Abstract
Aims/hypothesis
Non-albuminuric renal impairment has become the prevailing diabetic kidney disease (DKD) phenotype in individuals with type 2 diabetes and an estimated GFR (eGFR) <60 ml min−1 1.73 m−2. In the present study, we compared the rate and determinants of all-cause death in individuals with this phenotype with those in individuals with albuminuric phenotypes.
Methods
This observational prospective cohort study enrolled 15,773 individuals with type 2 diabetes in 2006–2008. Based on baseline albuminuria and eGFR, individuals were classified as having: no DKD (Alb−/eGFR−), albuminuria alone (Alb+/eGFR−), reduced eGFR alone (Alb−/eGFR+), or both albuminuria and reduced eGFR (Alb+/eGFR+). Vital status on 31 October 2015 was retrieved for 15,656 individuals (99.26%).
Results
Mortality risk adjusted for confounders was lowest for Alb−/eGFR− (reference category) and highest for Alb+/eGFR+ (HR 2.08 [95% CI 1.88, 2.30]), with similar values for Alb+/eGFR− (1.45 [1.33, 1.58]) and Alb−/eGFR+ (1.58 [1.43, 1.75]). Similar results were obtained when individuals were stratified by sex, age (except in the lowest age category) and prior cardiovascular disease. In normoalbuminuric individuals with eGFR <45 ml min−1 1.73 m−2, especially with low albuminuria (10–29 mg/day), risk was higher than in microalbuminuric and similar to macroalbuminuric individuals with preserved eGFR. Using recursive partitioning and amalgamation analysis, prevalent cardiovascular disease and lower HDL-cholesterol were the most relevant correlates of mortality in all phenotypes. Higher albuminuria within the normoalbuminuric range was associated with death in non-albuminuric DKD, whereas the classic ‘microvascular signatures’, such as glycaemic exposure and retinopathy, were correlates of mortality only in individuals with albuminuric phenotypes.
Conclusions/interpretation
Non-albuminuric renal impairment is a strong predictor of mortality, thus supporting a major prognostic impact of renal dysfunction irrespective of albuminuria. Correlates of death partly differ from the albuminuric forms, indicating that non-albuminuric DKD is a distinct phenotype.
Trial registration:
ClinicalTrials.gov NCT00715481
Similar content being viewed by others

Introduction
Recent data from the Third National Health and Nutrition Examination Survey (NHANES III) have indicated that prevalence of diabetic kidney disease (DKD) among people with diabetes has remained stable during the last decades [1], though the prevalence of reduced estimated GFR (eGFR) has increased, whereas that of albuminuria has decreased [2]. These opposite trends in the two main DKD manifestations reflect changes that have occurred in the natural history of DKD, which, in many individuals, does not recapitulate the classic five-stage course [3].
In particular, the paradigm that eGFR loss starts after macroalbuminuria has developed has been recently challenged [4, 5]. A cross-sectional analysis of the NHANES III 1988–1994 data revealed that 36.1% of diabetic individuals with reduced eGFR (i.e. <60 ml min−1 1.73 m−2) were normoalbuminuric [6]. More recently, both longitudinal and cross-sectional studies have demonstrated that non-albuminuric renal impairment has become the prevailing DKD phenotype in individuals with type 2 diabetes and reduced eGFR [7,8,9,10,11], and it is also frequently observed in individuals with type 1 diabetes [12,13,14].
Diabetes is associated with excess mortality mainly, but not exclusively, from cardiovascular disease (CVD) [15]. The NHANES III 1988–2000 data show that both increased albuminuria and reduced eGFR are independently associated with all-cause and CVD mortality [16]. These findings were confirmed by large meta-analyses from the general population [17, 18], high-CVD-risk cohorts (including diabetic individuals) [18] and chronic kidney disease (CKD) cohorts [18, 19], which also reported an increase in mortality for individuals with reduced eGFR values in the absence of albuminuria [17, 18]. Studies in type 1 [13] and type 2 [9, 10, 20, 21] diabetes also showed that albuminuria and reduced eGFR are independently associated with mortality and CVD and renal events, though they provide conflicting estimates of outcome rates associated with the non-albuminuric phenotype vs the albuminuric ones.
This study specifically assessed the rate and determinants of all-cause mortality in individuals with type 2 diabetes and non-albuminuric renal impairment compared with the albuminuric phenotypes, i.e., albuminuria with preserved or reduced eGFR.
Methods
The Renal Insufficiency And Cardiovascular Events (RIACE) Italian multicentre study is an observational prospective cohort study of the impact of eGFR on morbidity and mortality in individuals with type 2 diabetes [11]. The study was conducted in accordance with the Declaration of Helsinki. The study protocol was approved by the locally appointed ethics committees and participants gave informed consent.
Participants
The RIACE population consists of 15,773 white individuals with type 2 diabetes (after excluding 160 individuals with missing or implausible values), consecutively visiting 19 hospital-based tertiary referral diabetes clinics of the National Health Service throughout Italy (see electronic supplementary material [ESM]) in the years 2006–2008. Exclusion criteria were dialysis or renal transplantation.
The vital status of study participants on 31 October 2015 was verified by interrogating the Italian Health Card database (http://sistemats1.sanita.finanze.it/wps/portal/), which provides updated information on all current Italian residents [22].
Measurements
At baseline, anamnestic, clinical and laboratory data were obtained from all individuals using a standardised protocol across study centres [11].
Study participants underwent a structured interview to collect the following information: age, smoking status, known diabetes duration, comorbidities and current glucose-, lipid- and BP-lowering therapy.
BMI was calculated from weight and height and BP was then measured with a sphygmomanometer. Estimated waist circumference (eWC) was calculated from log-transformed BMI values using sex-specific linear regression equations derived from waist measurements obtained in 4618 individuals [23].
HbA1c was measured by high-performance liquid chromatography using DCCT-aligned methods; triacylglycerols, total cholesterol and HDL-cholesterol were determined in fasting blood samples by colorimetric enzymatic methods; non-HDL-cholesterol was calculated by the formula: total cholesterol – HDL-cholesterol; and LDL-cholesterol was calculated using the Friedewald formula.
Presence of DKD was assessed by measuring albuminuria and serum creatinine. As previously detailed [11, 24], AER was measured from 24 h urine collections (measured AER [mAER]) or estimated from albumin-to-creatinine ratio (ACR) in early-morning first-voided urine samples, using a conversion formula developed in individuals with type 1 diabetes (estimated AER [eAER]) [25], in keeping with a recent report that eAER is more accurate than ACR in predicting mAER [26]. Albuminuria was measured in fresh urine samples by immunonephelometry or immunoturbidimetry. For each individual, 1–3 measurements were obtained; in cases of multiple measurements, the geometric mean was used for analysis. In individuals with multiple measurements, the concordance rate between the first value and the geometric mean was >90% for all albuminuria categories [24].
Individuals were assigned to one of the following categories of albuminuria (mg/day): normoalbuminuria (A1, AER <30); microalbuminuria (A2, AER 30-299); or macroalbuminuria (A3, AER ≥300). Normoalbuminuric individuals were further divided in those with normal (A1a, AER <10) and low (A1b, 10–29) albuminuria [27]. Serum (and urine) creatinine was measured by the modified Jaffe method, traceable to isotope dilution mass spectrometry, and eGFR was calculated by the CKD Epidemiology Collaboration equation [28]. Individuals were assigned to one of the following categories of eGFR (ml min−1 1.73 m−2): G1 (≥90); G2 (60–89); G3a (45–59); G3b (30–44); G4 (15–29); and G5 (<15). The G2 category was further divided into G2a (75–89) and G2b (60–74), whereas G4 and G5 were pooled (G4–5).
Based on albuminuria and eGFR, individuals were classified into the following DKD phenotypes [11]: no DKD (i.e. G1A1, G2A1); albuminuria alone (albuminuric DKD with preserved eGFR, i.e. G1A2, G2A2, G1A3, G2A3); reduced eGFR alone (non-albuminuric DKD, i.e. G3A1, G4A1, G5A1); or albuminuria and reduced eGFR (albuminuric DKD with reduced eGFR, i.e. G3A2, G4A2, G5A2, G3A3, G4A3, G5A3). The classification of individuals into albuminuria categories (ESM Table 1) and DKD phenotypes (ESM Table 2) differed only slightly using eAER vs ACR values.
In each centre, the presence of diabetic retinopathy was evaluated by an expert ophthalmologist using dilated fundoscopy. Individuals with mild or moderate non-proliferative diabetic retinopathy were classified as having non-advanced diabetic retinopathy, whereas those with severe non-proliferative diabetic retinopathy, proliferative diabetic retinopathy or maculopathy were grouped into the advanced diabetic retinopathy category. Diabetic retinopathy grade was assigned based on the worst eye [29].
Previous major acute CVD events, including myocardial infarction, stroke, foot ulcer/gangrene/amputation and coronary, carotid and lower limb revascularisation, were adjudicated based on hospital discharge records by an ad hoc committee in each centre [30].
Statistical analysis
Data are expressed as mean (SD) or median (interquartile range) for continuous variables, and number of cases (percentage) for categorical variables. Continuous variables were compared using one-way ANOVA or the non-parametric Kruskal–Wallis test. The χ2 test was applied to categorical variables.
Crude mortality rates were described as events per 1000 person-years, with 95% Poisson CIs. Death rates were also adjusted for age and eventually for sex by a Poisson regression model. Kaplan–Meier survival probabilities for all-cause mortality were estimated according to DKD phenotypes and Kidney Disease: Improving Global Outcomes (KDIGO) risk categories/subcategories. Differences were analysed with the logrank statistic. HRs and their 95% CIs according to DKD phenotypes and KDIGO risk categories/subcategories were estimated by Cox proportional hazards regression, adjusted for baseline age (model 1) or by CVD risk factors and complications/comorbidities, i.e. age, sex, smoking status, diabetes duration, HbA1c, BMI, eWC, triacylglycerols, total cholesterol and HDL-cholesterol, lipid-lowering treatment, systolic and diastolic BP, anti-hypertensive treatment, diabetic retinopathy grade, any CVD and any cancer (model 2).
The recursive partitioning and amalgamation (RECPAM) method, which combines the advantages of standard Cox regression and tree-growing techniques, was used to evaluate interactions among covariates and identify homogeneous subgroups with distinct mortality risks within each DKD phenotype [31]. The set of variables entered in the algorithm was the same of the Cox regression, except for LDL-cholesterol in place of total cholesterol. Age was introduced as a global variable and categorisation of values for continuous variables was omitted to allow algorithm-based selection of the natural cut-off points. Kaplan–Meier survival probabilities were estimated according to the RECPAM final subgroups.
Tests were two sided, and a p value <0.05 was considered statistically significant. Statistical analyses were performed using SPSS version 21.0 (SPSS, Chicago, IL, USA) and SAS Software Release 9.4 (SAS Institute, Cary, NC, USA).
Results
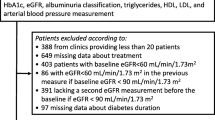
As reported in a recent analysis of the RIACE cohort assessing the overall contribution of DKD to excess mortality in individuals with type 2 diabetes [22], valid information on vital status was retrieved for 15,656 participants (99.3% of the original cohort, see Table 1 for baseline clinical characteristics). The prevalence of DKD phenotypes was 63.8% for no DKD, 18.9% for albuminuric DKD with preserved eGFR (16.6% with microalbuminuria and 2.3% with macroalbuminuria), 9.4% for non-albuminuric DKD and 7.9% for albuminuric DKD with reduced eGFR (5.5% with microalbuminuria and 2.3% with macroalbuminuria). Therefore, of individuals with reduced eGFR, the majority (54.6%) were normoalbuminuric. As previously reported [11], individuals with the non-albuminuric phenotype were more frequently women and never smokers and had lower HbA1c, systolic BP and diabetic retinopathy prevalence than those with albuminuric DKD with either preserved or reduced eGFR. In addition, they were older than participants with albuminuric DKD with preserved eGFR, but not compared with albuminuric DKD with reduced eGFR (Table 1).
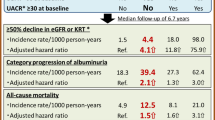
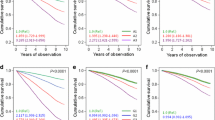
At the time of the census, 12,054 (77.0%) patients were alive, whereas 3602 (23.0%) individuals had died; the death rate was 31.0 per 1000 person-years (95% CI 30.0, 32.0) over a mean follow-up of 7.4 ± 2.1 years [22]. Crude mortality rates (Table 2) and Kaplan–Meier estimates (Fig. 1a) were lowest for no DKD and highest for albuminuric DKD with reduced eGFR, with a higher death rate for non-albuminuric DKD than for albuminuric DKD with preserved eGFR. However, the age-adjusted mortality rates for albuminuric DKD with reduced eGFR and non-albuminuric DKD were similar (Table 2), as were those adjusted for age and sex (29.98 vs 31.55 per 1000 person-years). At Cox regression adjusted for age (Fig. 1b) and multiple confounders (Fig. 1c), the HRs were similar for albuminuric DKD with preserved eGFR and non-albuminuric DKD, and lower for both than for albuminuric DKD with reduced eGFR. Other independent correlates of death were age, male sex, smoking, HbA1c, total cholesterol and HDL-cholesterol, lipid-lowering and anti-hypertensive treatment, diabetic retinopathy, CVD and cancer (ESM Table 3). The results were virtually identical when using ACR instead of eAER values (ESM Table 3 and ESM Fig. 1).
Cumulative survival by Kaplan–Meier analysis (a) and Cox proportional hazards regression, adjusted for age (b) and multiple confounders (c), according to DKD phenotype. Percentages for death (a) or HRs (95% CI) for mortality (b, c) are shown for each phenotype; p < 0.0001 across the phenotypes by logrank statistic (a) and Cox proportional hazards regression (b, c). Green, Alb−/eGFR− (no DKD); blue, Alb+/eGFR− (albuminuric DKD with preserved eGFR); red, Alb−/eGFR+ (non-albuminuric DKD); purple, Alb+/eGFR+ (albuminuric DKD with reduced eGFR). Ref, reference
Also, when individuals were stratified by sex (ESM Fig. 2 and ESM Table 4), age category (ESM Fig. 3 and ESM Table 4) and prior CVD (Fig. 2), the HRs were similar for albuminuric DKD with preserved eGFR and non-albuminuric DKD, except in participants aged <55 years. In this age category, individuals with non-albuminuric DKD showed the highest mortality risk; however, there were only 22 participants in this category and their adjusted HR was significantly higher than that of participants with albuminuria alone (n = 396) (p < 0.001), but not of those with both alterations (n = 55) (p = 0.344). Independent correlates of death were similar between men and women and individuals with and without CVD, except for HDL-cholesterol, which was associated with mortality only in women and participants without CVD (not shown).
Survival analysis by Cox proportional hazards regression, adjusted for age (a,c) and multiple confounders (b, d), according to DKD phenotype and the presence (a, b) or absence (c, d) of prior CVD. HRs for mortality are shown for each phenotype; p < 0.0001 across the phenotypes in each graph and p = 0.734 for interaction between DKD phenotypes and presence or absence of CVD by Cox proportional hazards regression. Green, Alb−/eGFR− (no DKD); blue, Alb+/eGFR− (albuminuric DKD with preserved eGFR); red, Alb−/eGFR+ (non-albuminuric DKD); purple, Alb+/eGFR+ (albuminuric DKD with reduced eGFR). Ref, reference
Crude mortality rates increased with increasing albuminuria and decreasing eGFR KDIGO categories (except between G2a and G2b) (Table 2). In the adjusted Cox regression analysis, normoalbuminuric individuals with an eGFR 45–59 ml min−1 1.73 m−2 (G3aA1a and b) had similar HRs (1.32 and 1.39, respectively), whereas those with an eGFR 30–44 ml min−1 1.73 m−2 (G3bA1a and b) had higher HRs (1.85 and 2.25, respectively), compared with individuals with microalbuminuria and preserved eGFR (G1A2-G2A2; HRs 1.31 to 1.39). Moreover, normoalbuminuric individuals with an eGFR 45–59 ml min−1 1.73 m−2 (G3aA1a and b) had lower HRs, whereas those with an eGFR 30–44 ml min−1 1.73 m−2 (G3bA1a and b), especially if in the low albuminuria range, had similar HRs to individuals with macroalbuminuria and preserved eGFR (G1A3-G2A3; HRs 1.71 to 2.48) (Fig. 3).
Survival analysis by Cox proportional hazards regression, adjusted for multiple confounders, according to KDIGO risk category and subcategory. eGFR categories are indicated by ‘G’, from G1 (≥90 ml min−1 1.73 m−2) to G4–5 (<30 ml min−1 1.73 m−2). Albuminuria categories are indicated by ‘A’, from A1a (AER <10 mg/day) to A3 (AER ≥300 mg/day). HRs for mortality with 95% CIs are shown for each category/subcategory; p < 0.0001 across the KDIGO categories/subcategories by Cox proportional hazards regression. Ref, reference. Increasing risk for mortality indicated from green through yellow, orange, red
Using RECPAM analysis, history of CVD was the most relevant correlate of mortality in all phenotypes, followed by lower levels of HDL-cholesterol (Figs. 4 and 5). Furthermore, the following variables were associated with higher mortality in a DKD phenotype-dependent manner: higher AER within the normoalbuminuric range, lower LDL-cholesterol and higher eWC in non-albuminuric DKD (Fig. 4); presence of any diabetic retinopathy, higher HbA1c, male sex and lower diastolic BP in albuminuric DKD with preserved eGFR (Fig. 5a); and longer diabetes duration, male sex and no lipid-lowering treatment in albuminuric DKD with reduced eGFR (Fig. 5b). The Kaplan–Meier curves for each DKD phenotype according to the RECPAM final subgroups are presented in ESM Fig. 4.
RECPAM tree-growing algorithm for identification of Alb−/eGFR+ (non-albuminuric DKD) participant subgroups with different mortality risks. The analysis was conducted on individuals with calculable LDL-cholesterol values. The data in the circles and squares represent the number of deaths (upper) and the number of participants (lower) in each subgroup. The squares indicate the final RECPAM class. The HRs for mortality with 95% CIs are shown for each class and the global variable (age). HDL-C, HDL-cholesterol; LDL-C, LDL-cholesterol
RECPAM tree-growing algorithm for identification of Alb+/eGFR− (albuminuric DKD with preserved eGFR, a) and Alb+/eGFR+ (albuminuric DKD with reduced eGFR, b) participant subgroups with different mortality risks. The analysis was conducted on individuals with calculable LDL-cholesterol values. The data in the circles and squares represent the number of deaths (upper) and the number of participants (lower) in each subgroup. The squares indicate the final RECPAM class. The HRs for mortality with 95% CIs are shown for each class and the global variable (age). DBP, diastolic BP; DM, diabetes mellitus; DR, diabetic retinopathy; F, female; HDL-C, HDL-cholesterol; LLT, lipid-lowering treatment; M, male
Regarding the non-albuminuric phenotype, RECPAM analysis identified eight subgroups with distinct mortality risks (Fig. 4 and ESM Table 5). As in the other phenotypes, history of CVD was the most relevant correlate of subsequent death, which was more likely in participants with HDL-cholesterol ≤ 1.14 mmol/l (class 1; HR 3.8) than in those with HDL-cholesterol above this threshold and, within the latter group, in individuals with LDL-cholesterol ≤2.64 mmol/l (class 2; HR 2.9) than in those with values above this threshold (class 3; HR 1.9). Among participants without CVD, risk of death was higher in individuals with AER >8.3 mg/day and particularly in those with AER >13.6 mg/day and eWC >104 cm (class 4; HR 3.0) than in those with values at or below these cut-offs (class 5; HR 2.0 and class 6; HR 1.6, respectively). Finally, among participants without CVD and with AER ≤ 8.3 mg/day, those with HDL-cholesterol ≤ 1.17 mmol/l had a higher risk (Class 7; HR 1.7) than those with HDL-cholesterol >1.17 mmol/l (Class 8; reference).
Discussion
Non-albuminuric renal impairment has become the prevailing DKD phenotype in individuals with type 2 diabetes and reduced eGFR, though it is still unclear whether it differs from the albuminuric phenotypes regarding the pathogenesis, prognosis and possibly treatment.
The increasing prevalence of the non-albuminuric DKD phenotype over the last decades may reflect the increasing age of the population, but the increase in prevalence of reduced eGFR was observed in both younger and older individuals from the NHANES III 1988–1994 cohort [2]. More likely, it may be related to the increasingly widespread use of blockers of the renin–angiotensin system (RAS) [2], favouring prevention of albuminuria and/or regression of micro/macroalbuminuria to normoalbuminuria [32, 33]. However, the NHANES III 1988–1994 findings only partly support this hypothesis, as reduction of albuminuria was associated with an absolute, not relative, increase in prevalence of reduced eGFR [2]. In addition, the progressive lowering of average blood pressure during the past two decades among adults with diabetes may have resulted in reduction of renal perfusion pressure and, hence, of eGFR in some of these individuals [2]. The increasing prevalence of the non-albuminuric phenotype may also reflect the continuing decrease in mortality [34] and progression to end-stage renal disease [35] observed in recent years in diabetic people because of improved treatment, but reduction in mortality was confined to individuals with albuminuria (see below). The weak association with diabetic retinopathy and the lack of association with HbA1c [6, 11, 36] suggest that non-albuminuric DKD may represent a distinct phenotype, with macroangiopathy instead of microangiopathy as the prevailing underlying pathology [4, 5]. This would be the case especially in individuals with type 2 diabetes, who present with several CVD risk factors in addition to hyperglycaemia, including hypertension, dyslipidaemia, central obesity and ageing itself, all of which may contribute to renal injury, though to a varying extent in each individual [4, 5]. Unfortunately, the clinical phenotype cannot be related to a specific anatomical phenotype, with presence or absence of albuminuria corresponding to typical glomerular or atypical vascular and/or tubulo-interstitial lesions, respectively. In fact, among individuals with reduced eGFR, those with micro/macroalbuminuria were found to have typical glomerular lesions, whereas half of those with normoalbuminuria showed atypical lesions, but the other half still presented with diabetic glomerulosclerosis, though associated with varying degrees of arteriosclerosis [37]. Moreover, a wide spectrum of renal pathology, including atypical lesions, was also observed in individuals with type 2 diabetes with preserved renal function and microalbuminuria [38], whereas typical (glomerular) microangiopathic lesions were detected in individuals with type 1 diabetes and normoalbuminuric renal impairment [39]. For these reasons, true diabetic nephropathy (glomerulosclerosis) cannot be distinguished on a clinical basis from ischaemic or hypertensive renal disease occurring in individuals with type 2 diabetes, thus prompting the use of DKD to encompass all types of renal dysfunction occurring in diabetic individuals, except for those of true non-diabetic nature [2, 4, 5].
To date, few data are available on the rate of death in both diabetic and non-diabetic individuals presenting with non-albuminuric DKD. Two meta-analyses from the general population [17, 18] and high-CVD-risk cohorts (including diabetic individuals) [18] showed that all-cause and CVD mortality increase for eGFR values below 45 or 60 ml min−1 1.73 m−2 in the presence of ACR <10 mg/g or dipstick-negative proteinuria. Information on mortality rates associated with the non-albuminuric phenotype has been derived from studies in individuals with type 2 diabetes, though the results are not univocal. A post hoc analysis of the Action in Diabetes and Vascular disease: preterAx and diamicroN-MR Controlled Evaluation (ADVANCE) study (10,640 participants) showed that risk of CVD death associated with non-albuminuric DKD was similar to that of microalbuminuria with an eGFR ≥90 ml min−1 1.73 m−2, but lower than that of microalbuminuria with an eGFR 60–89 ml min−1 1.73 m−2 and of macroalbuminuria with an eGFR >60 ml min−1 1.73 m−2 [9]. Conversely, a post hoc analysis of the Fenofibrate Intervention and Event Lowering in Diabetes (FIELD) study (9795 participants) showed that the non-albuminuric phenotype was associated with a higher risk of CVD, non-CVD and all-cause death compared with that of microalbuminuria with an eGFR >60 ml min−1 1.73 m−2 and even of macroalbuminuria ≥90 ml min−1 1.73 m−2 [10]. However, the results of these two post hoc analyses might have been affected by the selection criteria for trial entry, resulting in a limited number of individuals with eGFR <60 ml min−1 1.73 m−2, which did not allow grading of mortality risk within the range of reduced eGFR. The community-based Casale Monferrato Study (1565 persons) detected a significant trend towards an increase in mortality risk with decreasing eGFR only in macroalbuminuric individuals [20]. In contrast, in the Cardiovascular Health Study (691 older diabetic adults), the adjusted risk of death was similar for albuminuria alone and reduced cystatin C-based eGFR alone [40]. Linking the NHANES III data with the National Death Index (1430 persons) revealed that the standardised 10 year mortality in the non-albuminuric phenotype was intermediate between the albuminuric DKD phenotypes without and with reduced eGFR [21]. Of note, serial cross-sectional analyses of the NHANES III data showed that mortality rates in adults with diabetes trended downward for individuals with increased albuminuria, but increased for those with decreased eGFR and normoalbuminuria from 1988 to 2006 [41]. These time-dependent changes in mortality associated with albuminuria alone vs reduced eGFR alone may also explain, at least partly, the different mortality data reported by previous studies [9, 10, 20, 21, 40].
Our study specifically addressed mortality in individuals with type 2 diabetes and non-albuminuric DKD and graded the risk of death according to the extent of albuminuria and eGFR loss within the normal and reduced range, respectively. The results indicated that non-albuminuric renal impairment is associated with a significant risk of death, despite the risk associated with reduced eGFR values sometimes being underestimated in the absence of albuminuria. The adjusted HR of reduced eGFR alone was similar to that of albuminuria alone. Moreover, in normoalbuminuric participants with eGFR 45–59 ml min−1 1.73 m−2, risk was similar to that of individuals with microalbuminuria alone and, in those with eGFR <45 ml min−1 1.73 m−2, it was similar to that of participants with macroalbuminuria alone.
These results are consistent with the very recent report from NHANES III showing that, in the 2003–2006 population, age-standardised mortality risk with non-albuminuric DKD was indeed higher than for microalbuminuria alone and macroalbuminuria with eGFR ≥90 ml min−1 1.73 m−2, but lower than for macroalbuminuria with eGFR 60–89 60 ml min−1 1.73 m−2 [41]. Data from both the RIACE and the NHANES III cohorts point to a major prognostic value of CKD irrespective of albuminuria and indicate that changes in treatment, particularly the increasing use of RAS blockers resulting in lower blood pressure levels, have not impacted favourably on mortality in the non-albuminuric phenotype. The lack of effective therapeutic interventions in individuals presenting with this phenotype may also be because, so far, clinical trials have focused almost exclusively on individuals with micro- or macroalbuminuria. The finding that, in individuals aged <55 years, non-albuminuric DKD was associated with the highest risk of death has no obvious explanation and must be interpreted with caution owing to the very small number of individuals in this group.
At RECPAM analysis, variables associated with mortality risk in each DKD phenotype include history of CVD and traditional CVD risk factors, consistent with the major contribution of CVD to excess death in diabetic individuals [15]. Previous CVD events and HDL-cholesterol are the main determinants of mortality in all DKD phenotypes, in accordance with the strict relation of renal impairment with CVD morbidity and mortality [42] and the predictive value of HDL-cholesterol for CVD outcomes in individuals with type 2 diabetes [43], especially in those on target for LDL-cholesterol [44]. The inverse association of mortality with LDL-cholesterol and diastolic BP (and with total cholesterol and systolic BP in Cox regression analysis) likely represents an indication effect, i.e. individuals with more complications who are therefore at higher risk of death were treated more intensively and, as a consequence, presented with lower cholesterol and BP levels. In addition, this analysis demonstrates that the other variables associated with all-cause mortality differ among DKD phenotypes, thus supporting the concept that the non-albuminuric form is distinct from the albuminuric ones. In particular, AER levels within the normoalbuminuric range, together with higher eWC, were shown to affect mortality in individuals with non-albuminuric DKD without prevalent CVD. Conversely, death in the non-albuminuric phenotype was not associated with classic ‘microvascular signatures’ such as glycaemic exposure (HbA1c, diabetes duration) and diabetic retinopathy, at variance with the albuminuric phenotypes and consistent with the hypothesis of a prevailing macrovascular nature of underlying lesions [11].
The strengths of this study include the specific focus on the non-albuminuric DKD phenotype, the large size of the cohort, the completeness of baseline and follow-up data, the analysis of a contemporary and real-life dataset and the application of RECPAM analysis, which allowed the identification of clinical features of subgroups with distinct mortality risks within each DKD phenotype. Furthermore, our cohort may be considered as representative of type 2 diabetic individuals not receiving dialysis attending tertiary referral diabetes clinics in Italy. The main limitation is that these individuals do not represent the totality of people with type 2 diabetes, as a proportion are not followed in such centres. Other limitations are the relatively low number of participants with eGFR <30 ml min−1 1.73 m−2, the lack of information on causes of death and the possible, though inevitable, misclassification of some individuals into DKD phenotypes, due to the influence of drug treatment on both albuminuria and serum creatinine and imprecision of GFR estimation from creatinine, which may cause either under- or overestimation of eGFR. However, Rigalleau et al showed that correlation of eGFR with isotopic GFR was not weaker in non-albuminuric than in albuminuric individuals with reduced eGFR [45], indicating that the likelihood of eGFR underestimation is not restricted to the non-albuminuric phenotype. In addition, factors such as age and use of RAS blockers, which may affect eGFR (and albuminuria) and impact on mortality independently of renal function, were similar in non-albuminuric and albuminuric individuals with reduced eGFR from the RIACE cohort (use of RAS blockers was also similar in non-albuminuric and albuminuric individuals with preserved eGFR). Other potential limitations of the methods have been extensively addressed elsewhere [11, 22,23,24, 29, 30, 36].
In conclusion, the non-albuminuric DKD phenotype is a strong predictor of all-cause mortality in individuals with type 2 diabetes, particularly so in individuals with eGFR <45 ml min−1 1.73 m−2, who have a risk of all-cause mortality that is higher than individuals with microalbuminuria alone and similar to those with macroalbuminuria alone, especially if AER is in the low albuminuria range. Determinants of mortality risk in non-albuminuric renal impairment differ, at least in part, from those of the albuminuric forms, thus indicating that this is a distinct phenotype. These data indicate a major prognostic impact of CKD irrespective of albuminuria and suggest that individuals with non-albuminuric DKD deserve a higher level of attention and care than is generally provided. In particular, the rising mortality rate associated with this increasingly prevalent non-albuminuric DKD phenotype [41] indicates the need for effective intervention strategies and public health policies focusing on reduced eGFR.
Data availability
Data are available upon request from the authors.
Abbreviations
- ACR:
-
Albumin-to-creatinine ratio
- CKD:
-
Chronic kidney disease
- CVD:
-
Cardiovascular disease
- DKD:
-
Diabetic kidney disease
- eAER:
-
Estimated AER
- eGFR:
-
Estimated GFR
- eWC:
-
Estimated waist circumference
- KDIGO:
-
Kidney Disease: Improving Global Outcomes
- mAER:
-
Measured AER
- NHANES III:
-
Third National Health and Nutrition Examination Survey
- RAS:
-
Renin–angiotensin system
- RECPAM:
-
recursive partitioning and amalgamation
- RIACE:
-
Renal Insufficiency And Cardiovascular Events
References
de Boer IH, Rue TC, Hall YN, Heagerty PJ, Weiss NS, Himmelfarb J (2011) Temporal trends in the prevalence of diabetic kidney disease in the United States. JAMA 305:2532–2539
Afkarian M, Zelnick LR, Hall YN et al (2016) Clinical manifestations of kidney disease among US adults with diabetes, 1988-2014. JAMA 316:602–610
Mogensen CE (1999) Microalbuminuria, blood pressure and diabetic renal disease: origin and development of ideas. Diabetologia 42:263–285
Pugliese G (2014) Updating the natural history of diabetic nephropathy. Acta Diabetol 51:905–915
Porrini E, Ruggenenti P, Mogensen CE et al (2015) Non-proteinuric pathways in loss of renal function in patients with type 2 diabetes. Lancet Diabetes Endocrinol 3:382–391
Kramer HJ, Nguyen QD, Curhan G, Hsu CY (2003) Renal insufficiency in the absence of albuminuria and retinopathy among adults with type 2 diabetes mellitus. JAMA 289:3273–3277
Retnakaran R, Cull CA, Thorne KI, Adler AI, Holman RR, UKPDS Study Group (2006) Risk factors for renal dysfunction in type 2 diabetes: U.K. Prospective Diabetes Study 74. Diabetes 55:1832–1839
Thomas MC, Macisaac RJ, Jerums G et al (2009) Nonalbuminuric renal impairment in type 2 diabetic patients and in the general population (national evaluation of the frequency of renal impairment cO-existing with NIDDM [NEFRON] 11). Diabetes Care 32:1497–1502
Ninomiya T, Perkovic V, de Galan BE et al (2009) Albuminuria and kidney function independently predict cardiovascular and renal outcomes in diabetes. J Am Soc Nephrol 20:1813–1821
Drury PL, Ting R, Zannino D et al (2011) Estimated glomerular filtration rate and albuminuria are independent predictors of cardiovascular events and death in type 2 diabetes mellitus: the Fenofibrate Intervention and Event Lowering in Diabetes (FIELD) study. Diabetologia 54:32–43
Penno G, Solini A, Bonora E et al (2011) Clinical significance of nonalbuminuric renal impairment in type 2 diabetes. J Hypertens 29:1802–1809
Molitch ME, Steffes M, Sun W et al (2010) Development and progression of renal insufficiency with and without albuminuria in adults with type 1 diabetes in the diabetes control and complications trial and the epidemiology of diabetes interventions and complications study. Diabetes Care 33:1536–1543
Thorn LM, Gordin D, Harjutsalo V et al (2015) The presence and consequence of nonalbuminuric chronic kidney disease in patients with type 1 diabetes. Diabetes Care 38:2128–2133
Penno G, Russo E, Garofolo M et al (2017) Evidence for two distinct phenotypes of chronic kidney disease in individuals with type 1 diabetes mellitus. Diabetologia 60:1102–1113
Rao Kondapally Seshasai S, Kaptoge S, Thompson A et al (2011) Diabetes mellitus, fasting glucose, and risk of cause-specific death. N Engl J Med 364:829–841
Astor BC, Hallan SI, Miller ER 3rd, Yeung E, Coresh J (2008) Glomerular filtration rate, albuminuria, and risk of cardiovascular and all-cause mortality in the US population. Am J Epidemiol 167:1226–1234
Chronic Kidney Disease Prognosis Consortium, Matsushita K, van der Velde M et al (2010) Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet 375:2073–2081
Fox CS, Matsushita K, Woodward M et al (2012) Associations of kidney disease measures with mortality and end-stage renal disease in individuals with and without diabetes: a meta-analysis. Lancet 380:1662–1673
Astor BC, Matsushita K, Gansevoort RT et al (2011) Lower estimated glomerular filtration rate and higher albuminuria are associated with mortality and end-stage renal disease. A collaborative meta-analysis of kidney disease population cohorts. Kidney Int 79:1331–1340
Bruno G, Merletti F, Bargero G et al (2007) Estimated glomerular filtration rate, albuminuria and mortality in type 2 diabetes: the Casale Monferrato study. Diabetologia 50:941–948
Afkarian M, Sachs MC, Kestenbaum B et al (2013) Kidney disease and increased mortality risk in type 2 diabetes. J Am Soc Nephrol 24:302–308
Penno G, Solini A, Bonora E et al (2018) Defining the contribution of chronic kidney disease to all-cause mortality in patients with type 2 diabetes: the Renal Insufficiency And Cardiovascular Events (RIACE) Italian multicenter study. Acta Diabetol 55:603–612
Penno G, Solini A, Bonora E et al (2013) Gender differences in cardiovascular disease risk factors, treatments and complications in patients with type 2 diabetes: the RIACE Italian multicentre study. J Intern Med 274:176–191
Pugliese G, Solini A, Fondelli C et al (2011) Reproducibility of albuminuria in type 2 diabetic subjects. Findings from the Renal Insufficiency And Cardiovascular Events (RIACE) study. Nephrol Dial Transplant 26:3950–3954
Mangili R, Deferrari G, Di Mario U et al (1992) Prevalence of hypertension and microalbuminuria in adult type 1 (insulin-dependent) diabetic patients without renal failure in Italy. I. Validation of screening techniques to detect microalbuminuria. Acta Diabetol 29:156–166
Abdelmalek JA, Gansevoort RT, Lambers Heerspink HJ, Ix JH, Rifkin DE (2014) Estimated albumin excretion rate versus urine albumin-creatinine ratio for the assessment of albuminuria: a diagnostic test study from the Prevention of Renal and Vascular Endstage Disease (PREVEND) study. Am J Kidney Dis 63:415–421
Penno G, Solini A, Zoppini G et al (2015) Independent correlates of urinary albumin excretion within the normoalbuminuric range in patients with type 2 diabetes: the Renal Insufficiency And Cardiovascular Events (RIACE) Italian multicentre study. Acta Diabetol 52:971–981
Levey AS, Stevens LA, Schmid CH et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–612
Penno G, Solini A, Zoppini G et al (2012) Rate and determinants of association between advanced retinopathy and chronic kidney disease in patients with type 2 diabetes: the Renal Insufficiency And Cardiovascular Events (RIACE) Italian multicenter study. Diabetes Care 35:2317–2323
Solini A, Penno G, Bonora E et al (2012) Diverging association of reduced glomerular filtration rate and albuminuria with coronary and noncoronary events in patients with type 2 diabetes: the Renal Insufficiency And Cardiovascular Events (RIACE) Italian multicenter study. Diabetes Care 35:143–149
Ciampi A, Hogg SA, McKinney S, Thiffault J (1988) RECPAM: a computer program for recursive partition and amalgamation for censored survival data and other situations frequently occurring in biostatistics. I. Methods and program features. Comput Methods Prog Biomed 26:239–256
Perkins BA, Ficociello LH, Silva KH, Finkelstein DM, Warram JH, Krolewski AS (2003) Regression of microalbuminuria in type 1 diabetes. N Engl J Med 348:2285–2293
Gaede P, Tarnow L, Vedel P, Parving HH, Pedersen O (2004) Remission to normoalbuminuria during multifactorial treatment preserves kidney function in patients with type 2 diabetes and microalbuminuria. Nephrol Dial Transplant 19:2784–2788
Gregg EW, Cheng YJ, Saydah S et al (2012) Trends in death rates among U.S. adults with and without diabetes between 1997 and 2006: findings from the National Health Interview Survey. Diabetes Care 35:1252–1257
Burrows NR, Li Y, Geiss LS (2010) Incidence of treatment for end-stage renal disease among individuals with diabetes in the U.S. continues to decline. Diabetes Care 33:73–77
Penno G, Solini A, Bonora E et al (2013) HbA1c variability as an independent correlate of nephropathy, but not retinopathy, in patients with type 2 diabetes: the Renal Insufficiency And Cardiovascular Events (RIACE) Italian multicenter study. Diabetes Care 36:2301–2310
Ekinci EI, Jerums G, Skene A et al (2013) Renal structure in normoalbuminuric and albuminuric patients with type 2 diabetes and impaired renal function. Diabetes Care 36:3620–3626
Fioretto P, Mauer M, Brocco E et al (1996) Patterns of renal injury in NIDDM patients with microalbuminuria. Diabetologia 39:1569–1576
Caramori ML, Fioretto P, Mauer M (2003) Low glomerular filtration rate in normoalbuminuric type 1 diabetic patients: an indicator of more advanced glomerular lesions. Diabetes 52:1036–1040
de Boer IH, Katz R, Cao JJ et al (2009) Cystatin C, albuminuria, and mortality among older adults with diabetes. Diabetes Care 32:1833–1838
Kramer H, Boucher RE, Leehey D et al (2018) Increasing mortality in adults with diabetes and low estimated glomerular filtration rate in the absence of albuminuria. Diabetes Care 41:775–781
Gansevoort RT, Correa-Rotter R, Hemmelgarn BR et al (2013) Chronic kidney disease and cardiovascular risk: epidemiology, mechanisms, and prevention. Lancet 382:339–352
Drexel H, Aczel S, Marte T et al (2005) Is atherosclerosis in diabetes and impaired fasting glucose driven by elevated LDL cholesterol or by decreased HDL cholesterol? Diabetes Care 28:101–107
Sharif S, van der Graaf Y, Nathoe HM et al (2016) HDL cholesterol as a residual risk factor for vascular events and all-cause mortality in patients with type 2 diabetes. HDL cholesterol as a residual risk factor for vascular events and all-cause mortality in patients with type 2 diabetes. Diabetes Care 39:1424–1430
Rigalleau V, Lasseur C, Raffaitin C et al (2007) Normoalbuminuric renal-insufficient diabetic patients. Diabetes Care 30:2034–2039
Acknowledgements
The authors thank the participants and the RIACE Investigators (see ESM for a complete list) for participating in this study.
Some of the data have been presented as an abstract at the EASD meeting in 2017.
Funding
This research was supported by the Research Foundation of the Italian Diabetes Society (Diabete Ricerca) and the Diabetes, Endocrinology and Metabolism (DEM) Foundation, and by unconditional grants from Eli Lilly, Sigma-Tau, Takeda, Chiesi Farmaceutici and Boehringer Ingelheim. The funders had no role in the study’s design, conduct or reporting.
Author information
Authors and Affiliations
Consortia
Contributions
GPe, AS, AN and GPu conceived and designed the study. All authors contributed to data acquisition or analysis, and interpretation. GPu drafted the manuscript. GPe, AS, EO, EB, CF, RT, MV, FC, OL, MS and AN revised the manuscript critically for important intellectual content. All authors approved the final version. GPu is responsible for the integrity of the work as a whole.
Corresponding author
Ethics declarations
GPe has received: consulting fees from AstraZeneca, Boehringer Ingelheim and Eli Lilly; and lecture fees from AstraZeneca, Boehringer Ingelheim, Eli Lilly and MSD. AS has received: consulting fees from AstraZeneca, Boehringer Ingelheim and Eli Lilly; lecture fees from AstraZeneca, Boehringer Ingelheim and Eli Lilly; and grant support from AstraZeneca. EO has received consulting fees from Boehringer Ingelheim, Eli Lilly, Novo Nordisk and Sanofi Aventis; and lecture fees from Abbot, AstraZeneca, Eli Lilly, Lifescan, Sanofi Aventis and Takeda. EB has received: consulting fees from AstraZeneca, Boehringer Ingelheim and Eli Lilly; lecture fees from Bristol-Myers Squibb, Eli Lilly, Janssen, MSD, Novo Nordisk, Roche, Sanofi Aventis and Takeda; and grant support from AstraZeneca, Novo Nordisk, Roche and Takeda. RT has received: consulting fees from Boehringer Ingelheim and Sanofi Aventis; lecture fees from AstraZeneca, Boehringer Ingelheim, Eli Lilly, Janssen, Medtronic, Novartis, Novo Nordisk and Sanofi Aventis; and grant support from AstraZeneca, Boehringer Ingelheim, Eli Lilly, Janssen, Novo Nordisk and Sanofi Aventis. FC has received lecture fees from AstraZeneca, Sanofi Aventis and Takeda. OL has received: consulting fees from AstraZeneca and Boehringer Ingelheim; lecture fees from AstraZeneca, Eli Lilly, MSD, Sigma-Tau, Sanofi Aventis and Takeda; and grant support from AstraZeneca. AN has received consulting fees from Eli Lilly and Novo Nordisk; lecture fees from Eli Lilly and Novo Nordisk; and grant support from Artsana, AstraZeneca, Eli Lilly, Novo Nordisk and Sanofi Aventis. GPu has received: consulting fees from AstraZeneca, Boehringer Ingelheim, Eli Lilly and Shire; and lecture fees from AstraZeneca, Boehringer Ingelheim, Eli Lilly, MSD, Mylan, Sigma-Tau and Takeda. All other authors declare that there is no duality of interest associated with their contribution to this manuscript.
Additional information
A complete list of RIACE Investigators is given in the electronic supplementary material.
Electronic supplementary material
ESM
(PDF 833 kb)
Rights and permissions
About this article
Cite this article
Penno, G., Solini, A., Orsi, E. et al. Non-albuminuric renal impairment is a strong predictor of mortality in individuals with type 2 diabetes: the Renal Insufficiency And Cardiovascular Events (RIACE) Italian multicentre study. Diabetologia 61, 2277–2289 (2018). https://doi.org/10.1007/s00125-018-4691-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-018-4691-2