Abstract
Introduction
The progression of mild hyperkalemia and the predictors of progression have not been well characterized. In this study we aimed to characterize the progression of hyperkalemia and identify the risk factors for hyperkalemia progression.
Methods
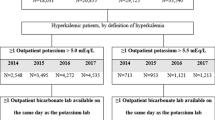
Adults with mild hyperkalemia (at least one serum potassium measure > 5.0 and ≤ 5.5 mEq/L) were identified using electronic medical records from the Research Action for Health Network (2012–2018). Progression to moderate-to-severe and progression to severe hyperkalemia were defined as the first occurrences of a serum potassium measure > 5.5 and > 6.0 mEq/L, respectively. Kaplan–Meier analyses were conducted to estimate progression rates for all patients and by pre-specified patient subgroups. Hazard ratios (HR) of moderate-to-severe and severe hyperkalemia progression were estimated using Cox models.
Results
Of 35,369 patients with mild hyperkalemia, 16.9% and 8.7% progressed to moderate-to-severe and severe hyperkalemia, respectively. Rates of hyperkalemia progression elevated with the severity of chronic kidney disease (CKD). The highest progression rates were seen in patients with CKD stage 5 (stage 5 vs. no CKD: moderate-to-severe, 50.2% vs. 12.0%; severe, 31.3% vs. 3.9%; p < 0.001). Higher progression rates were also observed in patients with heart failure, hypertension, and type II diabetes compared with patients without those conditions (all p < 0.001). The most prominent risk factors were CKD stage 5 (HR of progression to moderate-to-severe hyperkalemia, 3.32 [95% CI 3.03–3.64]; severe, 4.08 [3.55–4.69]), CKD stage 4 (2.19 [1.97–2.43], 2.28 [1.92–2.71]), CKD stage 3 (1.57 [1.46–1.68], 1.65 [1.46–1.87]), type I diabetes (1.37 [1.18–1.61], 1.54 [1.23–1.93]), and serum potassium (1.12 [1.10–1.15], 1.13 [1.10–1.17] per 0.1 mEq/L increase) (all p values < 0.05).
Conclusion
Hyperkalemia progression rates increased significantly with CKD stage and were also higher among patients with higher baseline potassium level, heart failure, hypertension, and diabetes.
Similar content being viewed by others
Why carry out this study? |
The progression of mild hyperkalemia and the predictors of progression have not been well characterized. |
In this study we aimed to characterize the progression of hyperkalemia and identify the risk factors for hyperkalemia progression. |
What was learned from the study? |
Among patients with mild hyperkalemia, 16.9% and 8.7% progressed to moderate-to-severe and severe hyperkalemia within 2 years of follow-up; the highest progression rates were seen in patients with CKD stage 5 (moderate-to-severe, 50.2%; severe, 31.3%). |
The most prominent risk factors for mild hyperkalemia progression were chronic kidney disease (stage 3, stage 4, and stage 5), type I diabetes, and higher serum potassium levels. |
The results suggest an unmet need among patients with mild hyperkalemia especially those who have risk factors for hyperkalemia progression; patients with high risk of progression may benefit from more frequent monitoring and timely and appropriate treatment of hyperkalemia. |
Introduction
Serum potassium is usually maintained at a narrow range from 3.5 to 5.0 mEq/L by various homeostatic mechanisms that simultaneously control intracellular–extracellular potassium redistribution and renal excretion of potassium [1]. Hyperkalemia occurs when defects in potassium homeostasis lead to an increase in serum potassium concentration above the normal threshold (> 5.0 mEq/L) [2, 3]. It is a common electrolyte disturbance with increased incidence among patients with chronic kidney disease (CKD), acute kidney injury (AKI), diabetes mellitus, heart failure, and use of renin angiotensin aldosterone system inhibitors (RAASi) [4,5,6].
Hyperkalemia has been associated with deleterious clinical outcomes (e.g., increased risk of sudden death [7], total mortality [8]) and significantly higher healthcare costs and resource use [2, 9, 10]. The impact of hyperkalemia on patient outcomes increases with severity. Moderate-to-severe cases may lead to serious or fatal complications including muscle weakness, paralysis, cardiac conduction abnormalities, and cardiac arrhythmias [11] whereas mild hyperkalemia is often asymptomatic. Given the considerable clinical impact, a significant economic burden associated with moderate-to-severe hyperkalemia has been reported. In particular, patients hospitalized because of moderate-to-severe hyperkalemia had a significantly higher risk of hyperkalemia-related readmission than those with mild hyperkalemia [10]. Outcomes in patients presenting to the emergency department (ED) also worsen with hyperkalemia severity. The mortality rate during ED visit (mild, 1.1%; moderate, 3.7%; and severe, 10.6%; p < 0.001) and inpatient admission rate within 30 days of discharge from ED (mild, 12.0%; moderate, 19.0%; and severe, 32.5%; p < 0.05) both increase substantially as the patient’s potassium level rises [12]. The substantial burden of moderate or severe hyperkalemia underscores the importance of hyperkalemia management and the prevention of progression.
Although the underlying pathogenesis of hyperkalemia is well documented, there is limited evidence-based guidance for the prevention of hyperkalemia progression [13]. Treatment guidelines focus on severe acute hyperkalemia only [14, 15]. Dietary modifications, use of gastrointestinal cation exchangers (e.g., patiromer, sodium zirconium cyclosilicate [SZC] [16]), diuretics, and avoidance of medication that creates an additive risk of hyperkalemia (e.g., RAASi) are suggested for patients without emergent hyperkalemia; however, explicit strategies regarding monitoring and treatment optimization are not specified [17]. The lack of guidance for chronic hyperkalemia management and progression prevention is in part because the natural history of hyperkalemia and the factors associated with progression after the onset of mild hyperkalemia are not well understood.
To help inform future clinical recommendations on the prevention of hyperkalemia progression and reduce the significant burden associated with hyperkalemia, the present study sought to describe time to progression from mild hyperkalemia to moderate-to-severe or severe hyperkalemia and evaluate the risk factors associated with hyperkalemia progression.
Methods
Data Source
This study was a retrospective cohort study of electronic medical record (EMR) data from the Research Action for Health Network (REACHnet). REACHnet was formed in 2014 with the goal of improving the efficiency and capacity for patient-centric research, as one of nine clinical data research networks participating in the National Patient-Centered Outcomes Research Network (PCORnet). The database contains EMR data from January 2012 to February 2018 for over 5 million patients of all ages, sexes, and racial groups from health systems across Louisiana and Texas. Specifically, this study analyzed EMR data from two health systems in Louisiana, Tulane Medical Center and Ochsner Medical Center, offering robust lab test results along with the standard EMR elements including patient demographics, prescriptions, procedures, and diagnosis.
Compliance with Ethics Guidelines
This study was approved by the New England Independent Review Board on June 25, 2018. Reference NEIRB# 1-5667-1. Permission to access the Research Action for Health Network database was granted by the study collaborator, REACHnet.
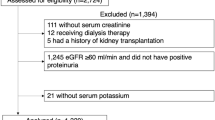
Sample Selection
The study population included adult patients with at least one mild hyperkalemia event (serum potassium lab [K+] > 5.0 and ≤ 5.5 mEq/L). The index date was defined as the date of the first mild hyperkalemia event. Patients were required to have at least 6 months of data prior to the index date (baseline period). The study period spanned from the index date to the earliest of 2 years post-index date, death, last date of patient data, or the end of the data cut in 2018. Patients were excluded if they had a moderate ([K+] > 5.5 and ≤ 6.0 mEq/L) or severe ([K+] > 6.0 mEq/L) hyperkalemia event any time prior to the first mild event. Additionally, patients with insufficient data (i.e., without any outpatient lab data throughout the entire data period or without any encounters after the first mild hyperkalemia event) were excluded.
Statistical Analysis
Patients were categorized on the basis of their most severe progression event into no progression, moderate progression, and severe progression subgroups. Patient characteristics, including demographics, comorbidities, treatments, and serum potassium lab values, of patients with no, moderate (5.5 < [K+] ≤ 6.0 mEq/L), and severe ([K+] > 6.0 mEq/L) hyperkalemia progression were described and compared between subgroups using pairwise chi-squared tests for categorical variables and Wilcoxon rank-sum tests for continuous variables.
Time to moderate-to-severe and time to severe hyperkalemia progression were calculated from the index date to the first moderate-to-severe ([K+] > 5.5 mEq/L) or severe ([K+] > 6.0 mEq/L) hyperkalemia event. Patients without an occurrence of a moderate-to-severe or severe hyperkalemia event after the index date were censored at the end of the study period. Kaplan–Meier analyses were used to estimate the time to progression and the proportions of patients who had an occurrence of a moderate-to-severe or a severe hyperkalemia event at certain time points (e.g., 1, 3, 6, 12, and 24 months after the index date) during the study period. Kaplan–Meier analyses were repeated among patients with CKD, heart failure, hypertension, and type II diabetes to describe comorbidity subgroup-specific rates of hyperkalemia progression.
Multivariable Cox proportional hazards models were implemented to estimate the adjusted hazard ratios (HR) of moderate-to-severe and severe hyperkalemia progression associated with key patient characteristics.
All analyses were performed using SAS 9.4 and R 3.4.2.
Results
Patient Characteristics
Among the 53,667 patients with at least one mild hyperkalemia event in REACHnet, 35,569 were determined to be eligible for this study. Among eligible patients, 3371 progressed to moderate hyperkalemia, 1952 progressed to severe hyperkalemia, and 30,046 did not progress during the 2-year follow-up period. Patients with no hyperkalemia progression, progression to moderate hyperkalemia, and progression to severe hyperkalemia were similar in age and all groups contained a slightly higher proportion of male patients than female patients (Table 1). Racial distribution was significantly different among patients with vs. without hyperkalemia progression. Specifically, a higher proportion of patients who progressed were Black (moderate-severe hyperkalemia, 29.3%; severe hyperkalemia, 43.9%; versus no progression, 24.3%; both p < 0.001).
Mean baseline serum potassium was 5.2 mEq/L in the no progression group and 5.3 mEq/L in both the moderate-to-severe and severe hyperkalemia groups. Patients who experienced progression had a greater prevalence of CKD stage 3 to stage 5 or end-stage renal disease (with and without dialysis), heart failure, type I diabetes, type II diabetes, hypertension, AKI, and higher mean Charlson Comorbidity Index (CCI) compared to those who did not progress. Baseline RAASi use was slightly higher among patients who progressed to moderate-to-severe hyperkalemia, compared to those who did not progress at 2 years post-index date.
Hyperkalemia Progression Rates
Among the overall population, 16.9% of patients progressed from mild to moderate-to-severe hyperkalemia within 2 years post-index date (Supplemental Fig. 1). The proportion of patients who progressed from mild to moderate-to-severe hyperkalemia at 2 years post-index date increased with CKD stage (no CKD, 12.0%; stage 3, 21.7%; stage 4, 32.2%; stage 5 without dialysis, 43.6%; and stage 5 with dialysis, 50.2%). Stage 5 CKD with dialysis was associated with the highest and most rapid progression rate of any subgroup (Table 2 and Fig. 1). Patients with heart failure also had a high risk of hyperkalemia progression with 28.0% of patients having progressed from mild to moderate-to-severe hyperkalemia at 2 years post-index date. Among patients with hypertension and type II diabetes, 20.3% and 23.3% progressed from mild to moderate-to-severe hyperkalemia at 2 years post-index date, respectively (Table 2).
Similar trends, with lower rates, were observed for progression from mild to severe hyperkalemia, where 6.3% of the overall group progressed to severe hyperkalemia during the 2-year study period. Higher progression rates were observed among patients with CKD, heart failure, hypertension, and type II diabetes (Table 2, Supplemental Figs. 2 and 3). Rates of progression to severe hyperkalemia at 2 years post-index date increased with increasing severity of CKD (no CKD, 3.9%; stage 3, 7.5%; stage 4, 12.4%; stage 5 with dialysis, 22.8%; and stage 5 without dialysis, 31.3%; Supplemental Fig. 3). Patients with heart failure also had a high risk of hyperkalemia progression where 1.5%, 3.5%, 5.5%, 8.4%, and 12.0% progressed from mild to severe hyperkalemia at 1, 3, 6, 12, and 24 months, respectively. Among patients with hypertension and type II diabetes, 7.7% and 8.9% progressed from mild to severe hyperkalemia at 2 years post-index date, respectively (Table 2).
Risk Factors for Hyperkalemia Progression
Multivariable Cox models found the most prominent risk factors for progression to moderate-to-severe hyperkalemia were CKD stage 5 (HR = 3.32, p < 0.001), CKD stage 4 (HR = 2.19, p < 0.001), CKD stage 3 (HR = 1.57, p < 0.001), type I diabetes (HR = 1.37, p < 0.001), and serum potassium on the index date (HR = 1.12 per 0.1 mEq/L increase, p < 0.001) (Table 3). These trends held in the analysis of risk of progression from mild to severe hyperkalemia, with a greater risk of progression associated with CKD stage 5 (HR = 4.08, p < 0.001), CKD stage 4 (HR = 2.28, p < 0.001), CKD stage 3 (HR = 1.65, p < 0.001), type I diabetes (HR = 1.54, p < 0.01), and serum potassium on the index date (HR = 1.13 per 0.1 mEq/L increase, p < 0.001, Table 3). Female (vs. male) and White (vs. non-White) showed a reduced risk of progression. A higher CCI and type II diabetes were associated with higher risk of progression. Additionally, AKI was associated with higher risk of progression to moderate-to-severe progression and patients who had their first mild hyperkalemia event at an older age had a reduced risk of progression to severe hyperkalemia.
Discussion
This study described the natural history of and assessed the risk factors for progression from mild to moderate-to-severe or severe hyperkalemia using lab-rich real-world data. The findings of this study indicate that rates of hyperkalemia progression are high among patients with mild hyperkalemia, especially in subgroups with specific comorbidities where increased risk of hyperkalemia has been established. Within the 2-year study period, the progression rates vary across different comorbidity subgroups with the highest rates reaching 50% for moderate-to-severe hyperkalemia and 30% for severe hyperkalemia among patients with CKD stage 5 or end-stage renal disease on dialysis. Furthermore, this study showed that comorbidities associated with hyperkalemia, such as CKD, type I diabetes, type II diabetes, and heart failure, could also be contributing risk factors for progression from mild to more severe hyperkalemia.
CKD at baseline was found to be the key risk factor for hyperkalemia progression which may be attributable to the fact that several biological mechanisms involving CKD are known to increase serum potassium levels. Renal impairment by its nature could cause reduced potassium excretion. Dietary modifications and inadequate management of CKD progression may also increase the risk of hyperkalemia progression. In particular, patients with CKD are typically instructed to consume a low sodium and low potassium diet; however, low sodium foods or products often contain a high amount of potassium (e.g., salt substitutes, low sodium soy sauce, fruits, leafy greens, roots, and tubers) [18, 19]. Furthermore, metabolic acidosis may occur among patients with uncontrolled CKD which drives more potassium into the bloodstream than usual to maintain electroneutrality [20, 21]. We observed that patients with stage 5 CKD and on dialysis have the highest rate of developing moderate-to-severe hyperkalemia and severe hyperkalemia within 2-years of follow-up. It is important to consider that the development of moderate or severe hyperkalemia in this patient group may be affected by factors such as dialysis technique and dialysate composition other than the underlying disease progression. Nevertheless, this data points to the unmet need among patients on dialysis in managing their hyperkalemia. We assessed how baseline CKD stage impacts hyperkalemia disease progression; it will be important for future studies to evaluate how the progression of CKD stage influences hyperkalemia progression.
Higher risk of hyperkalemia progression in patients with heart failure and diabetes (both type I and type II) may be a consequence of inadequate disease control. Uncontrolled diabetes among patients with heart failure may lead to hypertonicity which facilitates the shift of potassium from the intracellular space to the bloodstream [22, 23]. Reduced cardiac output can compromise renal perfusion in patients with heart failure, making them more susceptible to hyperkalemia [24]. Diabetes commonly leads to hyporeninemic hypoaldosteronism which leads to hyperkalemia. Although the underlying mechanisms among these comorbidities and hyperkalemia progression merit future research, the findings of this study are broadly in line with previous evaluations on recurrent hyperkalemia among high-risk patients, highlighting the importance of long-term management for hyperkalemia [25, 26].
Interestingly, no significant differences in hyperkalemia progression rates were seen for patients using RAASi treatments, despite past studies underscoring RAASi use as a key risk factor for the development of hyperkalemia [5]. This result may reflect awareness of the association between RAASi use and hyperkalemia and recommendations in clinical practice guidelines to withhold or down-titrate RAASi therapy once hyperkalemia is diagnosed among patients with CKD [27, 28]. Many patients were likely taken off these treatments after their initial mild hyperkalemia event, mitigating the impact of baseline RAASi use on the risk of progression during the study follow-up period. It is also possible that RAASi use has a lesser role in hyperkalemia progression than hyperkalemia recurrence as this study focused on the progression of mild hyperkalemia to moderate or severe hyperkalemia.
Our study found that 7.9% of the overall mild hyperkalemia population progressed to moderate-to-severe or severe disease within 6 months of follow-up. The high proportion of patients with rapid progression observed in this study may reflect a significant burden posed to society, as clinical outcomes worsen and healthcare resource utilization increases with hyperkalemia severity [2, 9]. For instance, a US study reported a significantly higher mortality rate (24.9% vs. 10.4%) and fivefold higher healthcare costs ($5645 vs. $1035) among Medicare-insured patients with CKD and hyperkalemia compared with those without hyperkalemia [29]. This suggests an unmet need among patients with mild hyperkalemia who have risk factors for hyperkalemia progression who may benefit from more frequent monitoring and timely and appropriate treatment of hyperkalemia. Traditionally physicians have been reducing or discontinuing RAASis when patients develop hyperkalemia, especially moderate to severe hyperkalemia. The new potassium binders (SZC or patiromer) should be part of the therapeutic measures for hyperkalemia management to maximize the benefits from the intended RAASi treatment.
Identifying hyperkalemia on the basis of diagnosis codes has been traditionally challenging because of low sensitivity [30] which underlines the difficulty in evaluating this condition in retrospective databases without lab measures. The REACHnet EMR database contained ample longitudinal lab measures which allowed this study to identify hyperkalemia events over an extended period of follow-up with high sensitivity. Furthermore, this study was able to evaluate hyperkalemia progression and its associated risk factors in a broadly representative sample across the communities of Louisiana, unlike typical EMR database studies which are usually restricted to data from a single center or a smaller geographic region coverage. Results of this study are robust as demonstrated by the consistent findings across a variety of analyses conducted.
Nevertheless, the results of this study should be interpreted in light of its limitations. First, the data source draws only from patients in the Louisiana area, potentially restricting the generalizability of the study findings to regions or nations with distinct differences from Louisiana. Second, patient encounters occurring outside of the healthcare systems were not available through the EMR data, leading to potential underestimations of progression estimates (e.g., outpatient labs done at a facility outside of the healthcare system may not have been captured). However, we excluded patients without any outpatient lab data or without any encounters in the health systems after the first mild hyperkalemia event and this should have mitigated this limitation. Additionally, there may be inconsistency in self-reported variables such as race, limiting the ability to determine the effect of such variables on outcomes. Finally, limitations that are inherent to studies using EMR data sources also apply to this study, including potential data omissions and coding errors. Furthermore, codes used to identify diagnoses and treatments may not perfectly capture this information nor confirm actual treatment administration.
Conclusions
The study found that hyperkalemia progression rates increased significantly with CKD stage and were also higher among patients with higher baseline potassium level, heart failure, hypertension, and diabetes. The totality of evidence across the analyses conducted in this study demonstrates the need for better management of patients with mild hyperkalemia to prevent hyperkalemia progression. In particular, the results suggest that more frequent monitoring and the new potassium binders should be part of the therapeutic measures for hyperkalemia management especially for patients at high risk of hyperkalemia progression, such as those with CKD, heart failure, hypertension, and diabetes.
References
Gumz ML, Rabinowitz L, Wingo CS. An integrated view of potassium homeostasis. N Engl J Med. 2015;373(1):60–72.
Jain N, Kotla S, Little BB, et al. Predictors of hyperkalemia and death in patients with cardiac and renal disease. Am J Cardiol. 2012;109(10):1510–3.
Lehnhardt A, Kemper MJ. Pathogenesis, diagnosis and management of hyperkalemia. Pediatr Nephrol. 2011;26(3):377–84.
Betts KA, Woolley JM, Mu F, McDonald E, Tang W, Wu EQ. The prevalence of hyperkalemia in the United States. Curr Med Res Opin. 2018;34(6):971–8.
Weir MR, Rolfe M. Potassium homeostasis and renin-angiotensin-aldosterone system inhibitors. Clin J Am Soc Nephrol. 2010;5(3):531–48.
Nyirenda MJ, Tang JI, Padfield PL, Seckl JR. Hyperkalaemia. BMJ. 2009;339:b4114.
Faxén J, Xu H, Evans M, Jernberg T, Szummer K, Carrero J-J. Potassium levels and risk of in-hospital arrhythmias and mortality in patients admitted with suspected acute coronary syndrome. Int J Cardiol. 2019;274:52–8.
Brueske B, Sidhu MS, Schulman-Marcus J, Kashani KB, Barsness GW, Jentzer JC. Hyperkalemia is associated with increased mortality among unselected cardiac intensive care unit patients. J Am Heart Assoc. 2019;8(7):e011814.
Betts KA, Woolley JM, Mu F, Xiang C, Tang W, Wu EQ. The cost of hyperkalemia in the United States. Kidney Int Rep. 2018;3(2):385–93.
Davis J, Israni R, Betts K, Mu F, Cook E, Anzalone D, et al. Management of hyperkalemic patients in the inpatient setting by hyperkalemia severity. In: Presented at the 2019 Academy of Managed Care & Specialty Pharmacy Annual Meeting held March 25–28, 2019, San Diego, California.
Montford JR, Linas S. How dangerous is hyperkalemia? J Am Soc Nephrol. 2017;28(11):3155–65.
Davis J, Israni R, Betts K, et al. Management of hyperkalemic patients in the emergency department setting. Boston: National Kidney Foundation; 2019.
Rossignol P, Legrand M, Kosiborod M, et al. Emergency management of severe hyperkalemia: guideline for best practice and opportunities for the future. Pharmacol Res. 2016;113(Pt A):585–91.
Bianchi S, Aucella F, De Nicola L, Genovesi S, Paoletti E, Regolisti G. Management of hyperkalemia in patients with kidney disease: a position paper endorsed by the Italian Society of Nephrology. J Nephrol. 2019;32(4):499–516.
Weir MR. Current and future treatment options for managing hyperkalemia. Kidney Int Suppl. 2016;6(1):29–34.
Sterns RH, Grieff M, Bernstein PL. Treatment of hyperkalemia: something old, something new. Kidney Int. 2016;89(3):546–54.
Mount DB. Treatment and prevention of hyperkalemia in adults. UpToDate. Waltham (MA): Wolters Kluwer; 2013.
Palmer BF, Clegg DJ. Achieving the benefits of a high-potassium, paleolithic diet, without the toxicity. Mayo Clin Proc. 2016;91(4):496–508.
Burnier M. Should we eat more potassium to better control blood pressure in hypertension? Nephrol Dial Transplant. 2018;34(2):184–93.
Kraut JA, Kurtz I. Metabolic acidosis of CKD: diagnosis, clinical characteristics, and treatment. Am J Kidney Dis. 2005;45(6):978–93.
Magner PO, Robinson L, Halperin RM, Zettle R, Halperin ML. The plasma potassium concentration in metabolic acidosis: a re-evaluation. Am J Kidney Dis. 1988;11(3):220–4.
Thomsen RW, Nicolaisen SK, Hasvold P, et al. Elevated potassium levels in patients with congestive heart failure: occurrence, risk factors, and clinical outcomes: a Danish population-based cohort study. J Am Heart Assoc. 2018;7(11):e008912.
DeFronzo RA, Sherwin RS, Felig P, Bia M. Nonuremic diabetic hyperkalemia: possible role of insulin deficiency. Arch Intern Med. 1977;137(7):842–3.
Desai AS. Hyperkalemia in patients with heart failure: incidence, prevalence, and management. Curr Heart Fail Rep. 2009;6(4):272–80.
Yan T, Wang J, Li J, et al. Recurrent hyperkalemia in patients with chronic kidney disease and hepatitis C treated with direct antiviral agents. BMC Infect Dis. 2019;19(1):550.
Ahmed A, Campbell RC. Epidemiology of chronic kidney disease in heart failure. Heart Fail Clin. 2008;4(4):387–99.
National Collaborating Centre for Chronic Conditions (UK). Chronic kidney disease: national clinical guideline for early identification and management in adults in primary and secondary care. London: Royal College of Physicians; 2008.
Levey AS, Lau J, Uhlig K, et al. K/DOQI clinical practice guidelines on hypertension and antihypertensive agents in chronic kidney disease. Am J Kidney Dis. 2004;43(5 Suppl. 1):11–3.
Fitch K, Woolley JM, Engel T, Blumen H. The clinical and economic burden of hyperkalemia on medicare and commercial payers. Am Health Drug Benefits. 2017;10(4):202.
Fleet JL, Shariff SZ, Gandhi S, Weir MA, Jain AK, Garg AX. Validity of the International Classification of Diseases 10th revision code for hyperkalaemia in elderly patients at presentation to an emergency department and at hospital admission. BMJ Open. 2012;2(6):e002011.
Acknowledgements
Funding
Sponsorship for this study and the Rapid Service Fee were provided by AstraZeneca. The study sponsor was involved in the study’s design, interpretation, writing and editing, and the decision to submit this work for publication.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authors’ Contributions
Rubeen Israni, Keith A. Betts, Fan Mu, Jill Davis, Jessie Wang, Deborah Anzalone, Gabriel I. Uwaifo, Harold Szerlip, Vivian Fonseca, and Eric Wu contributed to the study’s design, interpretation, and writing and editing. Jessie Wang, Fan Mu, Keith A. Betts, and Eric Wu conducted formal analyses.
Compliance with Ethics Guidelines
This study was approved by the New England Independent Review Board on June 25, 2018. Reference NEIRB# 1-5667-1. Permission to access the Research Action for Health Network database was granted by the study collaborator, REACHnet.
Medical Writing, Editorial, and Other Assistance
Medical writing assistance in the preparation of this article was provided by Samuel Rochette, an employee of Analysis Group, Inc. at the time this study was conducted. Support for this assistance was funded by AstraZeneca. The authors acknowledge the participation of REACHnet partner health systems, Tulane Medical Center and Ochsner Medical Center, in this project. The research reported in this article was conducted in partnership with Research Action for Health Network (REACHnet), funded by the Patient Centered Outcomes Research Institute® (PCORI Award RI-CRN-2020-008). REACHnet is a partner network in PCORnet®, the National Patient- Centered Clinical Research Network, which was developed with funding from PCORI®. The content of this article is solely the responsibility of the author(s) and does not necessarily represent the views of other organizations participating in, collaborating with, or funding REACHnet or PCORnet®, or of PCORI®.
Disclosures
Jessie Wang, Fan Mu, Keith A. Betts, and Eric Wu are employees of Analysis Group, Inc., which received consultancy fees from AstraZeneca for the conduct of this analysis. Jill Davis, Rubeen Israni, and Deborah Anzalone were employees of AstraZeneca at the time this study was conducted. Vivian Fonseca receives research support through Tulane via grants from Bayer, Boehringer Ingelheim, and Gilead Sciences, Inc.; receives honoraria for consulting and lectures from Takeda, Novo Nordisk, Sanofi-Aventis, Eli Lilly and Company, Abbott, AstraZeneca, Intarcia Therapeutics, Inc., and Asahi Kasei Pharma; has stock options in Microbiome Technologies, Insulin Algorithms, and BRAVO4Health; and has stock in Amgen. Gabriel Uwaifo has no conflicts of interests associated with this work. Harold Szerlip is on the advisory board and speakers bureau for AstraZeneca.
Data Availability
The datasets generated in this study are not publicly available due to partnership with REACHnet.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Israni, R., Betts, K.A., Mu, F. et al. Determinants of Hyperkalemia Progression Among Patients with Mild Hyperkalemia. Adv Ther 38, 5596–5608 (2021). https://doi.org/10.1007/s12325-021-01925-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-021-01925-1