Subjects (CCMO) stated that the research has ended with the death of the patient and relatives do not have the legal right to give consent for the use of medical data after the patient has died. Finally and most importantly, not using the data will probably jeopardize validity of study results [2].
To support the latter argument, we compared the results of a recent randomized controlled multicentre study in the field of intensive care medicine [3], including or excluding data from patients where study procedures were already finished before consent could be obtained. We hypothesize that not using these data will reduce internal and external validity.
Methods
In the example study, patients with hyperlactatemia on intensive care admission were randomly allocated to either the lactate group or the control group. In the lactate group, resuscitation therapy was guided by blood lactate levels with the objective to decrease lactate levels by 20% or more per 2 h, during the first 8 h of intensive care stay. In the control group the treatment team had no knowledge of lactate levels (except for the admission value). Because of the emergency nature and severity of disease in the target population, patients were enrolled under deferred (proxy) consent: study procedures were temporarily allowed without consent and, as soon as possible, written consent from the patient or legal representative was obtained. In-hospital mortality was the primary outcome measure. This primary outcome was compared between the two randomization groups using the chi-square test and using predefined multivariate Cox proportional-hazards analysis, stratified by centre and sepsis group, where adjustment was made for the following co-variables: age, sex, baseline Acute Physiology and Chronic Health Evaluation II (APACHE II) and baseline Sequential Organ Failure Assessment (SOFA) score [4]. We compared the primary outcome measures in the study population with or without patients where study procedures were already finished before consent could be obtained.
Results
The study population consisted of 348 patients; 39 patients (11%) died early, before the patient or his/her proxy could be approached and consent be obtained. In another 20 patients (6%), it was not possible to inform proxies and ask consent within the period of study procedures (no family available, non-Dutch-speaking family, transfer to other hospital etc.). Table 1 presents baseline characteristics according to obtained consent status. There were more patients with missing consent due to early death in the control group than in the lactate group [14.7% (26/177) versus 7.6% (13/171), p = 0.042]. The number of patients in each group with missing consent due to other reasons (than early death) was similar [control group 6.8% (12/177) versus lactate group 4.7% (8/171), p = 0.492].
Table 2 presents the results of the unadjusted and adjusted primary outcome analyses. A significant treatment effect (p = 0.006) in the adjusted analysis even became non-significant (p = 0.35) when patients with missing deferred consent were excluded. In addition, when adding the variable “missing consent” to the multivariable Cox proportional-hazards model, the treatment effect of lactate-guided therapy was reduced from 0.006 to 0.063. When adding the variable “missing consent due to early death”, the p value was reduced to 0.210. When calculating interaction, we could not demonstrate a significant difference in the unadjusted treatment effect between those with and without missing consent.
Discussion
As illustrated by the data, excluding patients for whom no deferred consent can be obtained after randomization may result in invalid study results. In our study, a significant adjusted treatment effect became non-significant when excluding patients with missing deferred consent. This phenomenon can be ascribed to two different reasons. First, it is the effect of a lack of power due to the reduced sample size in combination with altered mortality rates. This can be illustrated when calculating the actual power in the two populations. Based on an unadjusted absolute mortality reduction from 43.5 to 33.9% in the entire sample size of 348 patients, the calculated power was 45%. This was reduced to 12% when excluding all patients with missing deferred consent (sample size 289 patients, absolute mortality reduction from 33.1 to 28.7%). The second reason is the likely introduction of selection bias. Furthermore, because patients with missing consent were more severely ill, this means that, by excluding these patients, the study population will no longer be representative of the actual population defined by the inclusion and exclusion criteria.
Notably, more patients in the control group had missing consent due to early death than in the lactate group. The baseline characteristics presented in Table 1 show that patients lacking consent were indeed more severely ill. Furthermore, while missing consent due to early death was more frequent in the control group, the proportion of missing consent not due to death was similar between the treatment groups. This suggests that the difference in “obtained consent status” was probably not related to a more systematic search for consent in the lactate group due to the open-label study design, but to a matter of time before the patient’s death.
In conclusion, exclusion of patients with missing informed consent, because study procedures have already been finished before it was possible to obtain consent, can reduce statistical power, introduce selection bias, make randomization asymmetrical, decrease external validity and thereby jeopardize study results. In addition, very few patients or relatives refuse consent for use of already obtained data in emergency situations [1, 3]. Therefore, not using data from patients in whom study procedures have been completed and deferred consent has not been obtained is unethical and, in addition, will be unjust to patients and proxies who have consented for use of data. These findings may have important implications for emergency research in disciplines ranging from intensive care and emergency medicine to cardiology and (trauma) surgery.
References
Jansen TC, Kompanje EJO, Bakker J (2009) Deferred consent in emergency critical care research: ethically valid and practically feasible. Crit Care Med 37:S65–S68
Jansen TC, Kompanje EJO, Druml C, Menon DK, Wiederman CJ, Bakker J (2007) Deferred consent in emergency intensive care research: what if the patient dies early? Use the data or not? Intensive Care Med 33:894–900
Jansen TC, van Bommel J, Schoonderbeek J, Sleeswijk Visser S, van der Klooster J, Lima AP, Willemsen SP, Bakker J (2010) Early lactate-guided therapy in ICU patients: a multicentre, open-label randomized controlled trial. Am J Respir Crit Care Med [Epub ahead of print]
Roozenbeek B, Maas AIR, Lingsma HF, Butcher I, Lu J, Marmarou A, McHugh GS, Weir J, Murray GD, Steyerberg EW (2009) Baseline characteristics and statistical power in randomized controlled trials: selection, prognostic targeting, or covariate adjustment? Crit Care Med 37:2683–2690
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Jansen, T.C., Bakker, J. & Kompanje, E.J.O. Inability to obtain deferred consent due to early death in emergency research: effect on validity of clinical trial results. Intensive Care Med 36, 1962–1965 (2010). https://doi.org/10.1007/s00134-010-1988-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-010-1988-0