Abstract
Background
A satisfactory risk score specific to transaortic valve implantation (TAVI) procedure is strongly needed for accurate assessment of postprocedural mortality and outcome. The purpose of this study was to investigate the association between certain clinical and laboratory parameters, particularly serum cholesterol levels, and major adverse cardiac events in patients who underwent TAVI.
Method
We retrospectively analyzed 119 patients who underwent TAVI at our institution between 2008 and 2016. The independent relationship between clinical and laboratory parameters and major adverse cardiac and cerebrovascular events (MACCE) was analyzed by regression analysis.
Results
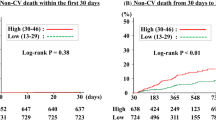
In all, 34 patients (28%) experienced MACCE during hospitalization and within 30 days of the procedure. Low-density lipoprotein cholesterol (LDL-C) and high-density lipoprotein cholesterol (HDL-C) levels were significantly lower in the MACCE(+) group compared with the MACCE(-) group (91.9 ± 38 vs. 110.8 ± 38.1 mg/dl, p = 0.01; 33.7 ± 7.3 vs. 38.1 ± 9.8 mg/dl, p = 0.02, respectively). In multivariate logistic regression analysis, age, white blood cell count (WBC), and lower levels of LDL-C and HDL-C were found to be independently correlated with MACCE in the study population. Receiver operating curve (ROC) analysis revealed that an LDL value higher than 71 mg/dl predicted MACCE with a sensitivity of 45.4% and a specificity of 91.8% (AUC: 0.814; p = 0.02).
Conclusion
This study suggests that lower serum LDL-C and HDL-C levels are independently associated with short-term MACCE in post-TAVI patients. Lower levels of LDL and HDL cholesterol may indicate a poor prognosis. Measurement of serum lipid levels might improve the preoperative risk assessment of potential TAVI candidates.
Zusammenfassung
Hintergrund
Ein zufriedenstellender Risikoscore, der sich speziell auf die transaortale Klappenimplantation (TAVI) bezieht, wird dringend benötigt, um postprozedural die Mortalität und den Verlauf genau ermitteln zu können. Ziel der vorliegenden Studie war es, den Zusammenhang zwischen bestimmten klinischen und Laborparametern, insbesondere Serumcholesterinwerten, und schweren unerwünschten kardialen Ereignissen bei Patienten nach TAVI zu untersuchen.
Methode
Die Autoren werteten retrospektiv die Daten von 119 Patienten aus, bei denen in der Klinik der Autoren zwischen 2008 und 2016 eine TAVI durchgeführt worden war. Die unabhängige Beziehung zwischen klinischen und Laborparametern und schweren unerwünschten kardialen und zerebrovaskulären Ereignissen (MACCE) wurde mit der Regressionsanalyse untersucht.
Ergebnisse
Insgesamt traten bei 34 Patienten (28 %) während des stationären Aufenthalts und innerhalb von 30 Tagen postoperativ MACCE auf. Die Spiegel für Low-Density-Lipoprotein-Cholesterin (LDL-C) und High-Density-Lipoprotein-Cholesterin (HDL-C) waren in der MACCE(+)-Gruppe signifikant niedriger als in der MACCE(-)-Gruppe (91,9 ± 38 vs. 110,8 ± 38,1 mg/dl; p = 0,01; bzw. 33,7 ± 7,3 vs. 38,1 ± 9,8 mg/dl; p = 0,02). In der multivariaten logistischen Regressionsanalyse stellte sich heraus, dass Alter, Zahl der weißen Blutkörperchen und niedrigere Spiegel für LDL-C und HDL-C in der Studienpopulation unabhängig mit MACCE korreliert waren. Die Receiver-Operating-Curve(ROC)-Analyse ergab, dass ein LDL-Wert von mehr als 71 mg/dl ein Prädiktor für MACCE mit einer Sensitivität von 45,4 % und einer Spezifität von 91,8 % (AUC, Fläche unter der Kurve: 0,814; p = 0,02) war.
Schlussfolgerung
Die vorliegende Studie liefert Hinweise dafür, dass niedrigere Serumspiegel für LDL-C und HDL-C unabhängig mit kurzfristig auftretenden MACCE bei Patienten nach TAVI assoziiert sind. Niedrigere Spiegel für LDL-C und HDL-C sind möglicherweise Indikatoren einer schlechten Prognose. Die Bestimmung der Serumlipidspiegel könnte die präoperative Risikobeurteilung potenzieller TAVI-Kandidaten verbessern.
Similar content being viewed by others
Abbreviations
- DAPT:
-
Dual antiplatelet therapy
- HDL-C:
-
High-density lipoprotein cholesterol
- MACCE:
-
Major adverse cardiac and cerebrovascular events
- LDL-C:
-
Low-density lipoprotein cholesterol
- logistic EuroSCORE:
-
Logistic European System for Cardiac Operative Risk Evaluation
- RDW:
-
Red cell distribution width
- STS:
-
The Society of Thoracic Surgeons Predictive Risk of Mortality score
- TAVI:
-
Transcatheter aortic valve implantation
- WBC:
-
White blood cell
References
Lindman BR, Clavel M‑A, Mathieu P et al (2016) Calcific aortic stenosis. Nat Rev Dis Primers 2:16006
Eveborn GW, Schirmer H, Heggelund G et al (2013) The evolving epidemiology of valvular aortic stenosis. The Tromsø Study. Heart 99(6):396–400
Collas VM, Paelinck BP, Rodrigus IE et al (2016) Red cell distribution width improves the prediction of prognosis after transcatheter aortic valve implantation. Eur J Cardiothorac Surg 49(2):471–477
López-Otero D, Trillo-Nouche R, Gude F et al (2013) Pro B‑type natriuretic peptide plasma value: A new criterion for the prediction of short- and long-term outcomes after transcatheter aortic valve implantation. Int J Cardiol 168(2):1264–1268
Kleczynski P, Dziewierz A, Bagienski M et al (2017) Impact of frailty on mortality after transcatheter aortic valve implantation. Am Heart J 185:52–58
Schalk BWM, Visser M, Deeg DJH et al (2004) Lower levels of serum albumin and total cholesterol and future decline in functional performance in older persons: The Longitudinal Aging Study Amsterdam. Age Ageing 33(3):266–272
Reuben DB, Ix JH, Greendale GA et al (1999) The predictive value of combined hypoalbuminemia and hypocholesterolemia in high functioning community-dwelling older persons: MacArthur studies of successful aging. J Am Geriatr Soc 47(4):402–406
Félix-Redondo FJ, Grau M, Fernández-Bergés D (2013) Cholesterol and cardiovascular disease in the elderly. Facts and gaps. Aging Dis 4(3):154–169
Karataş MB, Güngör B, İpek G et al (2016) Association of serum cholesterol levels with short-term mortality in patients with acute pulmonary embolism. Heart Lung Circ 25(4):365–370
Kappetein AP, Head SJ, Généreux P et al (2012) Updated standardized endpoint definitions for transcatheter aortic valve implantation: the Valve Academic Research Consortium-2 consensus document. Eur Heart J 33(19):2403–2418
Clavel MA, Rodés-Cabau J, Dumont É et al (2011) Validation and characterization of transcatheter aortic valve effective orifice area measured by doppler echocardiography. JACC Cardiovasc Imaging 4(10):1053–1062
Zamorano JL, Badano LP, Bruce C et al (2011) EAE/ASE recommendations for the use of echocardiography in new transcatheter interventions for valvular heart disease. Eur Heart J 32(17):2189–2214
Weyman AE (2002) Exploring the relationship between hyperlipidemia and aortic stenosis. Rev Cardiovasc Med 3(3):160–161
Rossebø AB, Pedersen TR (2004) Hyperlipidaemia and aortic valve disease. Curr Opin Lipidol 15(4):447–451
Alsara O, Alsarah A, Laird-Fick H (2014) Advanced age and the clinical outcomes of transcatheter aortic valve implantation. J Geriatr Cardiol 11(2):163–170
Tarantini G, Mojoli M, Windecker S et al (2016) Prevalence and impact of atrial fibrillation in patients with severe aortic stenosis undergoing transcatheter aortic valve replacement: an analysis from the SOURCE XT prospective Multicenter registry. JACC Cardiovasc Interv 9(9):937–946
Amaranto DJ, Wang EC, Eskandari MK et al (2011) Normal preoperative white blood cell count is predictive of outcomes for endovascular procedures. J Vasc Surg 54(5):1395–1403
Rodés-Cabau J, Masson J‑B, Welsh RC et al (2017) Aspirin versus Aspirin plus clopidogrel as antithrombotic treatment following transcatheter aortic valve replacement with a balloon-expandable valve. JACC Cardiovasc Interv 10(13):1357–1365
Chakravarty T, Søndergaard L, Friedman J et al (2017) Subclinical leaflet thrombosis in surgical and transcatheter bioprosthetic aortic valves: an observational study. Lancet 389(10087):2383–2392
Silva LS, Caramori PRA, Nunes Filho ACB et al (2015) Performance of surgical risk scores to predict mortality after transcatheter aortic valve implantation. Arq Bras Cardiol. https://doi.org/10.5935/abc.20150084
Anand A, Harley C, Visvanathan A et al (2017) The relationship between preoperative frailty and outcomes following transcatheter aortic valve implantation: a systematic review and meta-analysis. Eur Heart J Qual Care Clin Outcomes 3(2):123–132
Yamamoto M, Hayashida K, Mouillet G et al (2013) Prognostic value of chronic kidney disease after transcatheter aortic valve implantation. J Am Coll Cardiol 62(10):869–877
Kefer J, Beauloye C, Astarci P et al (2010) Usefulness of B‑type natriuretic peptide to predict outcome of patients treated by transcatheter aortic valve implantation. Am J Cardiol 106(12):1782–1786
Teo KK, Corsi DJ, Tam JW et al (2011) Lipid lowering on progression of mild to moderate aortic stenosis: meta-analysis of the randomized placebo-controlled clinical trials on 2344 patients. Can J Cardiol 27(6):800–808
Myasoedova E, Crowson CS, Kremers HM et al (2011) Lipid paradox in rheumatoid arthritis: the impact of serum lipid measures and systemic inflammation on the risk of cardiovascular disease. Ann Rheum Dis 70(3):482–487
Velavan P, Huan Loh P, Clark A et al (2007) Congestive heart failure (Greenwich, Conn.). The cholesterol paradox in heart failure, vol 13, pp 336–341
Kahveci G, Bayrak F, Mutlu B et al (2008) Clinical significance of high-density lipoprotein cholesterol in left-sided infective Endocarditis. Am J Cardiol 101(8):1170–1173
Chien YF, Chen CY, Hsu CL et al (2015) Decreased serum level of lipoprotein cholesterol is a poor prognostic factor for patients with severe community-acquired pneumonia that required intensive care unit admission. J Crit Care 30(3):506–510
Fruchter O, Yigla M, Kramer MR (2015) Lipid profile and statin use: the paradox of survival after acute exacerbation of chronic obstructive pulmonary disease. Am J Med Sci 349(4):338–343
Cheng KH, Chu CS, Lin TH et al (2015) Lipid paradox in acute myocardial infarction-the association with 30-day in-hospital mortality. Crit Care Med 43(6):1255–1264
Le Couteur DG, Blyth FM, Creasey HM et al (2010) The association of alanine transaminase with aging, frailty, and mortality. J Gerontol A Biol Sci Med Sci 65(7):712–717
Wang X, Liao D, Bharadwaj U et al (2008) C‑reactive protein inhibits cholesterol efflux from human macrophage-derived foam cells. Arterioscler Thromb Vasc Biol 28(3):519–526
Feingold KR, Grunfeld C (2015) The Effect of Inflammation and Infection on Lipids and Lipoproteins. In: De Groot LJ et al (eds) Endotext, South Dartmouth (MA)
Klingenspor M, Ebbinghaus C, Hülshorst G et al (1996) Multiple regulatory steps are involved in the control of lipoprotein lipase activity in brown adipose tissue. J Lipid Res 37(8):1685–1695
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
N.S. Yelgeç and A. Emre declare that they have no competing interests.
For this article no studies with human participants or animals were performed by any of the authors. All studies performed were in accordance with the ethical standards indicated in each case. This retrospective study was performed after consultation with the institutional ethics committee and in accordance with national legal requirements.
Rights and permissions
About this article
Cite this article
Yelgeç, N.S., Emre, A. Prognostic value of lipid levels in short-term outcome after TAVI. Herz 45, 382–388 (2020). https://doi.org/10.1007/s00059-019-4826-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-019-4826-3
Keywords
- Transcatheter aortic valve implantation
- Frailty
- Prognosis
- High-density lipoprotein
- Low-density lipoprotein