Abstract
Objective
To describe the trend of acute self-poisoning in the emergency and intensive care.
Methods
Electronic charts of adults who presented to the emergency department of the University Hospital Leipzig with self-poisoning following a suicide attempt (suicide group), intoxication (intoxication group), drug overdose for relief of pain or discomfort (drug overdose group) between 2005 and 2012 were analyzed.
Results
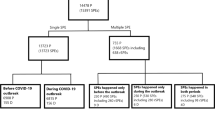
3533 adults (62.6 % males) were identified, with the yearly admissions increasing from 305 in 2005 to 624 in 2012. The admission rate in relation to the total emergency department admissions also increased, from 1.2 % in 2005 to 1.9 % in 2012. 31.7 % of the patients were younger than 25 years. The reasons for self-poisoning were suicide attempt (18.1 %), intoxication (76.8 %) and drug overdose (2.9 %). The reason could not be clearly classified in 80 patients. Psychotropic drugs were used in 71.6 % of suicide attempts, while alcohol was the sole cause of intoxication in 80.1 % of cases in the intoxication group. Self-poisoning using at least two substances was observed in 52.0 % of the suicide attempts, 10.3 % of those with intoxication and 29.7 % of those with drug overdose. While alcohol remains the most common cause of intoxication, there was a drastic increase in the consumption of cannabinoids, Crystal Meth and gamma-hydroxybutyrate in the years 2011 and 2012. ICU admission was necessary in 16.6 % of the cases. There were 22 deaths (0.6 % of the study population), of whom 15 were in the suicide group (2.3 %), four (0.15 %) in the intoxication group, and three in the not clearly classified group (3.8 %).
Conclusion
Acute self-poisoning is an increasing medical issue. Psychotropic drugs remain the most common means of suicide attempt. Although alcohol intoxication is very frequent, intake of illicit drugs as the cause of emergency admission is increasing.
Zusammenfassung
Ziel
Beschreibung des Trends der akuten Selbstvergiftung in der Notfall- und Intensivmedizin.
Methode
Elektronische Akten erwachsener Patienten, die zwischen 2005 und 2012 wegen einer akuten Selbstvergiftung infolge eines Selbstmordversuches (Selbstmordgruppe), einer Berauschung (Intoxikationsgruppe) oder Medikamentenüberdosierung zwecks Schmerzlinderung (Überdosierungsgruppe) in der Notaufnahme des Universitätsklinikums Leipzig eingewiesen worden waren, wurden ausgewertet.
Ergebnisse
3533 Patienten (62,6 % männlich) wurden identifiziert, mit einem Anstieg von 305 Fällen im Jahre 2005 auf 624 in 2012. Die Aufnahmerate bezogen auf die Gesamtaufnahmen stieg von 1,2 % im Jahre 2005 auf 1,9 % im Jahre 2012 an. 31,7 % der Patienten waren < 25 Jahre alt. Die Ursachen der Selbstvergiftung waren Suizidversuch (18,1 %), Intoxikation (76,8 %) und Medikamentenüberdosierung (2,9 %). Bei 80 Fällen war eine genaue Gruppenzuordnung nicht möglich. Während psychotrope Medikamente bei 71,6 % der Suizidversuche angewandt wurden, war Alkoholintoxikation die Ursache bei 80,1 % der Fälle in der Intoxikationsgruppe. Selbstvergiftung mit mindestens zwei Substanzen lag bei 52,0 % der Suizidversuche, 10,3 % der Intoxikationsgruppe und 29,7 % der Gruppe mit Medikamentenüberdosierung vor. Während die Alkoholintoxikation nach wie vor am häufigsten vorkam, gab es eine drastische Zunahme der Intoxikationen mit Cannabinoiden, Crystal Meth und Gamma-Hydroxybuttersäure in den Jahren 2011 und 2012. Eine Aufnahme auf die Intensivstation war bei 16,6 % der Fälle erforderlich. Es gab 22 Todesfälle (0,6 % der gesamten Studienpopulation), von denen 15 aus der Suizidgruppe (2,3 %), vier aus der Intoxikationsgruppe (0,15 %), und drei aus der nicht eindeutig zugeordneten Gruppe (3.8 %) waren.
Zusammenfassung
Akute Selbstvergiftung ist ein zunehmendes medizinisches Problem. Psychotrope Medikamente stellen nach wie vor die häufigsten Suizidversuchsmittel dar. Obwohl die Alkoholintoxikation weiterhin am häufigsten vorkommt, nehmen illegale Drogen als notfallmedizinischer Einweisungsgrund zu.





Similar content being viewed by others
References
Babor T, Campbell R, Room R, Saunders J (1994) Lexicon of alcohol and drug terms. World Health Organization, Geneva
National Institute for Clinical Excellence (2004) Self-harm. The short-term physical and psychological management and secondary prevention of self-harm in primary and secondary care. National Clinical Practice Guideline Number 16. Stanley L. Hunt Ltd., Northamptonshire
Cook R, Allcock R, Johnston M (2008) Self-poisoning: current trends and practice in a U.K. teaching hospital. Clin Med 8:37–40
Prescott K, Stratton R, Freyer A, Hall I, Le Jeune I (2009) Detailed analyses of self-poisoning episodes presenting to a large regional teaching hospital in the UK. Br J Clin Pharmacol 68:260–268
Hendrix L, Verelst S, Desruelles D, Gillet J-B (2012) Deliberate self-poisoning: characteristics of patients and impact on the emergency department of a large university hospital. Emerg Med J 30:e9
Buchanan WJ (1991) A year of intentional self poisoning in Christchurch. N Z Med J 104:470–472
Fürst S, Habscheid W (1993) Acute poisoning in patients of a medical intensive care unit. Dtsch Med Wochenschr 118:849–853
Viertel A, Weidmann E, Brodt HR (2001) Cases of acute poisoning admitted to a medical intensive care unit. Dtsch Med Wochenschr 126:1159–1163
Schwake L, Wollenschlager I, Stremmel W, Encke J (2009) Adverse drug reactions and deliberate self-poisoning as cause of admission to the intensive care unit: a 1-year prospective observational cohort study. Intensive Care Med 35:266–274
Weir P, Ardagh M (1998) The epidemiology of deliberate self poisoning presenting to Christchurch Hospital Emergency Department. N Z Med J 111:127–129
Bentur Y, Raikhlin-Eisenkraft B, Lavee M (2004) Toxicological features of deliberate self-poisonings. Hum Exp Toxicol 23:331–337
Mauri MC, Cerveri G, Volonteri LS, Fiorentini A, Colasanti A, Manfré S, Borghini R, Pannacciulli E (2005) Parasuicide and drug self-poisoning: analysis of the epidemiological and clinical variables of the patients admitted to the Poisoning Treatment Centre (CAV), Niguarda General Hospital, Milan. Clin Pract Epidemiol Ment Health 1(1):5
Eisenbach C, Ungur AL, Unger J, Stremmel W, Encke J (2008) Admission to intensive care for parasuicide by self-poisoning: Variation by time cycles, climate and the lunar cycle. Psychiatry Res 161:177–184
Ghazinour M, Emami H, Richter J, Abdollahi M, Pazhumand A (2009) Age and gender differences in the use of various poisoning methods for deliberate parasuicide cases admitted to loghman hospital in Tehran (2000–2004). Suicide Life Threat Behav 39:231–239
Tsirigotis K, Gruszczynski W, Tsirigotis M (2011) Gender differentiation in methods of suicide attempts. Med Sci Monit 17:65–70
Kupferschmid S, Gysin-Maillart A, Bühler SK, Steffen T, Michel K, Schimmelmann BG, Reisch T (2013) Gender differences in methods of suicide attempts and prevalence of previous suicide attempts. Z Kinder Jugendpsychiatr Psychother 41:401–405
Busse F, Omidi L, Timper K, Leichtle A, Windgassen M, Kluge E, Stumvoll M (2008) Lead poisoning due to adulterated marijuana. N Engl J Med 358:1641–1642
Haw CM, Hawton K (2011) Problem drug use, drug misuse and deliberate self-harm: trends and patient characteristics, with a focus on young people, Oxford, 1993–2006. Soc Psychiatry Psychiatr Epidemiol 46:85–93
Oksa H, Pitkäjärvi T, Koskelainen J, Ruosteenoja R, Kataja M (1981) Self-poisoning patients in an intensive care unit. Ann Clin Res 13:96–101
Balsa AI, French MT, Maclean JC, Norton EC (2009) From pubs to scrubs: alcohol misuse and health care use. Health Serv Res 44:1480–1503
Weilemann LS, Hilgers HJ, Reckmann A (1996) Current aspects of para-suicidal poisoning. Med Klin (Munich) 91:355–358
Die Drogenbeauftragte der Bundesregierung, Bundesministerium für Gesundheit (2013) Drogen- und Suchtbericht. enka-druck GmbH, Berlin
Islambulchilar M, Islambulchilar Z, Kargar-Maher MH (2009) Acute adult poisoning cases admitted to a university hospital in Tabriz, Iran. Hum Exp Toxicol 28:185–190
Hatzitolios AI, Sion ML, Eleftheriadis NP, Toulis E, Efstratiadis G, Vartzopoulos D, Ziakas AG (2001) Parasuicidal poisoning treated in a Greek medical ward: epidemiology and clinical experience. Hum Exp Toxicol 20:611–617
Verstraete AG, Buylaert WA (1995) Survey of patients with acute poisoning seen in the Emergency Department of the University Hospital of Gent between 1983 and 1990. Eur J Emerg Med 2:217–223
Hall AK, Curry C (1994) Changing epidemiology and management of deliberate self poisoning in Christchurch. N Z Med J 107:396–399
Mowry JB, Spyker DA, Cantilena LR Jr, Bailey JE, Ford M (2013) 2012 Annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 30th annual report. Clin Toxicol (Phila) 51:949–1229
Spiller HA, Appana S, Brock GN (2010) Epidemiological trends of suicide and attempted suicide by poisoning in the US: 2000–2008. Leg Med (Tokyo) 12:177–183
Bergen H, Hawton K, Waters K, Cooper J, Kapur N (2010) Epidemiology and trends in non-fatal self-harm in three centres in England: 2000–2007. Br J Psychiatry 197:493–498
Camidge DR, Wood RJ, Bateman DN (2003) The epidemiology of self-poisoning in the UK. Br J Clin Pharmacol 56:613–619
McEvedy CJ (1997) Trends in self-poisoning: admissions to a central London hospital, 1991–1994. J R Soc Med 90:496–498
Oh SH, Park KN, Jeong SH, Kim HJ, Lee CC (2011) Deliberate self-poisoning: factors associated with recurrent self-poisoning. Am J Emerg Med 29:908–912
Payne RA, Oliver JJ, Bain M, Elders A, Bateman DN (2009) Patterns and predictors of re-admission to hospital with self-poisoning in Scotland. Public Health 123:134–137
Maignan M, Pommier P, Clot S, Saviuc P, Debaty G, Briot R, Carpentier F, Danel V (2014) Deliberate drug poisoning with slight symptoms on admission: are there predictive factors for intensive care unit referral? A three-year Retrospective Study. Basic Clin Pharmacol Toxicol 114:281–287
McMahon A, Brohan J, Donnelly M, Fitzpatrick GJ (2013) Characteristics of patients admitted to the intensive care unit following self-poisoning and their impact on resource utilisation. Ir J Med Sci 183:391–395
Weidhase L, Hentschel H, Mende L, Schulze G, Petros S (2014) Acute poisoning in adults. Internist (Berl) 55:281–294
Bjornaas MA, Hovda KE, Heyerdahl F, Skog K, Drottning P, Opdahl A, Jacobsen D, Ekeberg O (2010) Suicidal intention, psychosocial factors and referral to further treatment: a one-year cross-sectional study of self-poisoning. BMC Psychiatry 10:58
Brandenburg R, Brinkman S, de Keizer NF, Meulenbelt J, de Lange DW (2014) In-hospital mortality and long-term survival of patients with acute intoxication admitted to the ICU. Crit Care Med 42:1471–1479
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M. Sorge, L. Weidhase, M. Bernhard, A. Gries, S. Petros declare no conflict of interest.
The accompanying manuscript does not include studies on humans or animals.
Rights and permissions
About this article
Cite this article
Sorge, M., Weidhase, L., Bernhard, M. et al. Self-poisoning in the acute care medicine 2005–2012. Anaesthesist 64, 456–462 (2015). https://doi.org/10.1007/s00101-015-0030-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00101-015-0030-x