Abstract
Objective
To assess and compare the effects of physiotherapy and suction on expired tidal volume (VTE), respiratory compliance (Crs), resistance (Rrs) and arterial blood gases.
Design
Randomised cross-over study comparing outcomes after both treatments on the same day.
Setting
Intensive tertiary care units, Great Ormond Street Hospital, London.
Patients
One hundred children on full ventilatory support requiring physiotherapy. Paired measurements were obtained in 90 participants, and 7 others were excluded because of tracheal tube leak.
Interventions
Respiratory physiotherapy and suction.
Measurements and results
Physiotherapy lasted longer and required more saline and catheters per treatment. There were no significant group changes in VTE or Crs after either treatment, but a tendency for Rrs to fall following physiotherapy which reached significance in patients on volume-preset ventilation. There were also small but statistically significant reductions in HCO3 −, base excess and SaO2 after physiotherapy. VTE and Crs increased and Rrs decreased in excess of their 95% limits of agreement for normal variability in approximately twice as many subjects following physiotherapy than suction, these differences being significant for VTE and approaching significance for Crs and Rrs.
Conclusions
Physiotherapy appeared to have an advantage in reducing Rrs in some patients, but also produced changes in derived blood gas parameters. Within individuals, physiotherapy treatments were also more likely to produce improvements in VTE, Crs and Rrs than suction. Further research should identify sensitive patient selection criteria and assess longer-term effects of such treatments.
Similar content being viewed by others
Introduction
Mechanically ventilated children and infants cannot adequately clear airway mucus when sedated or pharmacologically paralysed, since the ability to cough is compromised or absent. Mucus accumulation predisposes patients to respiratory infections, airflow obstruction and discomfort [1]. Routine chest physiotherapy and suction aim to remove airway secretions, improve delivery of ventilation, prevent or resolve respiratory complications and facilitate early weaning, thereby reducing lung damage associated with mechanical ventilation [2]. Until recently studies to assess the clinical effectiveness of such treatments have been limited by the lack of objective measures of respiratory function. Technological advances have now facilitated non-invasive measurement of respiratory function at the bedside [3].
The term “physiotherapy” in this and the accompanying manuscript [4] describes the respiratory therapy commonly performed in ventilated children, which includes the use of manual techniques (chest wall vibrations, percussion, compressions, manual hyperinflation, positioning and postural drainage), saline instillation and tracheal suction. These procedures are not exclusively performed by physiotherapists and do not constitute the entirety of physiotherapy care for ventilated children. Routine suction does not generally incorporate manual techniques and is usually but not exclusively performed by nurses. There is little firm evidence to substantiate the use of physiotherapy in ventilated children or to recommend it in preference to suction techniques [5].
A recently validated, portable, non-invasive respiratory monitor (“CO2SMO Plus”, version 3.0, Novametrix Medical Systems, Conn., USA) was used to measure respiratory function before and after physiotherapy and suction procedures in the same ventilated children. The principal aims of the study were: (a) to assess the short-term effects of physiotherapy and suction on expired tidal volume (VTE), respiratory resistance (Rrs), compliance (Crs) and arterial blood gases in critically ill infants and children and compare differences between these treatments; (b) to evaluate the range of individual responses with respect to the proportion demonstrating significant changes in these parameters shortly after physiotherapy or suction.
Materials and methods
Recruitment
Data were collected in the cardiac and general intensive care units at Great Ormond Street Hospital for Children, London, between April 1998 and March 2000.
While suction is generally performed in all mechanically ventilated patients at this hospital, physiotherapy is not. To enable comparison of these interventions ventilated infants or children were eligible for recruitment if they were both pharmacologically paralysed and deemed, after assessment by the respiratory physiotherapist, to require physiotherapy. Infusions of vecuronium, midazolam and morphine provided muscle relaxation, sedation and analgesia, respectively, according to standard protocols. As none of the participants were making independent respiratory efforts, passive Crs and Rrs could be calculated from pressure changes at the airway opening without oesophageal manometry [6, 7]. The Great Ormond Street Hospital and Institute of Child Health Research Ethics Committee approved the study, and written informed consent was obtained from parents.
Protocol
Patients were randomly assigned to receive either physiotherapy or suction in the morning and the alternative intervention in the afternoon. The order of treatment was randomised by witnessed coin toss at the bedside. The minimum interval between treatments was 90 min, and subjects were excluded from analysis if further airway clearance was required within this period.
The CO2SMO Plus respiratory monitor was used to measure VTE, Rrs and Crs for at least 15 min before and 30 min after each treatment. Measurements were continued for 60 min following treatment if other clinical interventions were not required. Data were summarised as the mean±SD from the 15-min epochs before and after interventions. Blood samples from existing arterial lines were analysed immediately before and 30 min after treatment using the Hewlett Packard i-Stat portable clinical analyser (i-STAT, N.J. USA) [8]. Ventilator settings, including fractional inspired oxygen concentration (FIO2) were held constant during the measurements and recorded for each subject in addition to mode of ventilation, oxygenation index (OI), tracheal tube internal diameter, flow sensor size, age and weight. Inspiratory gases were warmed (37°C) and humidified.
Within and between epoch repeatability of VTE, Crs and Rrs was assessed in 33 participants by comparing mean results from consecutive 15-min recordings under steady state conditions, where the only intervention was removal and re-insertion of the CO2SMO Plus sensor into the ventilator circuit.
Physiotherapy and suction procedures were flexibly defined to allow comparison of these techniques in a way that approximated clinical reality. Any combination of pre-oxygenation, saline instillation, manual hyperinflation and suction was permissible, with as many or few cycles as necessary. Physiotherapy additionally included the manual techniques defined earlier. Treatment details, experience of practitioner and adverse events were recorded for both interventions.
Equipment
The CO2SMO Plus measured pressure and flow at the airway opening via a small disposable, fixed-orifice, differential flow sensor inserted between the tracheal tube and the ventilator circuit [9]. VT was integrated from flow and VTE used in preference to inspired VT to minimise errors due to leak in children with an uncuffed tracheal tube [10, 11]. Crs and Rrs were calculated for each breath by least squares regression of volume, pressure and flow data points throughout the breath cycle [12], but only the passive expiratory portion of Rrs was recorded as it provides more clinically important information about the large airways and less about the ventilator than inspiratory Rrs [13].
The accuracy and validity of the equipment were established during substantial in vitro examination, details of which may be found in the Electronic Supplementary Material. Accuracy was considered clinically robust provided that tracheal tube leak was less than 20%. In the presence of leaks greater than 20%, Crs and Rrs are both grossly overestimated [10, 11, 14, 15]. The magnitude of tracheal tube leak (calculated as the percentage difference between inspired tidal volume (VTI) and VTE, divided by VTI) was recorded throughout the measurement periods [11].
Statistical analysis
Paired t tests with 95% confidence intervals (CI) of the difference were performed to assess (a) the repeatability of VTE, Crs and Rrs in the absence of any intervention, (b) the independent effects of physiotherapy and suction on VTE, Crs, Rrs and arterial blood gases, and (c) to compare group differences in response to these two therapies [16]. The proportion of individuals in whom changes in respiratory parameters following either treatment exceeded the 95% limits of agreement (LA) in the absence of any clinical interventions was also assessed. The 95% LA represent the upper and lower limits within which any difference between repeat measures in the absence of any intervention would be likely to fall on 95% of occasions (mean difference ±2 SD of difference). Changes in excess of these limits are considered likely to reflect significant within subject changes [17].
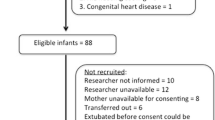
Results
Participants
A total of 100 infants and children were recruited. Paired comparisons were not possible in 10 due to changes in ventilation or clinical circumstances. Of the 90 children with successful paired respiratory function measurements, 79 were ventilated via an uncuffed tracheal tube, seven of whom had to be excluded from subsequent analysis due to a mean tracheal tube leak greater 20% [11]. The majority of participants with a primary cardiac diagnosis had undergone surgery for a congenital cardiac defect, some of whom had delayed sternal closure. Other diagnoses in this group included pulmonary hypertension and cardiac transplantation. Patients with primary or secondary respiratory problems included those with respiratory failure, head injury, major abdominal surgery, bone marrow transplantation, asthma, inhalation injuries and tracheal reconstruction. Demographic details of the remaining 83 are presented in Table 1. Arterial blood gases were measured before and 30 min after both treatments in 71/83 participants.
Differences between treatments
Physiotherapy was allocated as the first treatment 52% of the time. The mean±SD duration of physiotherapy was significantly longer than suction (8.5±3.5 vs. 5.6±2.7 min, p<0.0001), involved more saline instillation (3.6±2.4 vs. 1.8±1.6 ml, p<0.0001) and required more suction catheters per treatment (3.2±1.3 vs. 2.7±1.4, p<0.004). Typically, physiotherapy consisted of pre-oxygenation, saline instillation, manual hyperinflation with chest wall vibrations during expiration, followed by tracheal suction and further re-inflation breaths. Chest wall vibrations were used in 96% of physiotherapy treatments (median 18, range 0–55) while percussion was rarely performed. Suction involved a similar combination of procedures but without manual techniques. Number of treatment cycles depended on assessment of pulmonary secretions and haemodynamic tolerance, but neither treatment duration nor number of vibrations appeared to be influenced by diagnosis, age or sputum yield for either intervention.
Treatments took less than 12 min on 80% and 96% of occasions for physiotherapy and suction, and maximal treatment times were 33 and 20 min, respectively. Between one and eight suction catheters, each passed only once, were used during both interventions (suction pressures 15–25 kPa). Tracheal saline instillation was used in 98% and 82% of physiotherapy and suction interventions, exceeding 1.5 ml/kg in 20% of physiotherapy treatments, but never during suction. Short-lived adverse events such as temporary drop in oxygen saturation (SaO2) or blood pressure occurred in 7% of physiotherapy and 13% of suction procedures. These did not warrant change in ventilation and were resolved either by a transient (<5-min) increase in FIO2 or termination of the intervention. They were not determined by participant’s age or diagnosis.
Repeatability
Within epochs, recordings of respiratory parameters in this paralysed, fully ventilated population were highly reproducible, with the coefficient of variation (CV) for VTE, Crs and Rrs being 1.1%, 0.9% and 4.2%, respectively
Between epochs, when recordings were repeated in 33 subjects (median age 21 months; range 2 weeks–16 years) with no intervention but removal and reinsertion of the CO2SMO Plus sensor, there was no significant change in any parameter. The 95% LA were −5% to 6% for VTE, −7% to 5% for Crs and −15% to 12% for Rrs.
Effect of physiotherapy and suction on respiratory function
After 15 min there were no significant group changes in VTE or Crs following physiotherapy (Table 2) or suction (Table 3) irrespective of ventilation mode or diagnosis. However, there was a tendency for Crs to fall after suction in infants on pressure-preset ventilation (p=0.07). This change became significant after 30 min and remained significant at 45 min (p<0.05). There was a group tendency for Rrs to fall following physiotherapy that was sustained after both 15 and 30 min (Table 2). This trend reached statistical significance (p<0.05) for infants on volume-preset ventilation but remained non-significant (p<0.09) for those on pressure-preset ventilation. There were no significant group changes in Rrs after suction, irrespective of ventilation mode (Table 3). There were no significant group or subgroup differences in pH, arterial carbon dioxide tension (PaCO2) or arterial oxygen tension (PaO2) following either physiotherapy or suction and no significant changes in standard bicarbonate (HCO3 −), base excess (BE) or SaO2 following suction alone. The statistically significant reductions in HCO3 −, BE and SaO2 after physiotherapy suggested a mild metabolic acidosis, although, as derivatives of pH, PaCO2 and PaO2, these values may have negligible clinical significance.
Comparison of treatments
Mean within-subject changes in VTE, Crs, Rrs and arterial blood gases following physiotherapy and suction were compared by t test analysis (Table 4). The difference in direction of change for VTE and Crs after physiotherapy and suction resulted in a tendency for paired differences to approach significance 15 min after treatment, and these reached significance after 30 min (p<0.05). By contrast, the reduction in Rrs following both treatments resulted in an insignificant difference between treatment modalities, although the magnitude of change in Rrs following physiotherapy was larger.
The reduction in HCO3 − after physiotherapy was confirmed to be a factor distinguishing physiotherapy from suction (Table 4). Differences between treatments for BE and SaO2 were smaller and approached significance for BE alone. No relationship between treatment and outcome could be demonstrated by multivariate analysis using length of treatment, experience of staff, patient diagnosis or age groups as co-variables.
Individual responses
Individual response to both physiotherapy and suction was variable. Changes in excess of the 95% LA were assumed to be important clinically. An apparent improvement (increase in VTE and Crs and reduction in Rrs) which exceeded the 95% LA (VTE ±5.5%, Crs ±7%, Rrs ±15%) was observed in approximately twice as many subjects following physiotherapy (VTE 27:13, Crs 24:14, Rrs 20:11), these differences being significant for VTE (p=0.01) and approaching significance for Crs and Rrs (p<0.06 and 0.07, respectively). Respiratory function deteriorated in up to one-third of participants after both treatments.
Both respiratory and cardiac groups included medical and surgical patients and 42% of patients had abnormal radiographic signs. However, scatter plots revealed no relationship between baseline values of Crs, Rrs or VTE or responses to therapy and surgical/medical management, radiographic changes, diagnosis or ventilation modality (data not shown).
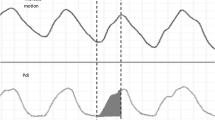
Baseline Rrs values ranged widely (10–276 cmH2O l−1 s−1), with the highest values seen in infants less than 6 months old and with Rrs falling predictably in older patients with larger airway calibre (Fig. 1). Concurrent in vitro analysis showed that the resistance generated by a 3-mm internal diameter tracheal tube at high flow (30l/min) was less than 100 cmH2O l−1 s−1. Thus even in the youngest infants, Rrs of less than 150 cmH2O l−1 s−1 was likely to reflect some pathological contribution to airway resistance (secretions, airway wall oedema or bronchospasm). Patients with high baseline Rrs values relative to their age were most likely to respond to physiotherapy with a fall in Rrs of more than 15% (Fig. 1a). This tendency was not noticeable following suction (Fig. 1b).
Plots of Crs and VTE against age with respect to treatment response (data not shown) demonstrated a wide range of baseline values (0.02 – 1.2 ml cmH2O−1 kg−1 and 3–17 ml kg−1, respectively) but neither showed any relationship between baseline values and changes following treatment.
The median baseline OI of participants with an arterial line was 4.1 (range 2.3–36.4). Scatter plot analysis revealed no relationship between OI and adverse events or response to treatment for either physiotherapy or suction.
The greatest individual changes in HCO3 − were −7 mmol/l after physiotherapy and 7 mmol/l after suction. With the exception of these two participants, individual changes in HCO3 − after treatment were less than 3 mmol/l. The largest individual change in base deficit was 5 following physiotherapy. Although SaO2 was more likely to fall following physiotherapy, changes greater than 5% after either treatment were rare. One exception was a 20% fall in SaO2 after suction.
Following both treatments 50% of participants had a change in PaO2 and 41% had changes in PaCO2 that exceeded twice the reported CV for these parameters in stable adult patients (6.1% and 4.7%, respectively) [18]. In approximately 70% of these individuals PaO2 decreased.
Discussion
Physiotherapy treatments differed from suction in two ways. First, physiotherapy involved the application of manual techniques and treatments were significantly longer, involved greater volumes of saline instillation and more suction catheters. Secondly, there was some evidence that physiotherapy treatments had small but statistically distinguishable effects on respiratory function. Results suggested that physiotherapy was more effective at reducing Rrs, presumably as a result of removing secretions, but also produced an increase in arterial blood gas markers for metabolic acidosis. In addition, physiotherapy was twice as likely to produce significant within-subject improvements in VTE, Crs and Rrs as suction alone. Suction was not accompanied by any statistically significant group changes in arterial blood gases or respiratory function parameters.
Group vs. individual changes
Physiotherapy and suction aim to prevent secretion retention as well as resolve acute clinical complications. Primarily preventative treatments may be important for the patient (their regular performance probably contributes to the rarity of life-threatening airway occlusion) but may not result in any measurable change in respiratory function. Conversely, treatment of acute lobar atelectasis may produce marked differences in respiratory function, but occurs infrequently. Such results may be obscured by simple analysis of group changes in response to treatment. Within-subject changes in respiratory function were therefore examined separately.
Individual responses to physiotherapy and suction were variable in both direction and magnitude and sometimes exceeded three times the 95% LA of normal variability for VTE, Rrs and Crs (i.e. ±6 SDs). Improvements in some individuals confirmed the potential benefit of respiratory therapies, whereas the absence of change amongst others probably reflected a large proportion of preventative treatments. However, the deterioration observed in up to one-third of participants exposed a need for sensitive treatment exclusion criteria. Multivariate analyses were unable to demonstrate predictive factors for improvement or deterioration on the basis of age, diagnosis, ventilation mode, staff experience or treatment details.
Previous studies
Few studies have examined the differences between respiratory physiotherapy treatment regimens and simple suction. One suggested that in acute lobar atelectasis positioning and vibrations improved the efficacy of hyperinflation and suction [19]. This concurred with studies confirming the benefits of physiotherapy for patients with atelectatic changes [19, 20, 21, 22, 23]. Other found no difference in incidence of infection or change in Crs between groups undergoing physiotherapy or suction [24, 25]. Thus while there is relatively strong evidence that acute atelectasis can rapidly be resolved with physiotherapy, there remain uncertainties about other clinical indications for treatment.
Respiratory compliance
Crs depends on tissue elasticity, lung water content, surfactant, and pulmonary blood flow and volume. Individual components of treatment may potentially influence any of the determinants of Crs differently. Adding manual hyperinflation to treatment, for example, can improve Crs [26, 27, 28], whereas suction can contribute to alveolar collapse and reduced Crs [29]. A tendency for VTE and Crs to decrease following treatment could thus reflect a technique in which suctioning (collapsing alveoli) has not been adequately compensated for by manual hyperinflation (recruiting alveoli).
Respiratory resistance
Rrs is dominated by the upper airways and in ventilated patients, the tracheal tube creates a non-linear resistance, dependent on flow entry effects, laminar or turbulent flow due to secretions, tube position and tube wall properties [30]. Response to treatment may be influenced by the length, position or relative size of the tracheal tube to the tracheal diameter as well as treatment technique [31, 32, 33, 34]. Acute changes in Rrs such as those observed after physiotherapy probably do not reflect changes in peripheral airway resistance, but the removal of secretions from upper airways.
Patients with high baseline Rrs relative to their age were most likely to respond to physiotherapy with a fall in Rrs greater than15% (>95% LA), while this tendency was not observed following suction. This result suggests some advantage of physiotherapy in clearing airway secretions, possibly because chest wall vibrations applied during expiration rapidly increase expiratory flow in a manner resembling a huff or cough, advancing secretions to the larger airways. Additionally, the frequency of applied chest wall vibrations or percussion, coupled with the turbulence of instilled saline may reduce both mucus viscosity and its adherence to the airway wall.
Arterial blood gases
The reduction in HCO3 −, BE and SaO2 observed after physiotherapy suggest a mild metabolic acidosis that may be related to an uncompensated increase in metabolic demand. The observed changes in HCO3 − and BE have not been reported previously but the drop in SaO2 concurs with previous studies [35, 36, 37]. Several studies have reported an increase in metabolic demand following physiotherapy, while others have described a significant reduction with sedation or pharmacological paralysis [38, 39, 40]. Since all participants in this study were sedated and paralysed, responses to the stress of physiotherapy may have been dampened.
A sustained reduction in PaO2 following physiotherapy or suction reported in previous studies was not confirmed in this study [33, 35, 37, 41]. This may reflect a successful unit policy of pre-oxygenation before treatment.
Study limitations
Data from in vivo studies suggested that 5 min would have been sufficient to acquire representative baseline data in stable, paralysed patients. The 15-min period selected was thus sufficient for recording baseline values and acute changes. Although monitoring was continued for longer than 30 min after treatment when feasible, it is possible that delayed changes were missed. Furthermore, outcomes such as VTE and Crs reflect the immediate clinical status of the patient, but may inaccurately represent the longer-term benefit achieved by removal of secretions. Both the study design and outcome measures chosen may thus have been insensitive to the overall effect of treatment.
Future studies
This study compared the effects of different treatment regimens. There remains a great deal of variability in the delivery of physiotherapy techniques. The next step in understanding individual responses to physiotherapy may be in quantification and detailed analysis of the force and pressure profiles delivered to the chest wall during manual vibration or percussion and the resultant changes in flow at the airway opening [42]. Further information is required about the magnitude and duration of effects and whether detrimental consequences can be minimised by appropriate patient selection.
Conclusions
The majority of intubated children require regular airway clearance to prevent pulmonary morbidity, especially when sedated or pharmacologically paralysed. This study demonstrated that while physiotherapy treatments take longer and involve more saline instillation and suction catheters than suction, they appear to have an advantage in reducing Rrs, that reached significance in the 22 patients on volume-preset ventilation. Physiotherapy, however, also produced small reductions in HCO3 −, BE and SaO2, the clinical importance of which is unclear. The advantages conferred by physiotherapy in removing secretions may be of substantial benefit in patients with evidence of acute atelectasis, while the low physiological cost of suction alone may offer a relatively benign but important routine intervention for ensuring airway patency.
Within individuals, physiotherapy treatments were more likely to produce improvements in VTE, Crs and Rrs than suction alone, but both treatments induced an immediate deterioration in almost a third of subjects. Further research should attempt to identify sensitive tools for selection of patients likely to benefit from physiotherapy and and assess longer term effects.
Reference
Kim WD (1997) Lung mucus: a clinician’s view. Eur Respir J 10:1914–1917
Ciesla ND (1996) Chest physical therapy for patients in the intensive care unit. Phys Ther 76:609–625
Hammer J, Newth CJ (1995) Infant lung function testing in the intensive care unit. Intensive Care Med 21:744–752
Main E, Stocks J (2004) The influence of physiotherapy and suction on respiratory deadspace in ventilated children. Intensive Care Med (http://dx.doi.org/10.1007/s00134-004-2261-1)
Stiller K (2000) Physiotherapy in intensive care: towards an evidence-based practice. Chest 118:1801–1813
Conti G, Vilardi V, Rocco M, DeBlasi RA, Lappa A, Bufi M, Antonelli M, Gasparetto A (1995) Paralysis has no effect on chest wall and respiratory system mechanics of mechanically ventilated, sedated patients. Intensive Care Med 21:808–812
Iotti GA, Braschi A, Brunner JX, Smits T, Olivei M, Palo A, Veronesi R (1995) Respiratory mechanics by least squares fitting in mechanically ventilated patients: applications during paralysis and during pressure support ventilation. Intensive Care Med 21:406–413
Sediame S, Zerah-Lancner F, d’Ortho MP, Adnot S, Harf A (1999) Accuracy of the i-STAT bedside blood gas analyser. Eur Respir J 14:214–217
Cannon ML, Cornell J, Tripp-Hamel DS, Gentile MA, Hubble CL, Meliones JN, Cheifetz IM (2000) Tidal volumes for ventilated infants should be determined with a pneumotachometer placed at the endotracheal tube. Am J Respir Crit Care Med 162:2109–2112
Kuo CY, Gerhardt T, Bolivar J, Claure N, Bancalari E (1996) Effect of leak around the endotracheal tube on measurements of pulmonary compliance and resistance during mechanical ventilation: a lung model study. Pediatr Pulmonol 22:35–43
Main E, Castle R, Stocks J, James I, Hatch D (2001) The influence of endotracheal tube leak on the assessment of respiratory function in ventilated children. Intensive Care Med 27:1788–1797
Frey U, Stocks J, Coates A, Sly P, Bates J (2000) Specifications for equipment used for infant pulmonary function testing. ERS/ATS Task Force on Standards for Infant Respiratory Function Testing. European Respiratory Society/ American Thoracic Society. Eur Respir J 16:731–740
Hjalmarson O (1994) Lung function testing—useless in ventilated newborns? Eur J Pediatr 153:S22–S26
Main E, Elliott MJ, Schindler M, Stocks J (2001) Effect of delayed sternal closure after cardiac surgery on respiratory function in ventilated infants. Critical Care Med 29:1798–1802
Kondo T, Matsumoto I, Lanteri CJ, Sly PD (1997) Respiratory mechanics during mechanical ventilation: a model study on the effects of leak around a tracheal tube. Pediatr Pulmonol 24:423–428
Bland JM, Altman DG (1999) Measuring agreement in method comparison studies. Stat Methods Med Res 8:135–160
Lagerstrand L, Ingemansson M, Bergstrom SE, Lidberg K, Hedlin G (2002) Tidal volume forced expiration in asthmatic infants: reproducibility and reversibility tests. Respiration 69:389–396
Sasse SA, Chen PA, Mahutte CK (1994) Variability of arterial blood gas values over time in stable medical ICU patients. Chest 106:187–193
Stiller K, Geake T, Taylor J, Grant R, Hall B (1990) Acute lobar atelectasis. A comparison of two chest physiotherapy regimens. Chest 98:1336–1340
Marini JJ, Pierson DJ, Hudson LD (1979) Acute lobar atelectasis: a prospective comparison of fiberoptic bronchoscopy and respiratory therapy. Am Rev Respir Dis 119:971–978
Fourrier F, Fourrier L, Lestavel P (1994) Acute lobar atelectasis in ICU patients: comparative randomized study of fibroptic bronchoscopy versus respiratory therapy. Intensive Care Med 20:s40
Stiller K, Jenkins S, Grant R, Geake T, Taylor J, Hall B (1996) Acute lobar atelectasis: a comparison of five physiotherapy regimens. Physiother Theo Pract 12:197–209
Galvis AG, Reyes G, Nelson WB (1994) Bedside management of lung collapse in children on mechanical ventilation: saline lavage-simulated cough technique proves simple, effective. Pediatr Pulmonol 17:326–330
Ntoumenopoulos G, Gild A, Cooper DJ (1998) The effect of manual lung hyperinflation and postural drainage on pulmonary complications in mechanically ventilated trauma patients. Anaesth Intensive Care 26:492–496
Eales CJ, Barker M, Cubberley NJ (1995) Evaluation of a single chest physiotherapy treatment to post-operative, mechanically ventilated cardiac surgery patients. Physiother Theo Pract 11:23–38
Jones AY, Hutchinson RC, Oh TE (1992) Effects of bagging and percussion on total static compliance of the respiratory system. Physiotherapy 78:661–666
Hodgson C, Denehy L, Ntoumenopoulos G, Santamaria J, Carroll S (2000) An investigation of the early effects of manual lung hyperinflation in critically ill patients. Anaesth Intensive Care 28:255–261
Macnaughton PD (1997) Assessment of lung function in the ventilated patient. Intensive Care Med 23:810–818
Brandstater B, Muallem M (1969) Atelectasis following tracheal suction in infants. Anesthesiology 31:468–473
Sly PD, Lanteri C, Nicolai T (1996) Measurement of Respiratory Function in the Intensive Care Unit. In: Stocks J, Sly PD, Tepper RS, Morgan WJ (eds) Infant respiratory function testing. Wiley, New York, pp 445–484
Mackenzie CF, Shin B (1985) Cardiorespiratory function before and after chest physiotherapy in mechanically ventilated patients with post-traumatic respiratory failure. Crit Care Med 13:483–486
Prendiville A, Thomson A, Silverman M (1986) Effect of tracheobronchial suction on respiratory resistance in intubated preterm babies. Arch Dis Child 61:1178–1183
Fox WW, Schwartz JG, Shaffer TH (1978) Pulmonary physiotherapy in neonates: physiologic changes and respiratory management. J Pediatr 92:977–981
Cochrane GM, Webber BA, Clarke SW (1977) Effects of sputum on pulmonary function. BMJ 2:1181–1183
Simbruner G, Coradello H, Fodor M, Havelec L, Lubec G, Pollak A (1981) Effect of tracheal suction on oxygenation, circulation, and lung mechanics in newborn infants. Arch Dis Child 56:326–330
Kerem E, Yatsiv I, Goitein KJ (1990) Effect of endotracheal suctioning on arterial blood gases in children. Intensive Care Med 16:95–99
Hussey JM (1992) Effects of chest physiotherapy for children in intensive care after surgery. Physiotherapy 78:109–113
Harding J, Kemper M, Weissman C (1994) Midazolam attenuates the metabolic and cardiopulmonary responses to an acute increase in oxygen demand. Chest 106:194–200
Cohen D, Horiuchi K, Kemper M, Weissman C (1996) Modulating effects of propofol on metabolic and cardiopulmonary responses to stressful intensive care unit procedures. Crit Care Med 24:612–617
Horiuchi K, Jordan D, Cohen D, Kemper MC, Weissman C (1997) Insights into the increased oxygen demand during chest physiotherapy. Crit Care Med 25:1347–1351
Gormezano J, Branthwaite MA (1972) Effects of physiotherapy during intermittent positive pressure ventilation. Changes in arterial blood gas tensions. Anaesthesia 27:258–264
Gregson RK, Petley GW, Browne M, Pickering RM, Warner JO (2003) A new method to quantify manual chest physiotherapy techniques. Physiotherapy 289:611–612
Acknowledgements
We thank Prof. Linda Franck for advice during preparation of the manuscript. This work was undertaken by Great Ormond Street Hospital for Children NHS Trust which received a proportion of its funding from the NHS Executive; the views expressed in this publication are those of the authors and are not necessarily those of the NHS Executive.
Author information
Authors and Affiliations
Corresponding author
Additional information
Janet Stocks and Rosemary Castle are supported by Portex PLC.
An editorial regarding this article can be found at http://dx.doi.org/10.1007/s00134-004-2216-6
Electronic Supplementary Material
Rights and permissions
About this article
Cite this article
Main, E., Castle, R., Newham, D. et al. Respiratory physiotherapy vs. suction: the effects on respiratory function in ventilated infants and children. Intensive Care Med 30, 1144–1151 (2004). https://doi.org/10.1007/s00134-004-2262-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-004-2262-0