Abstract
Purpose
Mental illness represents a major public health burden among Canada’s large immigrant population. A burgeoning cross-sectional, longitudinal, and experimental evidence base implicates nutrition in mental health. Healthier diets (e.g., those rich in certain micro-nutrients) may benefit cognitive, social, and emotional functioning through attenuated inflammation and other bio-psychological pathways. The present study examined associations between nutrition and three markers of mental health among immigrants to Canada.
Methods
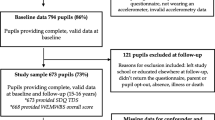
Employing cross-sectional data from immigrant respondents (n = 37,071) to a nationally representative population-based survey (the Canadian Community Health Survey: CCHS 2011–2014), we modelled associations of daily fruit and vegetable consumption with three mental health outcomes: anxiety and/or mood disorder diagnosis, being distressed (assessed via the 6-item Kessler Psychological Distress Scale), and having good self-rated overall mental health. Multivariable logistic regression analyses were employed, adjusting for various socio-demographic and lifestyle-related variables.
Results
Higher consumption of fruit and vegetables demonstrated significant, protective associations with odds of having a mood and/or anxiety disorder, being distressed, and self-rated good mental health. Such patterns of association were similar regardless of ethno-cultural minority status and recency of immigration. Moreover, the protective associations of nutrition and mental health were independent of socio-demographic, health, and lifestyle factors.
Conclusions
Results suggested evidence of protective associations between healthy nutritional intake and mental illness among a large-scale sample of immigrants in Canada. Importantly, the protective associations of healthier diets with immigrants’ mental health were independent of various markers of healthy lifestyles (e.g., general health status, physical activity, alcohol use). Healthy dietary intake may, therefore, be worth consideration in efforts to prevent mental illness among immigrants.
Similar content being viewed by others
References
Statistics Canada (2017) Immigration and ethnocultural diversity: key results from the 2016 Census. Retrieved from https://www150.statcan.gc.ca/n1/en/daily-quotidien/171025/dq171025b-eng.pdf?st=Hib3Z2wR
Statistics Canada (2017) Children with an immigrant background: bridging cultures. Retrieved from https://www12.statcan.gc.ca/census-recensement/2016/as-sa/98-200-x/2016015/98-200-x2016015-eng.pdf
Gushulak BD, Pottie K, Roberts JH, Torres S, DesMeules M (2011) Migration and health in Canada: health in the global village. CMAJ 183(12):E952–E958. https://doi.org/10.1503/cmaj.090287
Vigo D, Thornicroft G, Atun R (2016) Estimating the true global burden of mental illness. Lancet Psychiatry 3(2):171–178
Pearson C, Janz T, Ali J (2013) Mental and substance use disorders in Canada. Statistics Canada, Ottawa. Retrieved from https://www150.statcan.gc.ca/n1/pub/82-624-x/2013001/article/11855-eng.htm
Quan H, Fong A, De Coster C, Wang J, Musto R, Noseworthy TW et al (2006) Variation in health services utilization among ethnic populations. Can Med Assoc J 174(6):787–791
Chaze F, Thomson MS, George U, Guruge S (2015) Role of cultural beliefs, religion, and spirituality in mental health and/or service utilization among immigrants in Canada: a scoping review. Can J Commun Mental Health 34(3):87–101
Castañeda H, Holmes SM, Madrigal DS, Young M-ED, Beyeler N, Quesada J (2015) Immigration as a social determinant of health. Ann Rev Public Health 36:375–392
George U, Thomson MS, Chaze F, Guruge S (2015) Immigrant mental health, a public health issue: looking back and moving forward. Int J Environ Res Public Health 12(10):13624–13648
Chekroud SR, Gueorguieva R, Zheutlin AB, Paulus M, Krumholz HM, Krystal JH et al (2018) Association between physical exercise and mental health in 1· 2 million individuals in the USA between 2011 and 2015: a cross-sectional study. Lancet Psychiatry 5(9):739–746
Van Duyn MAS, Pivonka E (2000) Overview of the health benefits of fruit and vegetable consumption for the dietetics professional: selected literature. J Am Diet Assoc 100(12):1511–1521
Lock K, Pomerleau J, Causer L, Altmann DR, McKee M (2005) The global burden of disease attributable to low consumption of fruit and vegetables: implications for the global strategy on diet. Bull World Health Organ 83(2):100–108
Sarris J, Logan AC, Akbaraly TN, Amminger GP, Balanzá-Martínez V, Freeman MP et al (2015) Nutritional medicine as mainstream in psychiatry. Lancet Psychiatry 2(3):271–274
Oriach CS, Robertson RC, Stanton C, Cryan JF, Dinan TG (2016) Food for thought: the role of nutrition in the microbiota-gut–brain axis. Clin Nutr Exp 6:25–38
Berk M, Williams LJ, Jacka FN, O’Neil A, Pasco JA, Moylan S et al (2013) So depression is an inflammatory disease, but where does the inflammation come from? BMC Med 11(1):200
Kaplan BJ, Rucklidge JJ, Romijn A, McLeod K (2015) The emerging field of nutritional mental health: inflammation, the microbiome, oxidative stress, and mitochondrial function. Clin Psychol Sci 3(6):964–980
Sarris J, Logan AC, Akbaraly TN, Amminger P, Balanzá-Martínez G, Freeman VMP et al (2015) International Society for Nutritional Psychiatry Research consensus position statement: nutritional medicine in modern psychiatry. World Psychiatry 14(3):370–371
Sarris J, Mischoulon D, Schweitzer I (2011) Adjunctive nutraceuticals with standard pharmacotherapies in bipolar disorder: a systematic review of clinical trials. Bipolar Disord 13(5-6):454–465
Kean JD, Camfield D, Sarris J, Kras M, Silberstein R, Scholey A et al (2013) A randomized controlled trial investigating the effects of PCSO-524®, a patented oil extract of the New Zealand green lipped mussel (Perna canaliculus), on the behaviour, mood, cognition and neurophysiology of children and adolescents (aged 6–14 years) experiencing clinical and sub-clinical levels of hyperactivity and inattention: study protocol ACTRN12610000978066. Nutr J 12(1):100
McMartin SE, Jacka FN, Colman I (2013) The association between fruit and vegetable consumption and mental health disorders: evidence from five waves of a national survey of Canadians. Prev Med 56(3–4):225–230
Jacka FN, Cherbuin N, Anstey KJ, Sachdev P, Butterworth P (2015) Western diet is associated with a smaller hippocampus: a longitudinal investigation. BMC Med 13(1):215
Kingsbury M, Dupuis G, Jacka F, Roy-Gagnon M-H, McMartin SE, Colman I (2015) Associations between fruit and vegetable consumption and depressive symptoms: evidence from a national Canadian longitudinal survey. J Epidemiol Commun Health 70(2):155–161
Jacka FN, O’Neil A, Opie R, Itsiopoulos C, Cotton S, Mohebbi M et al (2017) A randomised controlled trial of dietary improvement for adults with major depression (the ‘SMILES’trial). BMC Med 15(1):23
Parletta N, Zarnowiecki D, Cho J, Wilson A, Bogomolova S, Villani A et al (2017) A Mediterranean-style dietary intervention supplemented with fish oil improves diet quality and mental health in people with depression: a randomized controlled trial (HELFIMED). Nutr Neurosci. https://doi.org/10.1080/1028415X.2017.1411320
Li Y, Lv M-R, Wei Y-J, Sun L, Zhang J-X, Zhang H-G et al (2017) Dietary patterns and depression risk: a meta-analysis. Psychiatry Res 253:373–382
Lai JS, Hiles S, Bisquera A, Hure AJ, McEvoy M, Attia J (2013) A systematic review and meta-analysis of dietary patterns and depression in community-dwelling adults. Am J Clin Nutr 99(1):181–197
Sanou D, O’Reilly E, Ngnie-Teta I, Batal M, Mondain N, Andrew C et al (2014) Acculturation and nutritional health of immigrants in Canada: a scoping review. J Immigr Minor Health 16(1):24–34
Statistics Canada (2012) Canadian Community Health Survey: Annual component. Retrieved from http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&Id=135927
Statistics Canada (2014) Canadian Community Health Survey: Annual component. Retrived from http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&Id=164081
Centres for Disease Control (2011) Behavioural Risk Factor Surveillance System Questionnaire. US Department of Health and Human Services. Centers for Disease Control and Prevention. Atlanta, Georgia
Kulkarni A, Swinburn B, Utter J (2015) Associations between diet quality and mental health in socially disadvantaged New Zealand adolescents. Eur J Clin Nutr 69(1):79
Garriguet D (2009) Diet quality in Canada. Health Rep 20(3):41
Pérez CE (2002) Fruit and vegetable consumption. Health Rep 13(3):23–31
O’Donnell S, Vanderloo S, McRae L, Onysko J, Patten S, Pelletier L (2016) Comparison of the estimated prevalence of mood and/or anxiety disorders in Canada between self-report and administrative data. Epidemiol Psychiatric Sci 25(4):360–369
Cairney J, Veldhuizen S, Wade TJ, Kurdyak P, Streiner DL (2007) Evaluation of 2 measures of psychological distress as screeners for depression in the general population. Can J Psychiatry 52(2):111–120. https://doi.org/10.1177/070674370705200209
Ahmad F, Jhajj AK, Stewart DE, Burghardt M, Bierman AS (2014) Single item measures of self-rated mental health: a scoping review. BMC Health Serv Res 14(1):398
Statistics Canada (2011) Canadian Community Health Survey (CCHS) Derived Variable (DV) Specifications. Ottawa, ON
SAS Institute Inc (2018) SAS software (version 14, University Edition)
The University of British Columbia Broad of Governors (2012) Policy #89: Research Involving Human Participants
Pan SW, Carpiano RM (2013) Immigrant density, sense of community belonging, and suicidal ideation among racial minority and white immigrants in Canada. J Immigr Minor Health 15(1):34–42
Psaltopoulou T, Sergentanis TN, Panagiotakos DB, Sergentanis IN, Kosti R, Scarmeas N (2013) Mediterranean diet, stroke, cognitive impairment, and depression: a meta-analysis. Ann Neurol 74(4):580–591
Bauer IE, Gálvez JF, Hamilton JE, Balanzá-Martínez V, Zunta-Soares GB, Soares JC et al (2016) Lifestyle interventions targeting dietary habits and exercise in bipolar disorder: a systematic review. J Psychiatric Res 74:1–7
Firth J, Stubbs B, Sarris J, Rosenbaum S, Teasdale S, Berk M et al (2017) The effects of vitamin and mineral supplementation on symptoms of schizophrenia: a systematic review and meta-analysis. Psychol Med 47(9):1515–1527
Gordon HA, Rucklidge JJ, Blampied NM, Johnstone JM (2015) Clinically significant symptom reduction in children with attention-deficit/hyperactivity disorder treated with micronutrients: an open-label reversal design study. J Child Adolesc Psychopharmacol 25(10):783–798
Christensen L (2001) The effect of food intake on mood. Clin Nutr 20:161–166
Jacka FN, Cherbuin N, Anstey KJ, Butterworth P (2015) Does reverse causality explain the relationship between diet and depression? J Affect Disord 175:248–250
Berry JW, Hou F (2016) Immigrant acculturation and wellbeing in Canada. Can Psychol/Psychologie canadienne 57(4):254–264
Chiu M, Amartey A, Wang X, Kurdyak P (2018) Ethnic differences in mental health status and service utilization: a population-based study in Ontario, Canada. Can J Psychiatry 63(7):481–491
Furukawa TA, Kessler RC, Slade T, Andrews G (2003) The performance of the K6 and K10 screening scales for psychological distress in the Australian National Survey of Mental Health and Well-Being. Psychol Med 33(2):357–362
Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E et al (2003) Screening for serious mental illness in the general population. Arch Gen Psychiatry 60(2):184–189
Walsh R (2011) Lifestyle and mental health. Am Psychol 66(7):579
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical considerations
The authors declare no conflicts of interest. This study contains secondary data analysis of publicly available data from the Canadian Community Health Survey.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Emerson, S.D., Carbert, N.S. An apple a day: Protective associations between nutrition and the mental health of immigrants in Canada. Soc Psychiatry Psychiatr Epidemiol 54, 567–578 (2019). https://doi.org/10.1007/s00127-018-1616-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-018-1616-9