Abstract
Convergent evidence indicates that abnormalities in the innate immune system may be pertinent to the pathogenesis, phenomenology, and possible treatment of several mental disorders. In keeping with this view, the targeting of interleukin-6 with the human monoclonal antibody sirukumab may represent a possible treatment and disease modification approach, for adults with brain-based disorders (e.g., major depressive disorder). A PubMed/Medline database search was performed using the following search terms: sirukumab; anti-IL-6; IL-6; major depressive disorder; inflammation. A systematic review was conducted of both preclinical and clinical trials reporting on the pharmacology of sirukumab or investigating the efficacy of targeting IL-6 signaling. Overall, sirukumab has been reported to be a safe and well-tolerated agent, capable of modulating the immune response in healthy populations as well as in subjects with inflammatory disorders (e.g., rheumatoid arthritis). Sirukumab’s effects on cytokine networks as part of the innate immune system provide a coherent rationale for possible application in neuropsychiatric disorders with possible benefits across several domains of the biobehavioral Research Domain Criteria matrix (e.g., general cognitive processes, positive valence systems). Amongst individuals with complex brain-based disorders (e.g., mood disorders), the dimensions/domains most likely to benefit with sirukumab are negative valence disturbances (e.g., anxiety, depression, rumination), positive valence disturbances (e.g., anhedonia) as well as general cognitive processes. We suggest that sirukumab represents a prototype and possibly a proof-of-concept that agents that engage IL-6 targets have salutary effects in psychiatry.
Similar content being viewed by others
Introduction
Currently available antidepressants primarily target monoaminergic systems via effects on either monoamine reuptake inhibition, receptor modulation, or monoamine oxidase inhibition [1]. Available evidence indicates that antidepressants are highly effective for a subset of individuals with major depressive disorder (MDD) and minimally effective for a larger proportion of affected individuals [2,3,4]. The foregoing therapeutic deficiency in treatment outcomes, as well as the relatively high rates of discontinuation (i.e., 43–61%) due to treatment-emergent adverse events [5], underscores the need for genuinely novel treatments that primarily engage non-monoaminergic molecular targets. In addition to suboptimal symptomatic/functional outcomes with existing antidepressants, there is no compelling evidence that existing therapies are capable of disease modification in MDD.
Several non-mutually exclusive effector systems are implicated in the pathoetiology of MDD including, but not limited to, dysregulation of the innate immune inflammatory system [6,7,8,9,10]. The innate immune inflammatory system provides immediate defense against pathogens introduced to the body (e.g., resulting from injury or infection) and as a repair system for damaged tissue. Notwithstanding the evolutionary benefits of the inflammatory response in the presence of physical threat, its overactivity in response to everyday social stressors is thought to result in depressive symptomology [11]. A detailed review of the role of inflammation in depression, including the neurochemical mechanisms by which the immune system affects mood and behavior, is outlined from an evolutionary perspective elsewhere [12]. Components of the innate immune response include the action of several cytokines, chemokines, cellular adhesion molecules, and acute phase reactants. Of the foregoing categories of inflammatory protein systems, alteration in interleukin-6 (IL-6) levels has been identified as one of the most reproducible abnormalities in MDD [13].
In addition to being an intrinsic abnormality in adults with MDD, for many individuals with MDD, alterations in the immune inflammatory system are a secondary phenomenon to either the behavioral disturbances observed in depression (e.g., sleep disturbance), comorbidity (e.g., obesity), and/or iatrogenic effects (e.g., weight-gain-promoting psychotropic agents) [11]. Notwithstanding the potential confounding effects of other contributing factors, alterations in immune inflammatory systems in adults with MDD are also reported in individuals without comorbidities and who are medication-naïve [14]. Moreover, the observation of alterations in messenger RNA transcripts in unaffected relatives of probands with mood disorders provides further evidence that disturbances in inflammatory system are a trait abnormality in adults with MDD [15].
Interleukin-6
Interleukin-6 is a pleiotropic cytokine synthesized and released in response to inflammatory signaling, with both pro- and anti-inflammatory properties. As a pro-inflammatory cytokine, IL-6 is a potent transcriptional stimulus for the production of acute-phase proteins [e.g., C-reactive protein (CRP)] [16, 17], recruitment of leukocytes, and augmentation of the production of other pro-inflammatory chemokines [18]. IL-6 is also reported to play a role in anti-inflammatory processes, including the activation and enhanced production of anti-inflammatory molecules (e.g., macrophage type 2, IL-1 receptor antagonist) [19, 20].
The production and method of signaling of IL-6 has been reviewed in detail elsewhere [21]. The rationale for targeting IL-6 is further augmented by the established interconnectedness of IL-6, as well as other cytokine systems, in effector systems relevant to the pathoetiology and phenomenology of MDD. For example, it is well established that inflammatory cytokines modulate amino acid synthesis, release, and availability (e.g., glutamate), as well as playing a critical role in cellular respiration in oxidative processes. Moreover, cytokine systems implicated as abnormal in MDD are in interplay with the hypothalamic–pituitary–adrenal (HPA) axis and are significantly modulated by circadian rhythms, as well as gut enterotype. Taken together, the foregoing set of effector systems (e.g., glutamate dysregulation, oxidative stress, glucocorticoid signaling alterations, circadian dysrhythmicity, and gut dysbiosis) are all implicated as pathoetiologically relevant in MDD [22, 23].
Preclinical and clinical evidence also indicates that IL-6 is associated with deficits in cognitive function [23]. Moreover, it has been well established that amongst mixed populations with MDD, cognitive deficits are prevalent, persistent, and are a principal determinant of psychosocial outcome as well as workplace disability [24, 25]. The putative role of IL-6 in mediating cognitive function in adults with mood disorders provides a further rationale for conceptualizing IL-6 as a possible convergent substrate subserving multiple domains of psychopathology in mood disorders.
Furthermore, several lines of evidence highlight the robust correlation between elevated peripheral IL-6 concentrations and symptom severity of MDD [6, 8]. It is additionally reported that pretreatment peripheral IL-6 levels are predictive of suboptimal treatment response to conventional antidepressant therapy [7, 26]. Central [i.e., cerebrospinal fluid (CSF)] IL-6 concentration is also reported to be elevated in clinical populations with MDD, further suggesting that IL-6 may be a relevant proximate mediator of disease processes in MDD [27].
Convergent lines of evidence indicate that both peripheral and central IL-6 levels are also significantly elevated in adults exhibiting self-harm (i.e., suicide attempt) [8, 28]. For example, Lindqvist et al. [8] reported that CSF IL-6 levels were significantly higher in individuals with MDD (mean = 3.76 pg/mL) and in individuals who attempted violent suicide (mean = 5.25 pg/mL) when compared to healthy controls (mean = 0.64 pg/mL). In a separate study, Janelidze et al. [28] reported significantly higher levels of peripheral IL-6 in individuals with MDD with history of suicide attempt when compared to individuals with MDD without history of suicide attempt (p = 0.048) and healthy controls (p = 0.009). The foregoing observations implicate a putatively mediational role of elevated central and peripheral IL-6 concentrations in both affective valence and possibly cognitive function (e.g., impulsivity).
The potent transcriptional effect of IL-6 on CRP, a nonspecific marker of inflammatory activation, has implications for biosignature characterization of MDD insofar as alterations in CRP are a highly replicated abnormality in clinical populations [29]. Moreover, alterations in peripheral CRP levels are associated with treatment response outcomes with some antidepressants [30].
Interventional research indicates that interferon-α (IFN-α) therapy is highly associated with the emergence and/or amplification of depressive symptoms. Risk for treatment-emergent depressive symptoms with cytokine-based therapies has been highly associated with a single nucleotide polymorphism (SNP) at the IL-6 gene [31]. For example, subjects with the GG/GC genotype were reported to have developed greater depressive symptoms compared to those with the CC genotype at the IL-6 gene promotor region, where the G allele is associated with higher transcriptional activity resulting in higher plasma IL-6 compared to the C allele.
In a separate study, peripherally administered IFN-α was reported to activate central nervous system (CNS) inflammatory responses, as indicated by increased CSF IL-6 and IFN-α levels. Results of the foregoing study indicated that the increase in CSF IL-6 levels significantly correlated with a decrease in the concentration of serotonin metabolite 5-hydroxyindoleacetic acid (5-HIAA) [32]. The foregoing collection of convergent findings implicates dysregulation of IL-6 as a critical pathogenetic molecular substrate and possible target in adults with MDD.
Sirukumab is a human monoclonal antibody that targets soluble IL-6 with high affinity and specificity [33]. Sirukumab targets the IL-6 signaling pathway, inhibiting both the pro- and anti-inflammatory effects of the pleiotropic cytokine IL-6. Interventional studies with sirukumab have been conducted across a variety of inflammatory disorders, including cutaneous or systemic lupus erythematosus (CLE/SLE) and rheumatoid arthritis (RA) [33,34,35,36,37,38]. Results from studies with sirukumab in clinical populations with inflammatory disorders provide evidence of beneficial effects on patient-reported outcomes (PROs), including measures of global functioning and quality of life. Herein, we review studies from both preclinical and clinical research that provide an empirical basis for hypothesizing that sirukumab is a possible symptom-mitigating and disease-modifying treatment. The application of sirukumab to MDD is chosen as an exemplar of its brain-based potential application, with recognition that there could be applications transdiagnostically in psychiatry.
Methods
This article is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors. The PubMed/Medline database was searched from inception to September 16, 2016 using combinations of the following search terms: sirukumab; anti-IL-6; IL-6; major depressive disorder; inflammation. Included articles were clinical trials reporting on the pharmacology of sirukumab, as well as preclinical studies investigating the efficacy of targeting IL-6 signaling in murine models of depression. Article reference lists were also reviewed for additional articles aligned with the overarching aim of this paper. Altogether, 11 preclinical and clinical trials were included in this review. Studies included for this review were those that reported specifically on preclinical and clinical models of depression, cognition, and/or evaluated the effects of sirukumab/IL-6 on neurobiological systems relevant to the pathoetiology of depression. We also sought present clinical trials on clinicaltrials.gov by entering the search words “sirukumab, psychiatry, depression, cognition”.
Results
Pharmacokinetics
Interventional clinical studies with sirukumab in healthy subjects as well as clinical populations with CLE, SLE, or RA have reported a biphasic pharmacokinetic profile, specifically a relatively quick distribution phase followed by a relatively slow elimination phase [33, 35]. The slow elimination phase of sirukumab is consistent with its relatively long half-life. In a study evaluating the effects of sirukumab in healthy human subjects, sirukumab was reported to have a median half-life of 18.5–29.6 days following 10–15 min intravenous (IV) infusions of 0.3-10 mg/kg doses [33]. The mean half-life of sirukumab following subcutaneous (SC) administration of sirukumab for healthy subjects is reportedly shorter than the mean half-life following IV administration (i.e., 15–18 vs. 19–30 days, respectively) [36].
The average maximum serum concentration (C max) value has been reported to increase in a dose-dependent manner in healthy subjects (i.e., 7.9–248.8 μg/mL for doses of 0.3–10 mg/kg). Similarly, the area under the serum concentration–time curve (AUC) values (i.e., drug absorption values) were reported to increase in a dose-dependent manner (r 2 = 0.996 and r 2 = 0.973 for AUC and C max, respectively) [33]. The clearance rate of the drug was reported to be independent of dosage in healthy subjects (mean 3.8–6.1 mg day−1 kg−1). Interestingly, all pharmacokinetic parameters (e.g., C max, AUC, clearance) have been consistent across mixed populations, independent of gender and race [33, 36].
Pharmacodynamics
Replicated evidence suggests that sirukumab administration decreases peripheral CRP levels in healthy subjects [33, 34]. In healthy subjects, a decrease of at least 50% from baseline CRP levels was observed for all dosages ranging from 0.3 to 10 mg/kg [33]. Efficacy of sirukumab in CRP reduction was further evidenced in studies of patients with inflammatory disorders. Smolen et al. [34] reported significant decreases in CRP levels with 100-mg biweekly administrations of sirukumab compared to placebo in subjects with RA (−91% vs. −20%, respectively). Suppression of peripheral CRP levels was evident within 2 weeks of sirukumab administration and was sustained for 24 weeks [34].
Szepietowski et al. [35] reported a significant decrease in mean peripheral CRP levels from 1 week following sirukumab treatment and remained suppressed for up to 14 weeks in subjects with CLE or SLE. The suppression of peripheral CRP levels associated with sirukumab treatment persists beyond the elimination half-life of sirukumab in subjects with CLE, SLE, or RA. Peripheral CRP suppression appeared to be dose-independent in all studies [33,34,35].
Preclinical Evidence
Convergent evidence from murine models suggests that inhibition of IL-6 signaling may offer protection against incident depression-like behavior. For example, Chourbaji et al. [37] reported a significant association between IL-6 and depressive behavior. IL-6 knockout (KO) mice were more resilient and less likely to exhibit despair than IL-6 wild-type (WT) mice in stress paradigms (i.e., forced swim, tail suspension, foot shock) [37]. In addition, WT mice exhibited an increase in hippocampal IL-6 expression compared to KO mice. Furthermore, KO mice exhibited enhanced hedonic behavior, as measured by sensitivity to rewards (i.e., sucrose), compared to WT mice.
Similarly, a separate line of evidence reported a significant association between elevated levels of endogenous cortical IL-6 expression and depression-like phenotypes (e.g., immobility time on tail suspension, forced swim tests). Fluoxetine does not mitigate the onset of depression-like symptoms in mice with endogenously elevated levels of IL-6 in the CNS or in mice exogenously administered IL-6 into the CSF [38]. It should be noted, however, that the administration of an anti-IL-6 antibody was able to alleviate depression-like symptoms following CSF IL-6 administration [38].
Moreover, Hodes et al. [39] reported that preexisting individual differences in the peripheral immune system could predict emotional response to social stressors, as illustrated by murine response to repeated social defeat stress (RSDS) paradigms. Results showed that mice susceptible to stress had significantly higher serum IL-6 within 20 min of treatment. IL-6 elevation effects were persistent following subsequent chronic stress (i.e., IL-6 levels remained elevated for over 1 month after exposure). Mice that underwent emotional stress (i.e., witness defeat) also had significantly elevated serum IL-6 levels relative to controls [39]. Emotional response (i.e., resilience versus vulnerability) to social stress was demonstrated to be controlled via alterations of periphery IL-6 levels [39]. IL-6−/− mice and IL-6−/− bone marrow (BM) chimeras exhibited resilience, as measured by levels of social interaction following RSDS. By contrast, BM chimeras from high-IL-6-releasing controls exhibited social avoidance behavior. Hodes et al. [39] also reported that the injection of IL-6 monoclonal antibodies in mice was able to successfully block the development of social avoidance.
Clinical Evidence
Available evidence indicates that conventional monoamine-based antidepressants exert indirect effects on the innate immune system [40]. It is also reported that baseline inflammatory markers/signature may have moderate effects on response outcomes in adults with MDD [41]. Interventional trials evaluating conventional antidepressants are limited by significant heterogeneity in sample composition, types of anti-inflammatory agents employed, dependent measures, and response outcome [42]. The notion that a subset of adults with MDD stratified on the basis of an elevated inflammatory marker may be differentially responsive to anti-inflammatory intervention is supported by results of a recently published study [43]. The post hoc finding by Raison et al. [43] reported that subjects with baseline serum high-sensitivity (hs) CRP levels greater than 5 mg/L were significantly more likely to respond to the tumor necrosis factor (TNF) antagonist infliximab [43], whereas subjects with baseline hs-CRP levels no greater than 5 mg/L were more likely to respond to placebo. The foregoing study result, in need of replication, provides empirical evidence that a specific anti-inflammatory biologic is differentially effective in a subset of adults with MDD stratified by phenomenological and biological characteristics.
Patient-Reported Outcomes
Sirukumab has been demonstrated to rapidly reduce peripheral CRP levels in clinical populations with inflammatory disorders as well as in healthy populations. Results from clinical trials in patient populations with CLE, SLE, or RA suggest that inhibiting IL-6 may improve patient-reported outcomes in individuals with inflammatory disorders. For example, a phase I, randomized, double-blind, placebo-controlled study investigated the efficacy of sirukumab in 36 subjects with CLE or SLE [35]. As a secondary outcome, Szepietowski et al. [35] assessed functional and mental health outcomes using the Short Form 36 (SF-36) Mental Component Summary (MCS), a self-administered assessment of social functioning, vitality, emotional well-being, and emotional role impairment. In subjects with CLE, sirukumab significantly improved median SF-36 MCS scores (+2.0) at week 22, whereas placebo worsened median scores (−4.0). In subjects with SLE, median SF-36 MCS scores improved at week 10 (+3.9 with sirukumab vs. −4.2 with placebo), although improvements were not significant at week 22 (+0.45 with sirukumab vs. +0.7 with placebo) 16 weeks after the last study infusion [35].
A separate line of evidence also reported functional improvements in a patient population with RA in response to sirukumab treatment. In part A of a two-part, phase II, randomized, placebo-controlled study, Smolen et al. [34] reported significant improvements with sirukumab compared to placebo (0.74 vs. 0.17, p < 0.001) (i.e., change from baseline to endpoint) on the Health Assessment Questionnaire Disability Index (HAQ-DI) in 36 subjects with RA. The HAQ-DI is a measure of disability-related functional outcomes that includes measures of mental health (e.g., dressing and grooming). In the larger, dose-finding part B of the foregoing clinical trial, Smolen et al. reported improvements in HAQ-DI with variable doses of sirukumab in 151 subjects with RA, although the differences were not statistically significant when compared to placebo (0.29–0.53 vs. 0.16, respectively; p value not reported). Improvements in quality of life, as evidenced by change in scores on the SF-36, were also detected in both interventional groups (i.e., sirukumab and placebo) for part A (6.4 vs. 3.3, respectively) and B (3.2–7.9 vs. 5.1, respectively) [34]. The foregoing improvements in PROs provide the basis for hypothesizing that sirukumab may mitigate symptoms as part of a neuropsychiatric disorder (e.g., MDD).
Safety/Tolerability
Replicated studies indicate that IV or SC administration of sirukumab at variable doses is safe and well tolerated [33]. The most commonly reported adverse events (AEs) with sirukumab treatment are headache, pharyngolaryngeal pain, nasopharyngitis, and mild upper respiratory tract infections [33]. A greater proportion of placebo-treated healthy subjects experienced one or more AEs compared to sirukumab-treated healthy subjects (72.7% vs. 55.9% for placebo and sirukumab, respectively) [33]. The foregoing reports suggest that AEs experienced by healthy subjects following IV administration of sirukumab are unlikely to be attributed directly to sirukumab. Similarly, 20 of 49 healthy subjects (61%) receiving sirukumab subcutaneously compared to 6 of 13 healthy subjects (46%) receiving placebo reported acute AEs (i.e., within 2 days or less) of mild to moderate intensity (i.e., toxicity grade 1–2) [36]. The safety and tolerability profile of SC sirukumab is similar to that of the IV formulation, with headaches, upper respiratory tract infections, and mild injection site erythema being the most commonly reported treatment-emergent AEs [36].
Sirukumab is also safe and well tolerated in clinical populations of individuals with inflammatory disorders. The incidence of AEs was similar for sirukumab-treated and placebo-treated subjects with RA (67.8–70.6 vs. 63.2–66.7%, respectively) [34] but greater with sirukumab treatment compared to placebo in subjects with CLE (21 of 23 vs. 5 of 8 subjects, respectively) or SLE (9 of 10 vs. 4 of 5 subjects, respectively) [35]. Mild respiratory infections and injection site reactions were most commonly reported in subjects with CLE, SLE, or RA. Severe adverse events (SAE) (e.g., pneumonia, staphylococcal cellulitis, fibrosarcoma) were reported by 8.8% of sirukumab-treated subjects compared to 13.3% of placebo-treated subjects with RA [34]. No opportunistic infections, cases of tuberculosis, or gastrointestinal perforations occurred in subjects with RA in a phase II study [34]. Overall, the safety profile of sirukumab in patients with RA was reported to be similar to that of other IL-6 inhibitor treatments for RA (e.g., tocilizumab, sarilumab, and clazakizumab) [34].
Severe adverse events (e.g., pneumonia, iatrogenic wound infection) were reported in 3 of 23 sirukumab-treated subjects with CLE, 2 of 10 sirukumab-treated subjects with SLE, and 1 of 5 placebo-treated subjects with SLE [35]. None of the aforementioned SAEs were considered by the investigators to be related to the study agent, except for the case of pneumonia [35]. Furthermore, SAEs experienced by sirukumab-treated patients with an inflammatory disorder may be confounded by a compromised immune response.
The presence of antibodies to biologics (e.g., sirukumab) may reduce overall efficacy and/or increase susceptibility to treatment-emergent AEs. Antibodies to sirukumab were not detected in healthy populations following IV or SC administration or in populations with CLE or SLE [33, 35, 36]. In two clinical trials, antibodies to sirukumab were not detected in any of 31 subjects with RA and were identified in only 2 of 142 subjects with RA [34]. To date, only safety results from relatively small phase II studies are available in the public domain. Several phase II and III studies with sirukumab are currently underway and will soon be actively recruiting participants (NCT02531633; NCT02019472; NCT01856309; NCT01606761; NCT01604343).
Conclusion
A cautious interpretation of the foregoing studies is warranted and, at best targeting IL-6 would need to be considered preliminary and promising. At this point in time, targeting IL-6 systems would need to be conceptualized as a promising approach, rather than an established approach. Molecular, cellular, and brain-circuit-based studies indicate that IL-6 as well as other inflammatory effectors are relevant to normal and pathological brain states. The foregoing provides the rationale for hypothesizing that an agent that targets IL-6 (e.g., sirukumab) may have the capability of improving self-reported, as well as objectively rated, psychopathology symptoms and possibly reversing pathological changes observed within and between brain circuits. Notwithstanding, proof-of-concept studies, particularly with target engagement, along with evidence of safety and improvement in behavioral measures are warranted.
Sirukumab represents a possible candidate approach insofar as it has been reported to be a safe and well-tolerated agent that is capable of modulating the immune response in healthy populations and in subjects with inflammatory disorders principally by inhibiting the IL-6 signaling pathway. Sirukumab’s tolerability profile is similar to the reported tolerability of other safe and well-tolerated inflammatory agents that are also efficacious in targeting IL-6 pathways (e.g., tocilizumab). Furthermore, sirukumab has consistently been reported to exhibit linear PK characteristics with a fast distribution phase and a slow elimination phase. In addition, sirukumab has been reported to have a relatively long half-life of approximately 18–30 days with IV infusion or approximately 15–18 days with SC injection.
Convergent evidence implicates a disruption of the inflammatory system in the pathogenesis and/or phenomenology in a subpopulation of adults with MDD. Furthermore, elevated levels of pro-inflammatory cytokines (e.g., IL-6) and acute-phase reactants (e.g., CRP) are associated with depressive symptoms in preclinical models as well as clinical populations of patients with MDD. Sirukumab’s ability to improve PROs that proxy positive mental health and well-being in adults with inflammatory disorders provides the basis for hypothesizing that they may be capable of mitigating symptoms and disease-modify illness activity amongst adults with a diagnosable brain disorder.
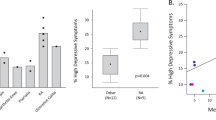
The National Institute of Mental Health has proposed the biobehavioral matrix RDoC (Research Domain Criteria). The overarching aim of RDoC is to identify neurobiological substrates that subserve convergent domains of psychopathology across psychiatry. The RDoC has proposed five discrete domains, all of which have subdomain “units of analysis”. Within the RDoC matrix, positive valence system disturbances are referred to as alterations in reward, response, learning, and valuation. Negative valence disturbances refer to threat (e.g., acute, sustained, anticipated). A separate domain for general cognition processes, as well as attachment/affiliation and arousal/circadian disturbances, are operationalized. Results from both preclinical and clinical evidence indicate that alterations in the innate immune inflammatory system may be relevant at molecular, cellular, and brain circuit levels across each of the foregoing domains, operationalized by the RDoC. Extant literature indicates that disturbances in the innate immune system result in psychomotor retardation, alterations in reward, as well as increase in anxiety, arousal, and alarm systems activity. A derivative of this is that a treatment strategy targeting innate immune inflammatory systems (e.g., sirukumab) may intentionally have domain-specific efficacy that is transdiagnostic (e.g., anhedonia). We would propose that the investigation of sirukumab would be well suited to the RDoC taxonomy with particular interest in positive/negative valence systems, general cognition, as well as arousal/circadian rhythm disturbances (Fig. 1).
The foregoing hypothesis is being empirically tested in an ongoing randomized, placebo-controlled, double-blind phase II study that aims to test the efficacy and safety of sirukumab as an adjunctive treatment to monoaminergic antidepressant therapy in adults with MDD (NCT02473289). In addition to mitigating conventional depression outcome measures (e.g., reduction in overall depression symptom severity), the totality of evidence would suggest that an inflammatory-based approach may be particularly effective for the dimension/domain of general cognitive disturbances, as well as positive and negative emotional valence abnormalities [23].
A strategic approach that would need to be kept in mind when evaluating sirukumab is replicated evidence indicating that subpopulations of individuals with MDD may be more likely to benefit from an intervention that targets, directly or indirectly, the inflammatory system. For example, evidence indicates that individuals with higher baseline levels of inflammatory markers would be preferentially responsive to infliximab, omega-3 fatty acids, exercise, and ketamine. We would propose that the study of sirukumab in adults with MDD should stratify patients on the basis of elevated inflammatory markers or signature, e.g., CRP. Moreover, sirukumab is an expensive biologic, notwithstanding the availability of an increasing number of “biosimilars”. We do not envisage in the short term that biologics will be a feasible treatment option for most individuals with depression. At this point, a cost-effectiveness model may support the use of such an approach in more tertiary treatment refractory patients; we believe that the review herein provides a rationale for the discovery and/or repurposing of less expensive and scalable treatments that target IL-6.
References
McIntyre RS. A vision for drug discovery and development: novel targets and multilateral partnerships. Adv Ther. 2014;31(3):245–6.
Entsuah AR, Huang H, Thase ME. Response and remission rates in different subpopulations with major depressive disorder administered venlafaxine, selective serotonin reuptake inhibitors, or placebo. J Clin Psychiatry. 2001;62(11):869–77.
Casacalenda N, Perry JC, Looper K. Remission in major depressive disorder: a comparison of pharmacotherapy, psychotherapy, and control conditions. Am J Psychiatry. 2002;159(8):1354–60.
Hardeveld F, Spijker J, De Graaf R, Nolen WA, Beekman AT. Prevalence and predictors of recurrence of major depressive disorder in the adult population. Acta Psychiatr Scand. 2010;122(3):184–91.
Crawford AA, Lewis S, Nutt D, et al. Adverse effects from antidepressant treatment: randomised controlled trial of 601 depressed individuals. Psychopharmacology. 2014;231(15):2921–31.
Bob P, Raboch J, Maes M, et al. Depression, traumatic stress and interleukin-6. J Affect Disord. 2010;120(1–3):231–4.
Eller T, Vasar V, Shlik J, Maron E. Pro-inflammatory cytokines and treatment response to escitalopram in major depressive disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32(2):445–50.
Lindqvist D, Janelidze S, Hagell P, et al. Interleukin-6 is elevated in the cerebrospinal fluid of suicide attempters and related to symptom severity. Biol Psychiatry. 2009;66(3):287–92.
Maes M, Vandoolaeghe E, Ranjan R, Bosmans E, Bergmans R, Desnyder R. Increased serum interleukin-1-receptor-antagonist concentrations in major depression. J Affect Disord. 1995;36(1–2):29–36.
Zeidan F, Martucci KT, Kraft RA, McHaffie JG, Coghill RC. Neural correlates of mindfulness meditation-related anxiety relief. Soc Cogn Affect Neurosci. 2014;9(6):751–9.
Slavich GM, Irwin MR. From stress to inflammation and major depressive disorder: a social signal transduction theory of depression. Psychol Bull. 2014;140(3):774–815.
Raison CL, Miller AH. Malaise, melancholia and madness: the evolutionary legacy of an inflammatory bias. Brain Behav Immun. 2013;31:1–8.
Dowlati Y, Herrmann N, Swardfager W, et al. A meta-analysis of cytokines in major depression. Biol Psychiatry. 2010;67(5):446–57.
Stelzhammer V, Haenisch F, Chan MK, et al. Proteomic changes in serum of first onset, antidepressant drug-naïve major depression patients. Int J Neuropsychopharmacol. 2014;17(10):1599–608.
Barnett JH, Smoller JW. The genetics of bipolar disorder. Neuroscience. 2009;164(1):331–43.
Naugler WE, Karin M. The wolf in sheep’s clothing: the role of interleukin-6 in immunity, inflammation and cancer. Trends Mol Med. 2008;14(3):109–19.
Gabay C, Kushner I. Acute-phase proteins and other systemic responses to inflammation. N Engl J Med. 1999;340(6):448–54.
Kishimoto T. Interleukin-6: discovery of a pleiotropic cytokine. Arthritis Res Ther. 2006;8(Suppl 2):S2.
Gabay C, Smith MF, Eidlen D, Arend WP. Interleukin 1 receptor antagonist (IL-1Ra) is an acute-phase protein. J Clin Invest. 1997;99(12):2930–40.
Tilg H, Trehu E, Atkins MB, Dinarello CA, Mier JW. Interleukin-6 (IL-6) as an anti-inflammatory cytokine: induction of circulating IL-1 receptor antagonist and soluble tumor necrosis factor receptor p55. Blood. 1994;83(1):113–8.
Fonseka TM, McIntyre RS, Soczynska JK, Kennedy SH. Novel investigational drugs targeting IL-6 signaling for the treatment of depression. Expert Opin Investig Drugs. 2015;24(4):459–75.
Haroon E, Miller AH. Inflammation effects on brain glutamate in depression: mechanistic considerations and treatment implications. Curr Top Behav Neurosci. 2016. doi:10.1007/7854_2016_40
Rosenblat JD, Brietzke E, Mansur RB, Maruschak NA, Lee Y, McIntyre RS. Inflammation as a neurobiological substrate of cognitive impairment in bipolar disorder: evidence, pathophysiology and treatment implications. J Affect Disord. 2015;188:149–59.
McIntyre RS, Xiao HX, Syeda K, et al. The prevalence, measurement, and treatment of the cognitive dimension/domain in major depressive disorder. CNS Drugs. 2015;29(7):577–89.
McIntyre RS, Soczynska JZ, Woldeyohannes HO, et al. The impact of cognitive impairment on perceived workforce performance: results from the International Mood Disorders Collaborative Project. Compr Psychiatry. 2015;56:279–82.
Lanquillon S, Krieg JC, Bening-Abu-Shach U, Vedder H. Cytokine production and treatment response in major depressive disorder. Neuropsychopharmacology. 2000;22(4):370–9.
Sasayama D, Hattori K, Wakabayashi C, et al. Increased cerebrospinal fluid interleukin-6 levels in patients with schizophrenia and those with major depressive disorder. J Psychiatr Res. 2013;47(3):401–6.
Janelidze S, Mattei D, Westrin Å, Träskman-Bendz L, Brundin L. Cytokine levels in the blood may distinguish suicide attempters from depressed patients. Brain Behav Immun. 2011;25(2):335–9.
Valkanova V, Ebmeier KP, Allan CL. CRP, IL-6 and depression: a systematic review and meta-analysis of longitudinal studies. J Affect Disord. 2013;150(3):736–44.
Rethorst CD, Bernstein I, Trivedi MH. Inflammation, obesity, and metabolic syndrome in depression: analysis of the 2009-2010 National Health and Nutrition Examination Survey (NHANES). J Clin Psychiatry. 2014;75(12):e1428–32.
Bull SJ, Huezo-Diaz P, Binder EB, et al. Functional polymorphisms in the interleukin-6 and serotonin transporter genes, and depression and fatigue induced by interferon-alpha and ribavirin treatment. Mol Psychiatry. 2009;14(12):1095–104.
Raison CL, Borisov AS, Majer M, et al. Activation of central nervous system inflammatory pathways by interferon-alpha: relationship to monoamines and depression. Biol Psychiatry. 2009;65(4):296–303.
Xu Z, Bouman-Thio E, Comisar C, et al. Pharmacokinetics, pharmacodynamics and safety of a human anti-IL-6 monoclonal antibody (sirukumab) in healthy subjects in a first-in-human study. Br J Clin Pharmacol. 2011;72(2):270–81.
Smolen JS, Weinblatt ME, Sheng S, Zhuang Y, Hsu B. Sirukumab, a human anti-interleukin-6 monoclonal antibody: a randomised, 2-part (proof-of-concept and dose-finding), phase II study in patients with active rheumatoid arthritis despite methotrexate therapy. Ann Rheum Dis. 2014;73(9):1616–25.
Szepietowski JC, Nilganuwong S, Wozniacka A, et al. Phase I, randomized, double-blind, placebo-controlled, multiple intravenous, dose-ascending study of sirukumab in cutaneous or systemic lupus erythematosus. Arthritis Rheum. 2013;65(10):2661–71.
Zhuang Y, Xu Z, de Vries DE, et al. Pharmacokinetics and safety of sirukumab following a single subcutaneous administration to healthy Japanese and Caucasian subjects. Int J Clin Pharmacol Ther. 2013;51(3):187–99.
Chourbaji S, Urani A, Inta I, et al. IL-6 knockout mice exhibit resistance to stress-induced development of depression-like behaviors. Neurobiol Dis. 2006;23(3):587–94.
Sukoff Rizzo SJ, Neal SJ, Hughes ZA, et al. Evidence for sustained elevation of IL-6 in the CNS as a key contributor of depressive-like phenotypes. Transl Psychiatry. 2012;2:e199.
Hodes GE, Pfau ML, Leboeuf M, et al. Individual differences in the peripheral immune system promote resilience versus susceptibility to social stress. Proc Natl Acad Sci USA. 2014;111(45):16136–41.
Maes M, Anderson G, Kubera M, Berk M. Targeting classical IL-6 signalling or IL-6 trans-signalling in depression? Expert Opin Ther Targets. 2014;18(5):495–512.
Uher R, Tansey KE, Dew T, et al. An inflammatory biomarker as a differential predictor of outcome of depression treatment with escitalopram and nortriptyline. Am J Psychiatry. 2014;171(12):1278–86.
Huhn M, Tardy M, Spineli LM, et al. Efficacy of pharmacotherapy and psychotherapy for adult psychiatric disorders: a systematic overview of meta-analyses. JAMA Psychiatry. 2014;71(6):706–15.
Raison CL, Rutherford RE, Woolwine BJ, et al. A randomized controlled trial of the tumor necrosis factor antagonist infliximab for treatment-resistant depression: the role of baseline inflammatory biomarkers. JAMA Psychiatry. 2013;70(1):31–41.
Acknowledgements
No funding or sponsorship was received for this study or publication of this article. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published.
Disclosures
Aileen J. Zhou, Yena Lee, and Trehani M. Foneska have no conflicts of interest to declare. Giacomo Salvadore receives salary from Janssen Research & Development. Benjamin Hsu receives salary from Janssen Research & Development. Sidney H. Kennedy has the following disclosures: Ontario Brain Institute, researcher, grant; CIHR, researcher, grant; Lundbeck, speaker/advisor/consultant, honorarium/grant; St. Judes Medical, researcher, grant; Bristol-Myers Squibb, speaker/advisor/consultant/researcher, honorarium; Clera, Inc., researcher, grant; Eli Lilly, honorarium; Lundbeck Institute, speaker/advisor/consultant, honorarium; Pfizer, speaker/advisor/consultant, honorarium; Servier, speaker/advisor/consultant, honorarium/grant; Forest, advisor/consultant, honorarium; Janssen, advisor/consultant, honorarium; Naurex, Inc., advisor/consultant, honorarium; AstraZeneca, advisor/consultant, honorarium. Within the last 2 years (i.e., 2014–2016), Roger S. McIntyre has received research grant support from Lundbeck, JanssenOrtho, Shire, Purdue, AstraZeneca, Pfizer, Otsuka, Allergan, Stanley Medical Research Institute (SMRI); speaker/consultation fees from Lundbeck, Pfizer, AstraZeneca, Elli-Lilly, JanssenOrtho, Purdue, Johnson & Johnson, Moksha8, Sunovion, Mitsubishi, Takeda, Forest, Otsuka, Bristol-Myers Squibb, and Shire.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced content
To view enhanced content for this article go to http://www.medengine.com/Redeem/B037F0607DF8812D.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Zhou, A.J., Lee, Y., Salvadore, G. et al. Sirukumab: A Potential Treatment for Mood Disorders?. Adv Ther 34, 78–90 (2017). https://doi.org/10.1007/s12325-016-0455-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-016-0455-x