Abstract
Cellular plasticity, by large, is the ability through which cells morph into new phenotypic identity by trading-off with the previous one. This phenomenon has been observed in the normal and tumor cells in a very similar fashion. Occurrence of cellular plasticity, in malignancies like epithelial ovarian carcinoma (EOC) are well known but highly debated in terms of origin of the tumor for the inherent heterogeneity across subtypes. EOC has been termed as a clinically challenging malady for its subversive nature against chemotherapy. The management of ovarian cancer is mostly hindered by relapse with recalcitrance towards primary chemotherapy regimen e.g. platinum–taxol combination. Also, late detection preceded by peritoneal metastasis poses another challenge to the treatment. Underlying both these aspects of the disease, tumor heterogeneity turns out as the most critical factor. In the light of heterogeneity that can be across patients (inter-tumoral) and/or within a tumor (intra-tumoral), ovarian carcinoma is a multifactorial ailment. The governing factors behind this heterogeneity are—diverse genetic landscape among subtypes of EOC; the presence of cancer stem cell (CSC) niche and inherent plasticity of the cancer cells themselves. Apart from the well-studied mechanisms of plasticity, there are several emerging molecular players like lncRNAs, Hippo pathway and also phenomena like dedifferentiation of non-CSC neoplastic cells ,and transdifferentiation of CSCs. Here, we present an overview of the current knowledge on the evolution of EOC through cellular plasticity with emphasis on the three major aspects namely, subtype-specific genetic diversity; ovarian CSC and cancer cell duality between epithelial and mesenchymal lineages.


Similar content being viewed by others
References
Blau HM (2014) Sir John Gurdon: father of nuclear reprogramming. Differentiation 88:10–12. https://doi.org/10.1016/j.diff.2014.05.002
Ge Y, Fuchs E (2018) Stretching the limits: from homeostasis to stem cell plasticity in wound healing and cancer. Nat Rev Genet 19:311–325. https://doi.org/10.1038/nrg.2018.9
Truman AM, Tilly JL, Woods DC (2017) Ovarian regeneration: the potential for stem cell contribution in the postnatal ovary to sustained endocrine function. Mol Cell Endocrinol 445:74–84. https://doi.org/10.1016/j.mce.2016.10.012
Vibert L, Daulny A, Jarriault S (2018) Wound healing, cellular regeneration and plasticity: the elegans way. Int J Dev Biol 62:491–505. https://doi.org/10.1387/ijdb.180123sj
Carter LE, Cook DP, Vanderhyden BC (2019) In: Leung PCK, Adashi EY (eds) The ovary, 3rd edn. Academic Press, pp 529–545
Baylin SB, Jones PA (2011) A decade of exploring the cancer epigenome—biological and translational implications. Nat Rev Cancer 11:726–734. https://doi.org/10.1038/nrc3130
Meacham CE, Morrison SJ (2013) Tumour heterogeneity and cancer cell plasticity. Nature 501:328–337. https://doi.org/10.1038/nature12624
Anderson AR, Weaver AM, Cummings PT, Quaranta V (2006) Tumor morphology and phenotypic evolution driven by selective pressure from the microenvironment. Cell 127:905–915. https://doi.org/10.1016/j.cell.2006.09.042
Tian H et al (2011) A reserve stem cell population in small intestine renders Lgr5-positive cells dispensable. Nature 478:255–259. https://doi.org/10.1038/nature10408
Rompolas P, Mesa KR, Greco V (2013) Spatial organization within a niche as a determinant of stem-cell fate. Nature 502:513–518. https://doi.org/10.1038/nature12602
Hoeck JD et al (2017) Stem cell plasticity enables hair regeneration following Lgr5(+) cell loss. Nat Cell Biol 19:666–676. https://doi.org/10.1038/ncb3535
Merrell AJ, Stanger BZ (2016) Adult cell plasticity in vivo: de-differentiation and transdifferentiation are back in style. Nat Rev Mol Cell Biol 17:413–425. https://doi.org/10.1038/nrm.2016.24
Ito M et al (2007) Wnt-dependent de novo hair follicle regeneration in adult mouse skin after wounding. Nature 447:316–320. https://doi.org/10.1038/nature05766
Bray F et al (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424. https://doi.org/10.3322/caac.21492
Wu SG et al (2019) Real-world impact of survival by period of diagnosis in epithelial ovarian cancer between 1990 and 2014. Front Oncol 9:639. https://doi.org/10.3389/fonc.2019.00639
Auersperg N, Wong AST, Choi K-C, Kang SK, Leung PCK (2001) Ovarian surface epithelium: biology, endocrinology, and pathology. Endocr Rev 22:255–288. https://doi.org/10.1210/edrv.22.2.0422
Ahmed N, Thompson EW, Quinn MA (2007) Epithelial–mesenchymal interconversions in normal ovarian surface epithelium and ovarian carcinomas: an exception to the norm. J Cell Physiol 213:581–588. https://doi.org/10.1002/jcp.21240
Levanon K, Crum C, Drapkin R (2008) New insights into the pathogenesis of serous ovarian cancer and its clinical impact. J Clin Oncol 26:5284–5293. https://doi.org/10.1200/JCO.2008.18.1107
Salvador S et al (2009) The fallopian tube: primary site of most pelvic high-grade serous carcinomas. Int J Gynecol Cancer 19:58–64. https://doi.org/10.1111/IGC.0b013e318199009c
Carter LE, Cook DP, Vanderhyden BC (2019) Phenotypic plasticity and the origins and progression of ovarian cancer. Ovary. https://doi.org/10.1016/b978-0-12-813209-8.00033-9
Auersperg N (2011) The origin of ovarian carcinomas: a unifying hypothesis. Int J Gynecol Pathol 30:12–21. https://doi.org/10.1097/PGP.0b013e3181f45f3e
Erickson BK, Conner MG, Landen CN Jr (2013) The role of the fallopian tube in the origin of ovarian cancer. Am J Obstet Gynecol 209:409–414. https://doi.org/10.1016/j.ajog.2013.04.019
Jarboe EA et al (2009) Tubal and ovarian pathways to pelvic epithelial cancer: a pathological perspective. Histopathology 55:619. https://doi.org/10.1111/j.1365-2559.2009.03408.x
Chen VW et al (2003) Pathology and classification of ovarian tumors. Cancer 97:2631–2642. https://doi.org/10.1002/cncr.11345
Kurman RJ, Shih I-M (2010) The origin and pathogenesis of epithelial ovarian cancer: a proposed unifying theory. Am J Surg Pathol 34:433–443. https://doi.org/10.1097/PAS.0b013e3181cf3d79
The Cancer Genome Atlas Research, N et al (2011) Integrated genomic analyses of ovarian carcinoma. Nature 474:609. doi: 10.1038/nature10166. https://www.nature.com/articles/nature10166#supplementary-information
Berns EMJJ, Bowtell DD (2012) The changing view of high-grade serous ovarian cancer. Cancer Res 72:2701–2704. https://doi.org/10.1158/0008-5472.can-11-3911
Cancer Genome Atlas Research, N (2011) Integrated genomic analyses of ovarian carcinoma. Nature 474:609–615. https://doi.org/10.1038/nature10166
Verhaak RG et al (2013) Prognostically relevant gene signatures of high-grade serous ovarian carcinoma. J Clin Invest 123:517–525. https://doi.org/10.1172/JCI65833
Tothill RW et al (2008) Novel molecular subtypes of serous and endometrioid ovarian cancer linked to clinical outcome. Clin Cancer Res 14:5198–5208. https://doi.org/10.1158/1078-0432.CCR-08-0196
Ince TA et al (2015) Characterization of twenty-five ovarian tumour cell lines that phenocopy primary tumours. Nat Commun 6:7419. https://doi.org/10.1038/ncomms8419
Hirst J, Crow J, Godwin A (2018) Ovarian cancer genetics: subtypes and risk factors. Ovarian Cancer Pathog Treat. https://doi.org/10.5772/intechopen.72705
Smith Sehdev AE, Sehdev PS, Kurman RJ (2003) Noninvasive and invasive micropapillary (low-grade) serous carcinoma of the ovary: a clinicopathologic analysis of 135 cases. Am J Surg Pathol 27:725–736. https://doi.org/10.1097/00000478-200306000-00003
Malpica A et al (2004) Grading ovarian serous carcinoma using a two-tier system. Am J Surg Pathol 28:496–504. https://doi.org/10.1097/00000478-200404000-00009
Singer G, Shih Ie M, Truskinovsky A, Umudum H, Kurman RJ (2003) Mutational analysis of K-ras segregates ovarian serous carcinomas into two types: invasive MPSC (low-grade tumor) and conventional serous carcinoma (high-grade tumor). Int J Gynecol Pathol 22:37–41. https://doi.org/10.1097/00004347-200301000-00009
Vang R, Shih Ie M, Kurman RJ (2009) Ovarian low-grade and high-grade serous carcinoma: pathogenesis, clinicopathologic and molecular biologic features, and diagnostic problems. Adv Anat Pathol 16:267–282. https://doi.org/10.1097/PAP.0b013e3181b4fffa
Parker RL, Clement PB, Chercover DJ, Sornarajah T, Gilks CB (2004) Early recurrence of ovarian serous borderline tumor as high-grade carcinoma: a report of two cases. Int J Gynecol Pathol 23:265–272. https://doi.org/10.1097/01.pgp.0000130049.19643.f6
Kurman RJ, Craig JM (1972) Endometrioid and clear cell carcinoma of the ovary. Cancer 29:1653–1664. https://doi.org/10.1002/1097-0142(197206)29:6%3c1653:aid-cncr2820290633%3e3.0.co;2-e
Terada T (2012) Endometrioid adenocarcinoma of the ovary arising in atypical endometriosis. Int J Clin Exp Pathol 5:924–927
Xy J, Wp Z, Mf W (2017) The clinical characteristics and prognosis of ovarian endometrioid carcinoma. Integr Cancer Sci Ther. https://doi.org/10.15761/icst.1000239
Hollis RL, Gourley C (2016) Genetic and molecular changes in ovarian cancer. Cancer Biol Med 13:236–247. https://doi.org/10.20892/j.issn.2095-3941.2016.0024
Bell DA (2005) Origins and molecular pathology of ovarian cancer. Mod Pathol 18:S19–S32. https://doi.org/10.1038/modpathol.3800306
Gilks CB (2010) Molecular abnormalities in ovarian cancer subtypes other than high-grade serous carcinoma. J Oncol 740968–740968:2010. https://doi.org/10.1155/2010/740968
Cheasley D et al (2019) The molecular origin and taxonomy of mucinous ovarian carcinoma. Nat Commun 10:3935–3935. https://doi.org/10.1038/s41467-019-11862-x
Lupia M, Cavallaro U (2017) Ovarian cancer stem cells: still an elusive entity? Mol Cancer 16:64
Abdullah LN, Chow EK-H (2013) Mechanisms of chemoresistance in cancer stem cells. Clin Transl Med 2:3
Clevers H (2011) The cancer stem cell: premises, promises and challenges. Nat Med 17:313
Bapat SA, Mali AM, Koppikar CB, Kurrey NK (2005) Stem and progenitor-like cells contribute to the aggressive behavior of human epithelial ovarian cancer. Can Res 65:3025–3029
Alvero AB et al (2009) Molecular phenotyping of human ovarian cancer stem cells unravels the mechanisms for repair and chemoresistance. Cell Cycle 8:158–166. https://doi.org/10.4161/cc.8.1.7533
Hu L, McArthur C, Jaffe RB (2010) Ovarian cancer stem-like side-population cells are tumourigenic and chemoresistant. Br J Cancer 102:1276–1283. https://doi.org/10.1038/sj.bjc.6605626
Boesch M, Wolf D, Sopper S (2016) Optimized stem cell detection using the dyecycle-triggered side population phenotype. Stem Cells Int 2016:1652389. https://doi.org/10.1155/2016/1652389
Landen CN et al (2010) Targeting aldehyde dehydrogenase cancer stem cells in ovarian cancer. Mol Cancer Ther 9:3186–3199
Zhang S et al (2008) Identification and characterization of ovarian cancer-initiating cells from primary human tumors. Cancer Res 68:4311–4320. https://doi.org/10.1158/0008-5472.CAN-08-0364
Slomiany MG et al (2009) Inhibition of functional hyaluronan-CD44 interactions in CD133-positive primary human ovarian carcinoma cells by small hyaluronan oligosaccharides. Clin Cancer Res 15:7593–7601. https://doi.org/10.1158/1078-0432.CCR-09-2317
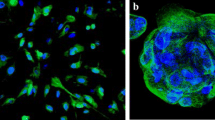
Latifi A et al (2012) Isolation and characterization of tumor cells from the ascites of ovarian cancer patients: molecular phenotype of chemoresistant ovarian tumors. PLoS ONE 7:e46858. https://doi.org/10.1371/journal.pone.0046858
Zhang S et al (2014) Ovarian cancer stem cells express ROR1, which can be targeted for anti-cancer-stem-cell therapy. Proc Natl Acad Sci USA 111:17266–17271. https://doi.org/10.1073/pnas.1419599111
Ruan Z, Yang X, Cheng W (2019) OCT4 accelerates tumorigenesis through activating JAK/STAT signaling in ovarian cancer side population cells. Cancer Manag Res 11:389–399. https://doi.org/10.2147/CMAR.S180418
Wen Y, Hou Y, Huang Z, Cai J, Wang Z (2017) SOX2 is required to maintain cancer stem cells in ovarian cancer. Cancer Sci 108:719–731. https://doi.org/10.1111/cas.13186
Pan Y et al (2010) Nanog is highly expressed in ovarian serous cystadenocarcinoma and correlated with clinical stage and pathological grade. Pathobiology J Immunopathol Mol Cell Biol 77:283–288. https://doi.org/10.1159/000320866
Kobayashi Y et al (2011) Side population is increased in paclitaxel-resistant ovarian cancer cell lines regardless of resistance to cisplatin. Gynecol Oncol 121:390–394. https://doi.org/10.1016/j.ygyno.2010.12.366
Wang A, Chen L, Li C, Zhu Y (2015) Heterogeneity in cancer stem cells. Cancer Lett 357:63–68. https://doi.org/10.1016/j.canlet.2014.11.040
Tang DG (2012) Understanding cancer stem cell heterogeneity and plasticity. Cell Res 22:457–472. https://doi.org/10.1038/cr.2012.13
Singh RK, Dhadve A, Sakpal A, De A, Ray P (2016) An active IGF-1R-AKT signaling imparts functional heterogeneity in ovarian CSC population. Sci Rep 6:36612
Cabrera MC, Hollingsworth RE, Hurt EM (2015) Cancer stem cell plasticity and tumor hierarchy. World J Stem Cells 7:27–36. https://doi.org/10.4252/wjsc.v7.i1.27
Boesch M et al (1866) Heterogeneity of cancer stem cells: rationale for targeting the stem cell niche. Biochem Biophys Acta 276–289:2016. https://doi.org/10.1016/j.bbcan.2016.10.003
Abelson S et al (2012) Intratumoral heterogeneity in the self-renewal and tumorigenic differentiation of ovarian cancer. Stem Cells 30:415–424
Cui T et al (2018) DDB2 represses ovarian cancer cell dedifferentiation by suppressing ALDH1A1. Cell Death Dis 9:561
Liu KC et al (2013) Ovarian cancer stem-like cells show induced translineage-differentiation capacity and are suppressed by alkaline phosphatase inhibitor. Oncotarget 4:2366–2382. https://doi.org/10.18632/oncotarget.1424
Ramakrishnan M, Mathur SR, Mukhopadhyay A (2013) Fusion-derived epithelial cancer cells express hematopoietic markers and contribute to stem cell and migratory phenotype in ovarian carcinoma. Cancer Res 73:5360–5370. https://doi.org/10.1158/0008-5472.CAN-13-0896
Kalluri R, Weinberg RA (2009) The basics of epithelial-mesenchymal transition. J Clin Invest 119:1420–1428. https://doi.org/10.1172/JCI39104
Gupta S, Maitra A (2016) EMT: matter of life or death? Cell 164:840–842. https://doi.org/10.1016/j.cell.2016.02.024
Klymenko Y, Kim O, Stack MS (2017) Complex determinants of epithelial: mesenchymal phenotypic plasticity in ovarian cancer. Cancers (Basel). https://doi.org/10.3390/cancers9080104
Jackstadt R et al (2019) Epithelial NOTCH signaling rewires the tumor microenvironment of colorectal cancer to drive poor-prognosis subtypes and metastasis. Cancer Cell 36:319–336 e317. https://doi.org/10.1016/j.ccell.2019.08.003
Yao D, Dai C, Peng S (2011) Mechanism of the mesenchymal-epithelial transition and its relationship with metastatic tumor formation. Mol Cancer Res 9:1608–1620. https://doi.org/10.1158/1541-7786.MCR-10-0568
Pastushenko I et al (2018) Identification of the tumour transition states occurring during EMT. Nature 556:463–468. https://doi.org/10.1038/s41586-018-0040-3
Guadamillas MC, Cerezo A, Del Pozo MA (2011) Overcoming anoikis–pathways to anchorage-independent growth in cancer. J Cell Sci 124:3189–3197. https://doi.org/10.1242/jcs.072165
Ahmed N, Abubaker K, Findlay J, Quinn M (2010) Epithelial mesenchymal transition and cancer stem cell-like phenotypes facilitate chemoresistance in recurrent ovarian cancer. Curr Cancer Drug Targets 10:268–278. https://doi.org/10.2174/156800910791190175
Loret N, Denys H, Tummers P, Berx G (2019) The role of epithelial-to-mesenchymal plasticity in ovarian cancer progression and therapy resistance. Cancers (Basel). https://doi.org/10.3390/cancers11060838
Alwosaibai K et al (2017) PAX2 maintains the differentiation of mouse oviductal epithelium and inhibits the transition to a stem cell-like state. Oncotarget 8:76881–76897. https://doi.org/10.18632/oncotarget.20173
Dean M, Davis DA, Burdette JE (2017) Activin A stimulates migration of the fallopian tube epithelium, an origin of high-grade serous ovarian cancer, through non-canonical signaling. Cancer Lett 391:114–124. https://doi.org/10.1016/j.canlet.2017.01.011
Newsted D et al (2019) Blockade of TGF-beta signaling with novel synthetic antibodies limits immune exclusion and improves chemotherapy response in metastatic ovarian cancer models. Oncoimmunology 8:e1539613. https://doi.org/10.1080/2162402X.2018.1539613
Tan DSP, Agarwal R, Kaye SB (2006) Mechanisms of transcoelomic metastasis in ovarian cancer. Lancet Oncol 7:925–934. https://doi.org/10.1016/S1470-2045(06)70939-1
Pradeep S et al (2014) Hematogenous metastasis of ovarian cancer: rethinking mode of spread. Cancer Cell 26:77–91. https://doi.org/10.1016/j.ccr.2014.05.002
Al Habyan S, Kalos C, Szymborski J, McCaffrey L (2018) Multicellular detachment generates metastatic spheroids during intra-abdominal dissemination in epithelial ovarian cancer. Oncogene 37:5127–5135. https://doi.org/10.1038/s41388-018-0317-x
Li G et al (2018) Frizzled7 promotes epithelial-to-mesenchymal transition and stemness via activating canonical Wnt/beta-catenin pathway in gastric cancer. Int J Biol Sci 14:280–293. https://doi.org/10.7150/ijbs.23756
Chen Y et al (2019) WFDC2 contributes to epithelial-mesenchymal transition (EMT) by activating AKT signaling pathway and regulating MMP-2 expression. Cancer Manag Res 11:2415–2424. https://doi.org/10.2147/CMAR.S192950
Westermann AM et al (1998) Malignant effusions contain lysophosphatidic acid (LPA)-like activity. Ann Oncol 9:437–442. https://doi.org/10.1023/a:1008217129273
Sutphen R et al (2004) Lysophospholipids are potential biomarkers of ovarian cancer. Cancer Epidemiol Biomark Prev 13:1185–1191
Sadlecki P et al (2019) Expression of zinc finger transcription factors (ZNF143 and ZNF281) in serous borderline ovarian tumors and low-grade ovarian cancers. J Ovarian Res 12:23. https://doi.org/10.1186/s13048-019-0501-9
Sadlecki P, Jozwicki J, Antosik P, Grabiec M (2018) Expression of selected epithelial-mesenchymal transition transcription factors in serous borderline ovarian tumors and type I ovarian cancers. Tumour Biol 40:1010428318784807. https://doi.org/10.1177/1010428318784807
Cheng JC, Auersperg N, Leung PC (2011) Inhibition of p53 induces invasion of serous borderline ovarian tumor cells by accentuating PI3K/Akt-mediated suppression of E-cadherin. Oncogene 30:1020–1031. https://doi.org/10.1038/onc.2010.486
Moffitt L, Karimnia N, Stephens A, Bilandzic M (2019) Therapeutic targeting of collective invasion in ovarian cancer. Int J Mol Sci. https://doi.org/10.3390/ijms20061466
Qian B-Z et al (2015) FLT1 signaling in metastasis-associated macrophages activates an inflammatory signature that promotes breast cancer metastasis. J Exp Med 212:1433–1448. https://doi.org/10.1084/jem.20141555
Terabe M et al (2003) Transforming growth factor-beta production and myeloid cells are an effector mechanism through which CD1d-restricted T cells block cytotoxic T lymphocyte-mediated tumor immunosurveillance: abrogation prevents tumor recurrence. J Exp Med 198:1741–1752. https://doi.org/10.1084/jem.20022227
Vander Griend DJ et al (2005) Suppression of metastatic colonization by the context-dependent activation of the c-Jun NH2-terminal kinase kinases JNKK1/MKK4 and MKK7. Can Res 65:10984. https://doi.org/10.1158/0008-5472.CAN-05-2382
Kurrey NK et al (2009) Snail and slug mediate radioresistance and chemoresistance by antagonizing p53-mediated apoptosis and acquiring a stem-like phenotype in ovarian cancer cells. Stem Cells 27:2059–2068. https://doi.org/10.1002/stem.154
He P, Qiu K, Jia Y (2018) Modeling of mesenchymal hybrid epithelial state and phenotypic transitions in EMT and MET processes of cancer cells. Sci Rep 8:14323. https://doi.org/10.1038/s41598-018-32737-z
Strauss R et al (2011) Analysis of epithelial and mesenchymal markers in ovarian cancer reveals phenotypic heterogeneity and plasticity. PLoS ONE 6:e16186. https://doi.org/10.1371/journal.pone.0016186
Jolly MK et al (2018) Interconnected feedback loops among ESRP1, HAS2, and CD44 regulate epithelial-mesenchymal plasticity in cancer. APL Bioeng 2:031908–031908. https://doi.org/10.1063/1.5024874
Bracken CP et al (2008) A double-negative feedback loop between ZEB1-SIP1 and the microRNA-200 family regulates epithelial-mesenchymal transition. Cancer Res 68:7846–7854. https://doi.org/10.1158/0008-5472.can-08-1942
Siemens H et al (2011) miR-34 and SNAIL form a double-negative feedback loop to regulate epithelial-mesenchymal transitions. Cell Cycle 10:4256–4271. https://doi.org/10.4161/cc.10.24.18552
Hu Z et al (2019) The repertoire of serous ovarian cancer non-genetic heterogeneity revealed by single-cell sequencing of normal fallopian tube epithelial cells. bioRxiv 672626. doi:10.1101/672626
Varankar SS et al (2019) Functional balance between Tcf21–Slug defines cellular plasticity and migratory modalities in high grade serous ovarian cancer cell lines. Carcinogenesis. https://doi.org/10.1093/carcin/bgz119
Jolly MK, Kulkarni P, Weninger K, Orban J, Levine H (2018) Phenotypic plasticity, bet-hedging, and androgen independence in prostate cancer: role of non-genetic heterogeneity. Front Oncol 8:50–50. https://doi.org/10.3389/fonc.2018.00050
Moyed HS, Bertrand KP (1983) hipA, a newly recognized gene of Escherichia coli K-12 that affects frequency of persistence after inhibition of murein synthesis. J Bacteriol 155:768–775
Sharma SV et al (2010) A chromatin-mediated reversible drug-tolerant state in cancer cell subpopulations. Cell 141:69–80. https://doi.org/10.1016/j.cell.2010.02.027
Beaumont HJE, Gallie J, Kost C, Ferguson GC, Rainey PB (2009) Experimental evolution of bet hedging. Nature 462:90–93. https://doi.org/10.1038/nature08504
Yang Q et al (2018) Analysis of LncRNA expression in cell differentiation. RNA Biol 15:413–422. https://doi.org/10.1080/15476286.2018.1441665
Li C, Hu G, Wei B, Wang L, Liu N (2019) lncRNA LINC01494 promotes proliferation, migration and invasion in glioma through miR-122-5p/CCNG1 axis. Onco Targets Ther 12:7655–7662. https://doi.org/10.2147/OTT.S213345
Rossi MN, Antonangeli F (2014) LncRNAs: new players in apoptosis control. Int J Cell Biol 2014:473857. https://doi.org/10.1155/2014/473857
Zhou M et al (2016) Comprehensive analysis of lncRNA expression profiles reveals a novel lncRNA signature to discriminate nonequivalent outcomes in patients with ovarian cancer. Oncotarget 7:32433–32448. https://doi.org/10.18632/oncotarget.8653
Xia B et al (2017) Long non-coding RNA ZFAS1 interacts with miR-150-5p to regulate Sp1 expression and ovarian cancer cell malignancy. Oncotarget 8:19534–19546. https://doi.org/10.18632/oncotarget.14663
Qiu JJ et al (2014) Overexpression of long non-coding RNA HOTAIR predicts poor patient prognosis and promotes tumor metastasis in epithelial ovarian cancer. Gynecol Oncol 134:121–128. https://doi.org/10.1016/j.ygyno.2014.03.556
Richards EJ et al (2015) Long non-coding RNAs (LncRNA) regulated by transforming growth factor (TGF) beta: LncRNA-hit-mediated TGFbeta-induced epithelial to mesenchymal transition in mammary epithelia. J Biol Chem 290:6857–6867. https://doi.org/10.1074/jbc.M114.610915
Xia Y et al (2014) YAP promotes ovarian cancer cell tumorigenesis and is indicative of a poor prognosis for ovarian cancer patients. PLoS ONE 9:e91770. https://doi.org/10.1371/journal.pone.0091770
Hall CA et al (2010) Hippo pathway effector Yap is an ovarian cancer oncogene. Cancer Res 70:8517–8525. https://doi.org/10.1158/0008-5472.CAN-10-1242
Wu X et al (2018) Sialyltransferase ST3GAL1 promotes cell migration, invasion, and TGF-beta1-induced EMT and confers paclitaxel resistance in ovarian cancer. Cell Death Dis 9:1102. https://doi.org/10.1038/s41419-018-1101-0
Zhang M et al (2019) Pyruvate dehydrogenase kinase 1 contributes to cisplatin resistance of ovarian cancer through EGFR activation. J Cell Physiol 234:6361–6370. https://doi.org/10.1002/jcp.27369
Tung SL et al (2017) miRNA-34c-5p inhibits amphiregulin-induced ovarian cancer stemness and drug resistance via downregulation of the AREG-EGFR-ERK pathway. Oncogenesis 6:e326. https://doi.org/10.1038/oncsis.2017.25
Zaytseva YY et al (2012) Inhibition of fatty acid synthase attenuates CD44-associated signaling and reduces metastasis in colorectal cancer. Cancer Res 72:1504–1517. https://doi.org/10.1158/0008-5472.CAN-11-4057
Menendez JA, Lupu R (2007) Fatty acid synthase and the lipogenic phenotype in cancer pathogenesis. Nat Rev Cancer 7:763–777. https://doi.org/10.1038/nrc2222
Furuta E, Okuda H, Kobayashi A, Watabe K (1805) Metabolic genes in cancer: their roles in tumor progression and clinical implications. Biochim Biophys Acta 141–152:2010. https://doi.org/10.1016/j.bbcan.2010.01.005
Jiang L et al (2014) Up-regulated FASN expression promotes transcoelomic metastasis of ovarian cancer cell through epithelial-mesenchymal transition. Int J Mol Sci 15:11539–11554. https://doi.org/10.3390/ijms150711539
Qin G et al (2015) Palbociclib inhibits epithelial-mesenchymal transition and metastasis in breast cancer via c-Jun/COX-2 signaling pathway. Oncotarget 6:41794–41808. https://doi.org/10.18632/oncotarget.5993
Wang YP, Wang QY, Li CH, Li XW (2018) COX-2 inhibition by celecoxib in epithelial ovarian cancer attenuates E-cadherin suppression through reduced Snail nuclear translocation. Chem Biol Interact 292:24–29. https://doi.org/10.1016/j.cbi.2018.06.020
Voth W, Jakob U (2017) Stress-activated chaperones: a first line of defense. Trends Biochem Sci 42:899–913. https://doi.org/10.1016/j.tibs.2017.08.006
Amoroso MR et al (2016) TRAP1 downregulation in human ovarian cancer enhances invasion and epithelial-mesenchymal transition. Cell Death Dis 7:e2522. https://doi.org/10.1038/cddis.2016.400
Na Y et al (2016) Stress chaperone mortalin contributes to epithelial-to-mesenchymal transition and cancer metastasis. Cancer Res 76:2754–2765. https://doi.org/10.1158/0008-5472.can-15-2704
Chen SN et al (2019) MicroRNA in ovarian cancer: biology, pathogenesis, and therapeutic opportunities. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph16091510
Nam EJ et al (2008) MicroRNA expression profiles in serous ovarian carcinoma. Clin Cancer Res 14:2690–2695. https://doi.org/10.1158/1078-0432.CCR-07-1731
Park SM, Gaur AB, Lengyel E, Peter ME (2008) The miR-200 family determines the epithelial phenotype of cancer cells by targeting the E-cadherin repressors ZEB1 and ZEB2. Genes Dev 22:894–907. https://doi.org/10.1101/gad.1640608
Gregory PA et al (2008) The miR-200 family and miR-205 regulate epithelial to mesenchymal transition by targeting ZEB1 and SIP1. Nat Cell Biol 10:593–601. https://doi.org/10.1038/ncb1722
Lee Y et al (2003) The nuclear RNase III Drosha initiates microRNA processing. Nature 425:415–419. https://doi.org/10.1038/nature01957
Lin Y, Xu T, Zhou S, Cui M (2017) MicroRNA-363 inhibits ovarian cancer progression by inhibiting NOB1. Oncotarget 8:101649–101658. https://doi.org/10.18632/oncotarget.21417
Mohamed Z et al (2018) miR-363 confers taxane resistance in ovarian cancer by targeting the Hippo pathway member, LATS2. Oncotarget 9:30053–30065. https://doi.org/10.18632/oncotarget.25698
Zhu X et al (2016) miR-186 regulation of Twist1 and ovarian cancer sensitivity to cisplatin. Oncogene 35:323–332. https://doi.org/10.1038/onc.2015.84
Dong S et al (2019) HOXD-AS1 promotes the epithelial to mesenchymal transition of ovarian cancer cells by regulating miR-186-5p and PIK3R3. J Exp Clin Cancer Res 38:110. https://doi.org/10.1186/s13046-019-1103-5
Liu Y et al (2017) MicroRNA-20a contributes to cisplatin-resistance and migration of OVCAR3 ovarian cancer cell line. Oncol Lett 14:1780–1786. https://doi.org/10.3892/ol.2017.6348
Wang Y, Kim S, Kim IM (2014) Regulation of metastasis by microRNAs in ovarian cancer. Front Oncol 4:143. https://doi.org/10.3389/fonc.2014.00143
Li L et al (2016) MiR-181a upregulation is associated with epithelial-to-mesenchymal transition (EMT) and multidrug resistance (MDR) of ovarian cancer cells. Eur Rev Med Pharmacol Sci 20:2004–2010
Au Yeung CL et al (2016) Exosomal transfer of stroma-derived miR21 confers paclitaxel resistance in ovarian cancer cells through targeting APAF1. Nat Commun 7:11150. https://doi.org/10.1038/ncomms11150
Funding
Department of Biotechnology and ACTREC–TMC.
Author information
Authors and Affiliations
Contributions
All authors have participated in concept design and preparation of the manuscript. PR, PP, MM and SM have contributed in literature mining and data interpretation. PR has also critically analysed the manuscript and all authors have agreed upon the submitted version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors do not have any conflict to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mukherjee, S., Phadte, P., Mehrotra, M. et al. Plasticity in Ovarian Cancer: The Molecular Underpinnings and Phenotypic Heterogeneity. J Indian Inst Sci 100, 537–553 (2020). https://doi.org/10.1007/s41745-020-00174-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41745-020-00174-5