Abstract
Objective
To evaluate the sensitivity, specificity and overall accuracy of a model based on the presence or absence of organ dysfunctions and/or infection (ODIN) to predict the outcome for intensive care unit patients.
Design
Prospective study.
Setting
General intensive care unit in a university teaching hospital.
Patients
1070 consecutive, unselected patients.
Interventions
There were no interventions.
Measurements and main results
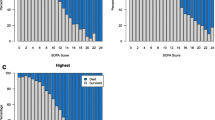
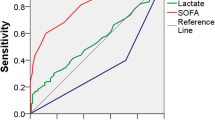
We recorded within the first 24h of admission the presence or absence of dysfunction in 6 organ systems: respiratory, cardiovascular, renal, hematologic, hepatic and neurologic, and/or infection (ODIN) in all patients admitted to our ICU, thus establishing a profile of organ dysfunctions in each patient. Using univariate analysis, a strong correlation was found between the number of ODIN and the death rate (2.6, 9.7, 16.7, 32.3, 64.9, 75.9, 94.4 and 100% for 0, 1, 2, 3, 4, 5, 6 and 7 ODIN, respectively; (p<0.001). In addition, the highest mortality rates were associated with hepatic (60.8%), hematologic (58.1%) and renal (54.8%) dysfunctions, and the lowest with respiratory dysfunction (36.5%) and infection (38.3%). For taking into account both the number and the type of organ dysfunction, a logistic regression model was then used to calculate individual probabilities of death that depended upon the statistical weight assigned to each ODIN (in the following order of descending severity: cardiovascular, renal, respiratory, neurologic, hematologic, hepatic dysfunctions and infection). The ability of this severity-of-disease classification system to stratify a wide variety of patients prognostically (sensitivity 51.4%, specificity 93.4%, overall accuracy 82.1%) was not different from that of currently used scoring systems.
Conclusions
These findings suggest that determination of the number and the type of organ dysfunctions and infection offers a clear and reliable method for characterizing ICU patients. Before a widespread use, this model requires to be validated in other institutions.
Similar content being viewed by others
References
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) Apache II: a severity of disease classification system. Crit Care Med 13:818–829
Le Gall JR; Loirat P, Alperovitch et al (1984) A simplified acute physiology score for ICU patients. Crit Care Med 12:975–977
Lemeshow S, Teres D, Pastides H, Aurunin JS, Steingrub JS (1985) A method predicting survical and mortality of ICU patients using objectively derived weights. Crit Care Med 13:519–525
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) Prognosis in acute organ-system failure. Ann Surg 202:689–693
Baue AE (1975) Multiple progressive or sequential system failure: a syndrome of the 1970's. Arch Surg 110:779
Bell RC, Coalson JJ, Smith JD, Johanson WG Jr (1983) Multiple organ system failure and infection in adult respiratory distress syndrome. Ann Intern Med 99:293–298
Chang RWS, Jacobs S, Lee B (1988) Predicting outcome among intensive care unit patients using computerised trend analysis of daily Apache II scores corrected for organ system failure. Intensive Care Med 14:558–566
McCabe WR, Jackson GG (1982) Gram-negative bactermia. I. Etiology and ecology. Arch Intern Med 110:847–864
Fry DE, Pearlstein L, Fulton RL, Hiram CP (1980) Multiple system organ failure: the role of uncontrolled infection. Arch Surg 115:136–140
Stevens LE (1983) Gauging the severity of surgical sepsis. Arch Surg 118:1190–1192
Jordan DA, Miller CF, Kubos KL, Rogers MC (1987) Evaluation of sepsis in a critically ill surgical population. Crit Care Med 15:897–904
Bihari D, Smithies M, Gimson A, Tinker J (1987) The effects of vasodilatation with prostacyclin on oxygen delivery and uptake in critically ill patients. N Engl J Med 17:397–403
Teasdale G, Jennett B (1974) Assessment of coma and impaired consciousness. A practicable scale. Lancet II:81–84
Hanley JA, McNeil BJ (1983) A method of comparing the areas under receiving operating characteristic curves derived from the same cases. Radiology 148:839–843
Matuschack GM, Rinaldo JE, Pinksy MR et al (1987) Effect of endstage liver failure on the incidence and resolution of the adult respiratory distress syndrome. J Crit Care 2:162–173
Pepe PE, Potkin RT, Reus DH, Hudson LD, Carrico CJ (1982) Clinical predictors of the adult respicatory distress syndrome. Am J Surg 144:124–129
Knaus WA, Le Gall JR, Wagner DP et al (1982) A comparison of intensive care in the USA and France. Lancet II:642–646
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1986) An evaluation of outcome from intensive care in major medical centers. Ann Intern Med 104:410–418
Lemeshow S, Teres D, Aurunin JS, Partides H (1987) A comparison of methods to predict mortality of intensive care unit patients. Crit Care Med 15:715–722
Castella X, Gilabert J, Torner F, Torres C (1991) Mortality prediction models in intensive care: acute physiology and chronic health evaluation II and mortality prediction model compared. Crit Care Med 19:191–197
Ruttimann UE, Pollack MM (1991) Objective assessment of changing mortality risks in pediatric intensive care unit patients. Crit Care Med 19:474–483
Dubois RW, Rogers WH, Moxley JH, Draper D, Brook RH (1987) Hospital inpatient mortality. Is it a prediction of quality? N Engl J Med 317:1674–1679
Couch JB, Nash DB (1988) Severity of illness measures: opportunities for clinicians. Ann Intern Med 109:771–773
Knaus WA, Wagner DP, Drapper EA et al (1991) The Apache III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest 100:1619–1636
Author information
Authors and Affiliations
Additional information
Supported in part by a grant from the Faculté Xavier-Bichat and the Direction Générale de la Santé
Rights and permissions
About this article
Cite this article
Fagon, J.Y., Chastre, J., Novara, A. et al. Characterization of intensive care unit patients using a model based on the presence or absence of organ dysfunctions and/or infection: The ODIN model. Intensive Care Med 19, 137–144 (1993). https://doi.org/10.1007/BF01720528
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF01720528