Abstract
Objectives
To determine the variables affecting serum 17 hydroxyprogesterone (17OHP) in neonates born at a tertiary hospital in Mumbai, India.
Methods
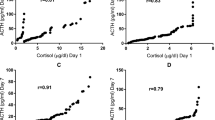
Serum 17OHP was measured in peripheral venous blood between 3rd to 5th day of life by competitive radioimmunoassay and on follow up at 3 mo of age. Serum 17OHP was compared among four groups [full term healthy(FT), full term stressed(FS), preterm healthy(PT), preterm stressed(PS)] by non-parametric tests (Kruskal Wallis (KW) test and Mann- Whitney (MW) test). Pearson’s test was used to correlate natural log of serum 17OHP (ln17OHP) with variables like gestational age, birth weight, stress factor, sex, antenatal administration of glucocorticoids to mothers, Apgar score at 5 min and mode of delivery. Linear regression analysis was done using significant variables in Pearson’s test to determine best predictors of ln17OHP.
Results
The initial median (number of cases, inter-quartile range) serum 17OHP (ng/ml) for the four groups was as follows; FT 8.4 (33, 6–13); PT 20 (36, 11–29.5); FS 34 (29, 26–45) and PS 58 (24, 40.75–76.5) [total N = 122 newborns, p = 0.001]. Pearson’s test showed that gestational age, birth weight, stress factor, Apgar score were negatively correlated with 17OHP whereas stress factor, mode of delivery, use of antenatal steroids in mothers were significantly positively correlated. However, stress factor emerged as the most important significant positive predictor (multiple R = 0.643, P = <0.0001). On follow up at 3 mo age, the median 17OHP (N = 73 newborns) had significantly decreased to normal level.
Conclusion
Stress due to neonatal illnesses like meconium aspiration, sepsis, birth asphyxia, etc. significantly elevate serum 17OHP and may lead to false positives in newborn screening for congenital adrenal hyperplasia.
Similar content being viewed by others
References
New MI, Ghizzoni L. Congenital adrenal hyperplasia. In: Lifshitz F, editor. Pediatric Endocrinology. 4th ed. New York: Marcel Dekker; 2003. pp. 175–92.
Pang S. Congenital adrenal hyperplasia. Endocr Metab Clin N Am. 1997;26:853–91.
White PC, Speiser PW. Congenital adrenal hyperplasia due to 21 hydroxylase deficiency. Endocr Rev. 2000;25:245–91.
Huynh T, McGown I, Cowley D, et al. The clinical and biochemical spectrum of congenital adrenal hyperplasia secondary to 21 hydroxylase deficiency. Clin Biochem Rev. 2009;30:75–86.
Linder N, Davidovitch N, Kogan A, et al. Longitudinal measurements of 17 hydroxyprogesterone in premature infants during first three months of life. Arch Dis Child Fetal Neonatal Ed. 1999;81:F175–8.
Devi RR, Naushad SM. Newborn screening in India. Indian J Pediatr. 2004;71:157–60.
Olgemoller B, Roscher AA, Liebl B, Fingerhut R. Screening for congenital adrenal hyperplasia: adjustment of 17-hydroxyprogesterone cut-off values to both age and birth weight markedly improves the pediatric value. J Clin Endocrinol Metab. 2003;88:5790–4.
Al-Nuaim AR, Abdullah MA, Stevens B, Zain M. Effect of gender, birth weight and gestational age on serum 17 hydroxy progesterone concentration and distribution among neonates in Saudi Arabia. Indian J Pediatr. 1995;62:605–9.
Siiteri PK, MacDonald PC. Placental estrogen biosynthesis during human pregnancy. J Clin Endocrinol Metab. 1966;26:751–61.
Nomura S. Immature adrenal steroidogenesis in preterm infants. Early Hum Dev. 1997;49:225–33.
Mesiano S, Jaffe RB. Developmental and functional biology of the primate fetal adrenal cortex. Endocr Rev. 1997;18:378–403.
Technical report: congenital adrenal hyperplasia. Section on Endocrinology and Committee on Genetics. Pediatrics. 2000;106:1511–8.
Gatelais F, Berthelot J, Beringue F, et al. Effect of single and multiple courses of prenatal corticosteroids on 17OHP levels: Implication for neonatal screening of congenital adrenal hyperplasia. Pediatr Res. 2004;56:701–5.
Murphy JF, Joyce BG, Dyas J, Hughes IA. Plasma 17OHP concentrations in ill newborn infants. Arch Dis Child. 1983;58:532–4.
Conflict of Interest
None.
Role of Funding Source
Funded by Sir Hurkisondas Nurrotumdas Medical Research Society
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chennuri, V.S., Mithbawkar, S.M., Mokal, R.A. et al. Serum 17 Alpha Hydroxyprogesterone in Normal Full Term and Preterm vs Sick Preterm and Full Term Newborns in a Tertiary Hospital. Indian J Pediatr 80, 21–25 (2013). https://doi.org/10.1007/s12098-012-0856-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-012-0856-z