Abstract
Objective
Muscle weakness in septic patients is a serious problem as it complicates and lengthens hospital stays, prolongs rehabilitation and increases costs. We examined the effects of a chronic infection with Escherichia coli on muscle function, muscle mass, and the expression of nicotinic acetylcholine receptors (AChRs).
Design and setting
Prospective, randomized animal study in an animal laboratory, university hospital.
Subjects
Sprague-Dawley rats.
Interventions
A catheter was implanted into the external jugular vein of anesthetized rats, and a dose of 3.2 × 108 CFU of E. coli bacteria was injected; the catheter was then sealed and tunneled subcutaneously.
Measurements and results
Animals injected with E. coli bacteria showed a significant decrease in body and muscle mass over the 14-day experimental period. Neuromuscular function was tested by mechanomyography on days 3, 7, and 14 following injection. Tetanic tension decreased over the time course of sepsis, without effecting tetanic fade. Serum levels of acute-phase protein, α1-acid glycoprotein, were increased by day 3, and remained significantly higher until day 14. AChRs were quantitated using 125I-labeled bungarotoxin and revealed no differences between groups.
Conclusions
Central venous injection of E. coli bacteria induces systemic inflammation evidenced as loss of body weight, muscle mass and increased α1-acid glycoprotein levels. The inflammation-induced muscle weakness is due to muscle atrophy and not to upregulated AChRs. This model may prove useful for studying maneuvers to prevent muscle wasting with inflammation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Weakness of limb and respiratory muscles associated with inflammation or critical illness is a common occurrence in intensive care units (ICUs) and is referred to as critical illness polyneuromyopathy (CIPM), since nerve and muscle disorders are concomitantly present [1–6]. CIPM is a chronic disease that requires at least 1 week of critical illness prior to its manifestation [7, 8]. More than 70% of patients with sepsis or multiorgan failure hospitalized in an ICU for more than 1 week develop CIPM [1, 3, 9]. Due to respiratory muscle weakness, failure to wean from mechanical ventilation and subsequent prolonged ventilator dependency are common among affected patients and may be the prevailing symptoms of CIPM. On neurological examination patients show muscle atrophy and severe flaccid tetraparesis [9]. Incidence of complications such as pneumonia, deep vein thrombosis, and pulmonary embolism increases with duration of ventilator dependency. Additionally, patients with CIPM have an increased organ dysfunction score [1, 7]. Therefore the presence of CIPM is associated with prolonged rehabilitation and higher mortality rate. Recent reports indicate that the majority of patients after intensive care treatment of 28 days or more show persistent neuromuscular disabilities and a reduced quality of life [10, 11].
The cause of CIMP is multifactorial, but inflammation and infection have been identified as key contributing factors [1–4, 6]. The origin of altered muscle function can be broadly classified as prejunctional (nerve), junctional (receptor) or postjunctional (muscle abnormality) [12, 13]. Various factors such as administration of neuromuscular blocking agents, antibiotics, and corticosteroids have also been implicated in the pathogenesis of CIPM [1, 9, 12]. Critical illness, however, can also cause muscle dysfunction in the absence of medications [14, 15]. Bolton [1, 3, 12] has speculated that systemic factors present during sepsis, including tumor necrosis factor, histamines, and formation of free radicals induce disturbances in the microcirculation of peripheral nerves and cause axonal degeneration.
Numerous animal models of sepsis have been established in an attempt to study systemic inflammatory effects on homeostatic conditions [16–18]. However, most of the previously described models such as endotoxin injection and bacterial peritonitis induce high mortality or early recovery and have not succeeded in mimicking the chronic catabolic state observed in critically ill patients [16]. The purpose of this study was to develop a septic rat model which reproduces the chronic nature of sepsis, especially the long-lasting muscle wasting. We hypothesized that central venous injection of live E. coli bacteria induces sepsis with decrease in body weight and muscle mass and leads to a persistent increase in inflammatory markers. It furthermore reduces muscle contraction and increases expression of nicotinic acetylcholine receptors (AChRs). To test these hypotheses the effects of E. coli infection on metabolism and neuromuscular junction were studied 3, 7, and 14 days following central venous injection. Preliminary findings of this study were presented at the Annual Meeting of the American Society of Anesthesiologist in 2003.
Material and methods
Animal model, group assignment, and bacteria injection technique
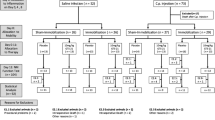
Approval of the study protocol was obtained from the responsible governmental veterinary and animal protection office in Germany (Regierung von Oberbayern, AZ 2091/211–2531-40/2000). Male Sprague-Dawley rats (Charles River, Kisslegg, Germany) weighing 342 ± 33 g were used. Animals were allowed to accommodate to the standard conditions of our animal facility with free access to rat chow and water for at least 1 week. In total 98 animals were randomly allocated to two groups, E. coli and saline. Aiming at similar group sizes for the neuromuscular function test, randomization resulted in a higher mortality rate in the E. coli group by 2:1. Animals of the E. coli group intravenously received 500 μl of a bacterial suspension containing 3.2 × 108 CFU of live E. coli (serotype 0153:KH) reconstituted in 0.9% sterile isotonic saline (Braun, Melsungen, Germany). Three subgroups were studied depending on the day of neuromuscular function tests (day 3, n = 20; day 7, n = 25; day 14, n = 22). Saline animals received an equivalent volume of 0.9% sterile isotonic saline (Braun) in respective subgroups (day 3, n = 10; day 7, n = 10; day 14, n = 11).
For the bacterial injection rats were anesthetized by inhalation of sevoflurane in a glass cylinder. After loss of consciousness the rats were endotracheally intubated and mechanically ventilated with oxygen in nitrous oxide (ratio 1:2). Anesthesia was maintained with 4–5% sevoflurane. The left jugular vein was catheterized and 200 μl blood was withdrawn to determine baseline values of hemoglobin, leukocytes, and platelets. A dose of 3.2 × 108 CFU E. coli bacteria was injected via the catheter, which was subsequently sealed and tunneled subcutaneously to produce a chronically dispersing infection source. After these interventions animals were allowed to recover from anesthesia and then returned to their cages.
Daily monitoring
Body weight was measured daily starting 2 days before infection and continuing over the 14-day experimental period. In accordance with the approved protocol, water and food intake of all animals was monitored daily until the day of the neuromuscular function test, or until they died prior to their measurement day. If the animals did not drink enough water, sterile saline (Braun) was injected subcutaneously. No additional therapeutic interventions were undertaken. The animals were also clinically evaluated daily for signs of infection/inflammation, such as ruffled fur, teary eyes, and decreased locomotor activity.
Anesthesia and vital parameters
Neuromuscular function tests were performed 3, 7, and 14 days after E. coli injection. Rats were again anesthetized, endotracheally intubated with sevoflurane, and mechanically ventilated with supplemental oxygen. After cannulation of the external right jugular vein anesthesia was switched to a continuous infusion of propofol 2% (12–24 mg/kg per hour) and fentanyl (4–16 μg/kg per hour. The right carotid artery was cannulated for monitoring of blood pressure and blood gas analyses. Heart rate and mean arterial pressure were continuously monitored to ensure stable hemodynamic conditions throughout the experiment. Arterial oxygen (PaO2) and carbon dioxide (PaCO2) partial pressures and acid-base status were intermittently measured and corrected if necessary to predefined ranges (PaO2 > 100 mmHg, pH 7.36–7.44, PaCO2 > 36–44 mmHg, base excess –2 ± 2 mM) by adjusting respiratory volume and injection of sodium bicarbonate. Body temperature was controlled between 36.5 °C and 37.2 °C with a warming blanket and heating lamp. At all times the administration of anesthesia was adjusted according to cardiovascular signs of inadequate anesthesia.
Rats were excluded from the experiment if they were hemodynamically unstable (mean arterial blood pressure < 80 mmHg) at the beginning of the experiments, or if their blood gas status throughout the experiment was not within the above predefined ranges.
Neuromuscular function tests
Neuromuscular transmission was monitored by evoked mechanomyography (S88 stimulator and SIU stimulus isolation unit, Grass Telefactor, Astro-Med, Rodgau, Germany). For this purpose rats were placed in supine position. The tendon of the insertion of tibialis cranialis muscle was surgically exposed on each side and individually attached to a Grass FT03 force displacement transducer (FT3, Grass Telefactor). Both sciatic nerves were exposed at its exit from the lumbosacral plexus and tied with ligatures. Stimulation electrodes were attached distal to the ligatures for nerve-mediated stimulation of the tibialis cranialis muscle. The knees were firmly stabilized in a clamp. A baseline tension of approx. 50 g was applied to the tendon of each tibialis cranialis muscle, which yielded optimal evoked tensions. The nerve-evoked tension of the respective tibialis muscle was recorded on a Grass P122 amplifier and printed on paper (Schwarzer Uniscript DU 210, Schwarzer-Picker, Munich, Germany). Mean values of both recordings were calculated and expressed in newtons.
Initially, supramaximal stimulus and baseline twitch tension were established. The baseline mechanomyographic responses were stabilized over a period of 20 min using a 1-Hz single twitch tension stimulation pattern. The mean values of the previous ten single twitches were calculated for single twitch tension values. Following this, tetanic stimulation with 100 Hz for 5 s was applied to assess the maximal tetanic muscle tension and the muscle fade associated with this stimulus. Specific tensions (single and tetanic twitch) were calculated as force (N) per milligram of tibialis cranialis muscle mass. Tetanic fade (fatigability) was calculated as (initial peak contraction–final contraction at the end of 5 s) × 100/initial peak contraction. Following the neuromuscular function test animals were killed by exsanguination.
In vitro analyses
Whole blood was withdrawn during exsanguination to determine hemoglobin, leukocytes, and platelets. The remaining blood was centrifuged (3,500 rpm, 10 min, 4 °C), and the serum was separated and immediately stored at –70 °C for determination of α1-acid glycoprotein concentrations (α1-AGP). Both tibialis cranialis, gastrocnemius, and soleus muscles were harvested, weighed, flash-frozen on dry ice, and stored at –70 °C for later analysis of the acetylcholine receptor number. Muscle mass was calculated as the sum of the harvested tibialis cranialis, gastrocnemius, and soleus muscles of both legs.
alpha1-Acid glycoprotein chemiluminescence immunoassay
Serum levels of α1-AGP were evaluated using a competitive chemiluminescence immunoassay, as described previously [19].
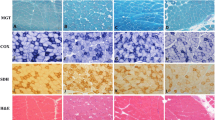
Acetylcholine receptor assay
The AChR protein expression in the tibialis cranialis was assayed using the 125I-labeled α-bungarotoxin binding assay, as previously described [15]. The protein concentration of the muscle extract was measured using the Bio-Rad DC protein assay kit (Bio-Rad Laboratories, Herkules, Calif., USA). Values of AChRs are expressed as fmol/mg protein.
Statistical analysis
Thirteen rats were excluded due to technical difficulties (E. coli, n = 8; saline, n = 5), and 26 animals died due to inflammation/or infection after injection of E. coli (mortality 44%). The final statistical analysis included 33 animals in the E. coli group (day 3, n = 10; day 7, n = 13; day 14, n = 10) and 26 in the saline group (day 3, n = 9; day 7, n = 7; day 16, n = 10). Values were compared by two-way repeated-measurements analyses of variance using day (3, 7, and 14) and group (saline and E. coli) as independent factors. Level of significance was set at p < 0.05. Post-hoc analysis was performed with paired and unpaired t-tests (p < 0.05).
Results
Mortality rate and systemic signs of inflammation
During the 2 days prior to the bacterial injection there were no significant differences in body weight between groups. E. coli infection induced a marked decline in body weight on day 1 after injection vs. saline injected controls. Over the 14-day experimental period mean body weight in the E. coli group was significantly lower than that in time-matched saline injected controls (Fig. 1). The muscle mass of the harvested muscles was significantly reduced in E. coli injected animals on days 3, 7, and 14 after infection (Table 1). Starting on day 3, E. coli injected rats showed the typical clinical signs of infection/inflammation including ruffled fur, teary eyes, and decreased locomotor activity. These signs were absent in all saline-injected animals. On day 0 leukocytes and platelets levels did not differ between septic animals and controls (Table 2). On day 3 after injection leukocytes were significantly increased in E. coli injected animals while platelets were reduced vs. controls (Table 2). On days 7 and 14 the leukocytes and platelets no longer differed between groups. Hemoglobin levels were significantly reduced over the experimental period (Table 2). Plasma concentrations of acute-phase protein α1-AGP, were significantly elevated on days 3, 7, and 14 (Table 2).
Body weight was measured daily starting 2 days before infection and continuing over the 14-day experimental period. Saline-injected animals served as controls. During the 2 days of accommodation in our animal facility there were no significant differences in body weight between groups. Over the experimental period body weight of the E. coli injected animals was significantly lower than those of their time-matched saline-injected controls. Data are presented as mean ± SD; values are expressed in grams
Neuromuscular function test and acetylcholine receptor expression
Despite the decrease in muscle mass with E. coli injection nerve-evoked single twitch tension did not differ between the saline and E. coli groups (Fig. 2). After twitch tension was normalized to muscle mass (tension/g muscle tension), there were also no differences between groups. Although there were no significant changes in absolute and specific tetanic tensions on day 3, there was a significant decrease in tetanic tension in E. coli animals vs. their time-matched controls 7 and 14 days after injection (Fig. 3). These differences disappeared when normalized to muscle mass. There were no differences in tetanic fade or in the expression of acetylcholine receptors (Table 1) between groups.
Evoked single twitch tension in the tibialis cranialis muscle. On 3, 7, and 14 days following E. coli injection single-twitch tension was measured by evoked mechanomyography. Single-twitch tension did not differ in E. coli injected animals relative to their time-matched saline-injected controls. Data are presented as mean ± SD; values are expressed in newtons
Peak tetanic tension in the tibialis cranialis muscle. On 3, 7, and 14 days following E. coli injection the tetanic tension was measured by evoked mechanomyography. Tetanic tension was significantly decreased in E. coli injected animals relative to saline injected controls on days 7 and 14. Data are presented as mean ± SD; values are expressed in newtons
Model stability
Hemodynamic and metabolic variables were kept in physiological ranges throughout the functional studies. These values did not differ between groups, and therefore group means are reported. Mean arterial pressure was 92 ± 32 mmHg, heart rate 325 ± 48 bpm, base excess 0.9 ± 2.6 mM, blood glucose level 105 ± 30 mg/dl, and body temperature ranged between 36.6 ± 0.1 °C and 37.0 ± 0.1 °C.
Discussion
This study documents that the central venous injection of E. coli induces the typical clinical signs of inflammation, evidenced as clinical deterioration, decreased body weight and muscle mass and increased levels of acute-phase protein. The induced sepsis reduced tetanic tension due to muscle atrophy. The infection had no effect on tetanic fade or expression of acetylcholine receptors.
CIPM is a chronic disease that requires at least 1 week of critical illness prior to its manifestation [7, 8]. Previous models of inflammation and sepsis have been described in effort to establish a clinically relevant paradigm suitable for studying their effects on organ function [16–18]. Some of the proposed models such as endotoxin or peritonitis models, however, enable only short-term observations as the majority of animals die within 24–48 h after injection of the agent while some others show a rapid recovery to normal health [16–18, 20]. Breuille et al. [16] established a rat sepsis model produced by administration of E. coli via the tail vein leading to a catabolic state for 9 days. A single injection of bacteria, however, does not simulate the intermittent release of pathogenes in septic patients in the ICU. Recent studies indicate that catheter-related infections remain the major cause of nosocomial infection in ICUs [21]. Therefore we developed a new inflammation model by injecting live E. coli bacteria over a central venous line and leaving part of the catheter subcutaneously in an attempt to closely simulate clinical conditions of a catheter sepsis. Our model of inflammation resulted in a mortality rate of 44% in the E. coli injected group. This is contradictory to the findings of Breuille et al., in whose study only one of eight rats died following a single injection of 6.8 × 108 CFU of live E. coli (serotype 0153:KH) bacteria [16].
Systemic markers of infection include alterations in the hematopoietic system. In the surviving E. coli animals injection of bacteria via a central venous line led to leukocytosis and thromboctopenia on day 3 and to a significant decrease in hemoglobin levels throughout the 14-day course of the experiments. In addition, α1-AGP, an acute-phase protein comparable to C-reactive protein, remained significantly elevated for 14 days. Changes in α1-acid glycoprotein levels during inflammation led to an increased binding of cationic molecules (e. g., neuromuscular blocking agents), which alters pharmacodynamics and pharmacokinetics of these drugs [22]. This model could be used to study these pharmacological changes during inflammation or infection.
Metabolic signs of infection include loss of body weight and muscle mass [16, 23]. In this study E. coli infection induced a significant decline in body weight over the 14-day experimental period. In analogy to the previously described triphase course by Voisin et al. [24], bacteria-injected animals showed a significant drop in body weight between days 1 and 3, followed by a plateau with stable body weight levels until day 8. By day 9 septic animals gained body weight in a manner similar as their saline-injected controls [16, 23, 24]. In our study muscle mass was reduced in infected animals up to 14 days of observation. This muscle wasting in inflammation or infection results from both a decrease in protein synthesis [25, 26] and an increase in protein degradation [27, 28], most likely due to previous described complex interactions of cytokines (tumor necrosis factor α, interleukins 1 and 6) and hormones (insulin, insulin-like growth factor) during the septic episode [2]. This model may therefore serve for making long-term observations on muscle changes during therapeutic manipulations.
Looking at the functional effects of infection on muscle, single-twitch stimulation did not reveal any muscle weakness. However, 100 Hz tetanic stimulation, mimicking increased workload by synchronized maximal fused contraction of all fibers, showed a decrease in contraction force on days 7 and 14. After tetanic tension was normalized to muscle mass (specific tetanic tension), the decreased tension was annulled, indicating that muscle atrophy is a possible cause of decreased tetanic tension in our model. The lack of changes in specific tetanic tension is in concordance with findings in muscles after immobilization, which induces a reduction in force-generating capacity of muscles in parallel with a decline in muscle mass and fiber size. These effects peak by day 7–14 of disuse [15]. Our observations in this study contrast with results in muscles underneath burn injury, which show reduction in force generating capacity primarily due to reduction in specific tension [29]. In the latter case factors other than muscle atrophy may account for the decrease in muscle function.
Changes in expression of AChR at the neuromuscular junction are concomitantly seen during critical illness together with muscle wasting [30–33]. Established factors that induce AChR upregulation include denervation, immobilization, burn injury, and upper and lower motor neuron injury [31, 33]. Upregulation of AChRs is clinically associated with a spread into the peri- and extrajunctional area, changes in subunit composition (immature vs. mature), and its subsequent prolonged mean channel open time [31, 33, 34]. Clinically an increased expression of AChR is a well established risk factor for succinylcholine-induced hyperkalemia [33, 35, 36]. However, in a model of cecal ligation and puncture, just the contrary has been demonstrated, namely that infection and inflammation reduced AChRs numbers leading to a myasthenialike state [37]. In our study however, expression of membrane AChRs was not affected by the central venous injection of E. coli. Clinical reports of critical ill patients showing hyperkalemia following injection of succinylcholine as an indirect measure of AChR upregulation might therefore be due to the concomitant total body immobilization with and without neuromuscular blocking agents acting in combination with the infection itself [33].
In conclusion, this study describes a clinically relevant chronic sepsis model. We demonstrated that central venous injection of E. coli bacteria induces the typical changes in body weight, muscle mass, and acute-phase protein. The tetanic tension of the tibialis cranialis muscle decreased with time course of inflammation/infection, without effecting tetanic fade and expression of acetylcholine receptors. Mechanisms of muscle wasting with inflammation and therapeutic maneuvers to prevent it could be tested with this model.
References
Bolton CF (2005) Neuromuscular manifestations of critical illness. Muscle Nerve 32:140–163
Zochodne DW, Bolton CF (1996) Neuromuscular disorders in critical illness. Baillieres Clin Neurol 5:645–671
Bolton CF (1993) Neuromuscular complications of sepsis. Intensive Care Med Suppl 19(2):S58–S63
Bednarík J, Vondracek P, Dusek L, Moravcova E, Cundrle I (2005) Risk factors for critical illness polyneuromyopathy. J Neurol 252:343–351
Johnson KL (2007) Neuromuscular complications in the intensive care unit: critical illness polyneuromyopathy. AACN Adv Crit Care 18:167–180
Rannou F, Pennec JP, Rossignol B, Morel J, Dorange G, Arvieux C, Gioux M, Giroux-Metges MA (2007) Effects of chronic sepsis on rat motor units: experimental study of critical illness polyneuromyopathy. Exp Neurol 204:741–747
De Letter MA, Schmitz PI, Visser LH, Verheul FA, Schellens RL, Op de Coul DA, van der Meche FG (2001) Risk factors for the development of polyneuropathy and myopathy in critically ill patients. Crit Care Med 29:2281–2286
De Jonghe B, Sharshar T, Lefaucheur JP, Authier FJ, Durand-Zaleski I, Boussarsar M, Cerf C, Renaud E, Mesrati F, Carlet J, Raphael JC, Outin H, Bastuji-Garin S (2002) Paresis acquired in the intensive care unit: a prospective multicenter study. JAMA 288:2859–2867
Hund E (2001) Neurological complications of sepsis: critical illness polyneuropathy and myopathy. J Neurol 248:929–934
Fletcher SN, Kennedy DD, Ghosh IR, Misra VP, Kiff K, Coakley JH, Hinds CJ (2003) Persistent neuromuscular and neurophysiologic abnormalities in long-term survivors of prolonged critical illness. Crit Care Med 31:1012–1016
Visser LH (2006) Critical Illness polyneuropathy and myopathy: clinical features, risk factors and prognosis. Eur J Neurol 13:1203–1212
Bolton CF (1996) Sepsis and the systemic inflammatory response syndrome: neuromuscular manifestations. Crit Care Med 24:1408–1416
Sieck GC, Prakash YS (1995) Fatigue at the neuromuscular junction. Branch point vs. presynaptic vs. postsynaptic mechanisms. Adv Exp Med Biol 384:83–100
Coakley JH, Nagendran K, Hanover M (1993) Neuromuscular abnormalities in the critical ill. Intensive Care Med 19:323–328
Ibebunjo C, Martyn JA (1999) Fiber atrophy, but not changes in acetylcholine receptor expression, contributes to the muscle dysfunction after immobilization. Crit Care Med 27:275–285
Breuille D, Voisin L, Contrepois M, Arnal M, Rose F, Obled C (1999) A sustained rat model for studying the long-lasting catabolic state of sepsis. Infect Immun 67:1079–1085
Fink MP, Heard SO (1990) Laboratory models of sepsis and septic shock. J Surg Res 49:186–196
Wichterman KA, Baue AE, Chaudry IH (1980) Sepsis and septic shock–a review of laboratory models and a proposal. J Surg Res 29:189–201
Metzger J, Blobner M, Luppa PB (2001) Sensitive chemiluminescence immunoassay for the determination of rat serum alpha1-acid glycoprotein. Clin Chem Lab Med 39:514–518
Breuille D, Rose F, Arnal M, Melin C, Obled C (1994) Sepsis modifies the contribution of different organs to whole-body protein synthesis in rats. Clin Sci (Lond) 86:663–669
Andrews P, Azoulay E, Antonelli M, Brochard L, Brun-Buisson C, De Backer D, Dobb G, Fagon JY, Gerlach H, Groeneveld J, Macrae D, Mancebo J, Metnitz P, Nava S, Pugin J, Pinsky M, Radermacher P, Richard C (2005) Year in review in intensive care medicine. I. Experimental studies. Clinical studies: brain injury, renal failure and endocrinology. Intensive Care Med 33:49–57
Fink H, Luppa P, Mayer B, Rosenbrock H, Metzger J, Martyn JA, Blobner M (2003) Systemic inflammation leads to resistance to atracurium without increasing membrane expression of acetylcholine receptors. Anesthesiology 98:82–88
Cooney RN, Kimball SR, Vary TC (1997) Regulation of skeletal muscle protein turnover during sepsis: mechanisms and mediators. Shock 7:1–16
Voisin L, Breuille D, Combaret L, Pouyet C, Taillandier D, Aurousseau E, Obled C, Attaix D (1996) Muscle wasting in a rat model of long-lasting sepsis results from the activation of lysosomal, Ca2+-activated, and ubiquitin-proteasome proteolytic pathways. J Clin Invest 97:1610–1617
Rennie MJ, Edwards RH, Emery PW, Halliday D, Lundholm K, Millward DJ (1983) Depressed protein synthesis is the dominant characteristic of muscle wasting and cachexia. Clin Physiol 3:387–398
Vary TC, Kimball SR (1992) Regulation of hepatic protein synthesis in chronic inflammation and sepsis. Am J Physiol 262:C445–C452
Clowes GH Jr, George BC, Villee CA Jr, Saravis CA (1983) Muscle proteolysis induced by a circulating peptide in patients with sepsis or trauma. N Engl J Med 308:545–552
Hasselgren PO, Talamini M, James JH, Fischer JE (1986) Protein metabolism in different types of skeletal muscle during early and late sepsis in rats. Arch Surg 121:918–923
Ibebunjo C, Martyn J (2001) Disparate dysfunction of skeletal muscles located near and distant from burn site in the rat. Muscle Nerve 24:1283–1294
Blobner M, Kochs E, Fink H, Mayer B, Veihelmann A, Brill T, Stadler J (1999) Pharmacokinetics and pharmacodynamics of vecuronium in rats with systemic inflammatory response syndrome: treatment with NG-monomethyl-L-arginine. Anesthesiology 91:999–1005
Martyn JA, White DA, Gronert GA, Jaffe RS, Ward JM (1992) Up-and-down regulation of skeletal muscle acetylcholine receptors. Effects on neuromuscular blockers. Anesthesiology 76:822–843
Tomera JF, Martyn J (1989) Intraperitoneal endotoxin but not protein malnutrition shifts d-tubocurarine dose-response curves in mouse gastrocnemius muscle. J Pharmacol Exp Ther 250:216–220
Martyn JA, Richtsfeld M (2006) Succinylcholine-induced hyperkalemia in acquired pathologic states: etiologic factors and molecular mechanisms. Anesthesiology 104:158–169
Vincent A, Newland C, Croxen R, Beeson D (1997) Genes at the junction-candidates for congenital myasthenic syndromes. Trends Neurosci 20:15–22
Kohlschutter B, Baur H, Roth F (1976) Suxamethonium-induced hyperkalaemia in patients with severe intra-abdominal infections. Br J Anaesth 48:557–562
Gronert GA (1999) Succinylcholine hyperkalemia after burns. Anesthesiology 91:320–322
Tsukagoshi H, Morita T, Takahashi K, Kunimoto F, Goto F (1999) Cecal ligation and puncture peritonitis model shows decreased nicotinic acetylcholine receptor numbers in rat muscle: immunopathologic mechanisms? Anesthesiology 91:448–460
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Frick, C.G., Fink, H., Gordan, M.L. et al. Chronic Escherichia coli infection induces muscle wasting without changing acetylcholine receptor numbers. Intensive Care Med 34, 561–567 (2008). https://doi.org/10.1007/s00134-007-0852-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-007-0852-3