Abstract
Background
Ultrasound-guided supraclavicular brachial plexus block is widely used in upper limb surgery; however, it requires a higher dose (20–30 mL) of local anesthetic. In this study, we aimed to determine the 90% minimum effective volume for ultrasound-guided supraclavicular brachial plexus block.
Methods
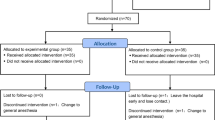
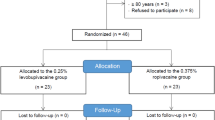
All patients received an ultrasound-guided two-point injection of 0.5% ropivacaine at a starting volume of 0.18 mL/mm2 cross-sectional nerve area. In cases of a successful block, the next patient had the same volume with a probability of 0.89, and the volume was reduced by 0.04 mL/mm2 cross-sectional nerve area with a probability of 0.11. When the block failed, the dose was increased by 0.04 mL/mm2 cross-sectional nerve area. After 45 cases of successful blocks, the 90% minimum effective volume of local anesthetic was calculated using the centered isotonic regression function.
Results
Centered isotonic regression analysis resulted in a 90% minimum effective volume and a 95% confidence interval of 0.189 mL/mm2 and 0.176–0.225 mL/mm2 for the supraclavicular brachial plexus block.
Conclusion
A good blocking effect can be achieved with 0.189 mL/mm2 of 0.5% ropivacaine with more precise dosing, thereby reducing the risk of local anesthetic poisoning.
Zusammenfassung
Hintergrund
Die ultraschallgesteuerte supraklavikuläre Blockade des Plexus brachialiswird häufig bei Eingriffen an den oberen Extremitäten eingesetzt. Allerdings erfordert sie eine höhere Dosis (20–30 ml) des Lokalanästhetikums. Ziel dieser Studie war es, das 90 %ige minimale effektive Volumen für die ultraschallgesteuerte supraklavikuläre Plexus-brachialis-Blockade zu bestimmen.
Methoden
Alle Patienten erhielten eine ultraschallgesteuerte Zweipunkt-Injektion von 0,5 % Ropivacain bei einem Ausgangsvolumen von 0,18 ml/mm2 Nervenquerschnittsfläche. Bei erfolgreicher Blockade erhielt der nächste Patient mit einer Wahrscheinlichkeit von 0,89 dasselbe Volumen, und das Volumen wurde um 0,04 ml/mm2 Nervenquerschnittsfläche mit einer Wahrscheinlichkeit von 0,11 reduziert. Bei Misserfolg der Blockade wurde die Dosis um 0,04 ml/mm2 Nervenquerschnittsfläche erhöht. Nach 45 erfolgreichen Blockaden wurde das 90 %ige minimale effektive Volumen der Lokalanästhetika mithilfe der zentrierten isotonischen Regressionsfunktion berechnet.
Ergebnisse
Die zentrierte isotonische Regressionsanalyse ergab ein 90 %iges minimales effektives Volumen und ein 95 % Konfidenzintervall (KI) von 0,189 ml/mm2 bzw. 0,176–0,225 ml/mm2 für die supraklavikuläre Plexus-brachialis-Blockade.
Schlussfolgerung
Ein guter Blockadeeffekt kann mit 0,189 ml/mm2 0,5 % Ropivacain erzielt werden, was zu einer präziseren Dosierung führt und somit das Risiko einer Lokalanästhetika-Intoxikation reduziert.




Similar content being viewed by others
Abbreviations
- CSA:
-
Cross-sectional area
- ED90 :
-
90% effective dose
- ED99 :
-
99% effective dose
- SCBPB:
-
Supraclavicular brachial plexus block
References
Datta R, Agrawal J, Narula G et al (2019) A fluoroscopic assessment of brachial plexus block by the supraclavicular approach: Have we been overmedicating? Med J Armed Forces India 76(4):410–417. https://doi.org/10.1016/j.mjafi.2019.06.004
Latzke D, Marhofer P, Zeitlinger M et al (2009) Minimal local anaesthetic volumes for sciatic nerve block: evaluation of ED 99 in volunteers. Br J Anaesth 104(2):239–244. https://doi.org/10.1093/bja/aep368
Haun DW, Cho JC, Clark TB et al (2009) Normative cross-sectional area of the brachial plexus and subclavian artery using ultrasonography. J Manipulative Physiol Ther. https://doi.org/10.1016/j.jmpt.2009.08.003
Techasuk W, González AP, Bernucci F, Cupido T, Finlayson RJ, Tran DQ (2014) A randomized comparison between double-injection and targeted intracluster-injection ultrasound-guided supraclavicular brachial plexus block. Anesth Analg 118(6):1363–1369. https://doi.org/10.1213/ANE.0000000000000224
Stylianou M, Flournoy N (2002) Dose finding using the biased coin up-and-down design and isotonic regression. Biometrics 58(1):171–177. https://doi.org/10.1111/j.0006-341x.2002.00171.x
Gupta PK, Pace NL, Hopkins PM (2010) Effect of body mass index on the ED50 volume of bupivacaine 0.5 % for supraclavicular brachial plexus block. Br J Anaesth 104(4):490–495. https://doi.org/10.1093/bja/aeq017
Fang G, Wan L, Mei W et al (2016) The minimum effective concentration (MEC90 ) of ropivacaine for ultrasound-guided supraclavicular brachial plexus block. Anaesthesia 71(6):700–705. https://doi.org/10.1111/anae.13445
Fang G, Wan L, Li S et al (2021) An optimal dose of ropivacaine for ultrasound-guided supraclavicular brachial plexus block: a biased coin design. Eur J Anaesthesiol 38(2):186–187. https://doi.org/10.1097/EJA.0000000000001298
Eichenberger U, Stöckli S, Marhofer P et al (2009) Minimal local anesthetic volume for peripheral nerve block: a new ultrasound-guided, nerve dimension-based method. Reg Anesth Pain Med 34(3):242–246. https://doi.org/10.1097/AAP.0b013e31819a7225
Renes SH, Spoormans HH, Gielen MJ et al (2009) Hemidiaphragmatic paresis can be avoided in ultrasound-guided supraclavicular brachial plexus block. Reg Anesth Pain Med. https://doi.org/10.1097/aap.0b013e3181bfbd83
Bigeleisen PE (2003) Anatomical variations of the phrenic nerve and its clinical implication for supraclavicular block. Br J Anaesth. https://doi.org/10.1093/bja/aeg254
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Q. Xuan, R. Pan, A. Wang, R. Li, X. Yang and G. Yin declare that they have no competing interests.
This study was conducted after approval by the Ethics Committee of the First Affiliated Hospital of Dali University (approval No.:2022052007) in accordance with the Declaration of Helsinki (1964) and adhered to the CONSORT guidelines. All patients were informed about the study and signed the informed consent.
The supplement containing this article is not sponsored by industry.
Additional information

Scan QR code & read article online
Rights and permissions
About this article
Cite this article
Xuan, Q., Pan, R., Wang, A. et al. The 90% minimum effective volume of 0.5 ropivacaine for ultrasound-guided supraclavicular brachial plexus block. Anaesthesiologie 72 (Suppl 1), 39–43 (2023). https://doi.org/10.1007/s00101-023-01344-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00101-023-01344-7
Keywords
- Brachial plexus block
- Ropivacaine
- Supraclavicular brachial plexus
- Cross-sectional nerve area
- Biased coin up-and-down design