Summary
Conclusions
The results of the present study suggest that the pancreas and parotid glands both respond with hypoplasia during absence of food in the digestive tract and with hyperplasia following pancreactico-biliary diversion (PBD). Factors other than cholecystokinin (CCK) are, however, involved in the effects on the parotid glands, since infusion of CCK-8S and devazepide was without influence.
Background and Aim
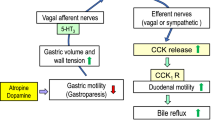
Total parenteral nutrition (TPN) causes reduced pancreatic weight, whereas PBD evokes hyperCCKemia and enlargement of the rat pancreas. The pancreas and parotid glands have in part similar morphology and function. Therefore, we studied the possible presence of alterations also in the parotid glands during TPN, after PBD and during infusion of sulfated cholecystokinin (CCK-8S) and the CCK-A receptor antagonist devazepide, respectively.
Materials and Results
Rats either received TPN for 7 d, or were kept under otherwise identical conditions with free access to food and water. TPN markedly reduced both pancreatic and parotid wet weight and thereby also the protein and amylase contents, and pancreatic DNA content was decreased. There was a significant correlation between the pancreas and parotid glands when comparing these parameters. The concentration of plasma CCK was unaffected by TPN. PBD caused a sevenfold increase in plasma CCK and a threefold increase in the pancreatic weight compared to control rats 28 d after the operation. The protein and DNA contents in the pancreas were found to be increased. The parotid glands increased twofold in weight, but their protein and amylase contents were not affected. There was a significant correlation between the pancreas and parotid glands when comparing weight, and protein and amylase concentrations. Infusion of CCK-8S during 28 d caused a marked increase in pancreatic wet wt and protein and DNA contents. The CCK-A receptor antagonist devazepide induced a reduction in protein and DNA contents in the pancreas. The parotid glands were not affected by either treatment. No effect on the labeling index of serous and ductal cells of the parotid gland was seen at 36 h, 3, 7, and 28 d of infusion with CCK-8S or devazepide.
Similar content being viewed by others
References
Young JA, Cook DI, van Lennep EW, Roberts M. Secretion of the major salivary glands, inPhysiology of the Gastrointestinal Tract, vol. 7, Johnson LR, ed., Raven, New York, 1987: pp. 73–815.
Skude G, Ihse I. Salivary amylase in duodenal aspirates.Scand J Gastroenterol 1976; 11: 17–20.
Lankisch PG, Otto J. Salivary isoamylase in duodenal aspirates.Dig Dis Sci 1986; 31: 1299–1302.
Axelson J, Hakanson R, Ihse I, Lija I, JRehfeld JF, Sundler F. Effects of endogenous cholecystokinin and of infusion with the cholecystokinin antagonist L-364,718 on pancreatic and gastro-intestinal growth.Scand J Gastroenterol 1990; 25: 471–480.
Saikatsu S, Ikeno K, Hanada Y, Ikeno T. Intravenous injection of cerulein or cholecystokinin increases the parotid-type amylase in the serum of rats. Shika Kiso Igakkai Zasshi 1989; 31: 592–596.
Grimmel K, Rossbach G, Kasper H. Amylase activity of parotid saliva in acute and chronic pancreatitis.Acta Hepatogastroenterol 1976; 23: 334–344.
Hirano T, Manabe T, Tobe T. Cellular alterations of parotid gland of rats with acute pancreatitis induced by cerulein.Int J Pancreatol 1991; 10: 217–227.
Miazza BM, Turberg Y, Guillaume P, Hahne W, Chayvialle JA, Loizeau E. Mechanism of pancreatic growth induced by pancreatico-biliary diversion in the rat.Scand J Gastroenterol 1985; 20: 75–83.
Fölsch UR, Cantor P, Wilms HM, Schafmayer A, Becker HD, Creutzfeldt W. Role of cholecystokinin in the negative feedback control of pancreatic enzyme secretion in conscious rats.Gastroenterology, 1987; 92: 449–458.
Hughes CA, Breuer RS, Ducker DA, Hatoff DE, Dowling RH. The effect of cholecystokinin and secretin on intestinal and pancreatic structure and function, inMechanisms of Intestinal Adaptation, Robinson JWL, Dowling RH, Riecken EO, eds., MTP, Lancaster, 1981: pp. 435–450.
Miazza BM, van Hung L, Vaja S, Dowling RH. Pancreatic hyperplasia after pancreatico biliary diversion (PBD) in orally and parenterally fed rats, inMechanisms of Intestinal Adaptation, Robinson JWL, Dowling RH, Riecken EO, eds., MTP, Lancaster, 1981: pp. 481–490.
Nylander AG, Chen D, Ihse I, Rehfeld JF, Håkanson R. Pancreatic atrophy in rats produced by the cholecystokinin-A receptor antagonist devazepide.Scand J Gastroenterol 1992; 27: 743–747.
Solomon TE, Yamada T, Elashoff J, Wood J, Beglinger C. Bioactivity of cholecystokinin analogues: CCK-8 is not more potent than CCK-33.Am J Physiol 1984; 253: 4016–4021.
Ohlsson B, Axelson J, Sternby B, Rehfeld JF, Ihse I. Time course of the pancreatic changes following long-term stimulation or inhibition of the CCK-A receptor.Int J Pancreatol 1995; 18: 59–66.
Rehfeld JF. Immunochemical studies on cholecystokinin. I. Development of sequence-specific radioimmunoassays for porcine triacontratriapeptide cholecystokinin.J Biol Chem 1978; 253: 4016–4021.
Cantor P. Evaluation of a radioimmunoassay for cholecystokinin in human plasma.Scand J Lab Invest 1986; 46: 213–221.
Lowry OH, Rosebrough NJ, Farr AL, Randall RJ. Protein measurement with the folin phenol reagent.J Biol Chem 1951; 193: 265–275.
Dahlqvist A. A method for the determination of amylase in intestinal content.Scand J Clin Lab Invest 1962; 14: 145–151.
Nagy I, Pap A, Varró V. Time-course of changes in pancreatic size and enzyme composition in rats during starvation.Int J Pancreatol 1989; 5: 35–45.
Iovanna JL, Dusetti NJ, Cadenas MB, Mallmann MC, Calco EL. Changes in pancreatic trophism and gene expression during a prolonged fasting period in rats.Int J Pancreatol 1991; 8: 177–186.
Koop I, Kimmich T, Koop H, Armold R. Effect of food deprivation on the function of intestinal cholecystokinin-producing cell in the rat.Digestion 1987; 38: 114–123.
Nealon WH, Upp JR, Jr., Alexander RW, Gomez G, Townsend CM, Thompson JC. Intravenous amino acids induce human gallbladder contraction.Am J Physiol 1990; 259: G173-G178.
Adler G, Beglinger C, Braun U, Reinshagen M, Koop I, Schafmayer A, Rovati L, Arnold R. Interaction of the cholinergic system and cholecystokinin in the regulation of endogenous and exogenous stimulation of pancreatic secretion in humans.Gastroenterology 1991; 100: 537–543.
Schneyer CA, Hall HD. Amylase and electrolyte changes after postganglionic parasympathectomy of parotid gland.Am J Physiol 1964; 207: 308–312.
Jaworek J, Konturek SJ, Bielanski W, Bilski J, Hladij M. Release and binding of epidermal growth factor in the pancreas of rats.Int J Pancreatol 1992; 11: 19–17.
Ino M, Ushiro K, Ino C, Yamashita T, Kumazawa T. Kinetics of epidermal growth factor in saliva.Acta Otolaryngol Suppl Stockh 1993; 500: 126–130.
Dembinski A, Gregory H, Konturek SJ, Polanski M. Trophic action of epidermal growth factor on the pancreas and gastrointestinal mucosa in rats.J Physiol 1982; 325: 35–42.
Ohlsson B, Jansen C, Ihse I, Axelson J. Epidermal growth factor induces cell proliferation in mouse pancreas and salivary glands.Pancreas 1996, in press.
Gasslander T, Chu M, Smeds S, Ihse I. Proliferative response of different exocrine pancreatic cells following surgical pancreatico-biliary diversion.Scand J Gastroenterol 1991; 26: 399–404.
Chu M, Borch K, Lilja I, Blomqvist, Rehfeld JF, Ihse I. Endogenous hypercholecystokininemia model in the hamster: trophic effect on the exocrine pancreas.Pancreas 1992; 7: 220–225.
Gasslander T, Axelson J, Håkanson R, Ihse I, Lilja I, Rehfeld JF. Cholecystokinin is responsible for growth of the pancreas following pancreatico-biliary diversion in rats.Scand J Gastroenterol 1990; 25: 1060–1065.
Schick J, Kern H, Scheele G. Hormonal stimulation in the exocrine pancreas results in coordinate and anticoordinate regulation of protein synthesis.J Cell Biol 1984; 99: 1569–1574.
Fölsch UR, Winckler K, Wormsley KG. Influence of repeated administration of cholecystokinin and secretin on the pancreas of the rat.Scand J Gastroenterol 1978; 13: 663–671.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Axelson, J., Fan, B.G., Ohlsson, B. et al. The changes in the rat parotid glands following total parenteral nutrition and pancreatico-biliary diversion are not mediated by cholecystokinin. Int J Pancreatol 20, 109–118 (1996). https://doi.org/10.1007/BF02825509
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF02825509