Abstract
Anaplastic thyroid carcinoma (ATC) exhibits an exceedingly poor prognosis, and the current treatment options are, for most cases, palliative by nature. Few reports of long-time survivors exist, although in these patients, tumors often were limited to the thyroid and/or regional lymph nodes. We describe a 64-year-old male who developed a rapidly growing mass in the left thyroid lobe. A fine-needle aspiration biopsy (FNAB) was consistent with ATC, and the patient underwent preoperative combined chemo- and radiotherapy followed by a hemithyroidectomy. The ensuing histopathological investigation was consistent with ATC adjoined by an oxyphilic well-differentiated lesion, likely a Hürthle cell carcinoma. Tumor margins were negative, and no extrathyroidal extension was noted. Focused next-generation sequencing analysis of the primary tumor tissue identified a TP53 gene mutation but could not identify any potential druggable targets. Additional Sanger sequencing detected a C228T TERT promoter mutation. The tumor was found to be microsatellite stable and displayed PDL1 expression in 80% of tumor cells. Following a CT scan 1 month postoperatively, metastatic deposits were suspected in the lung as well as in the left adrenal gland, of which FNAB verified the latter. Remarkably, upon radiological follow-up, the disease had gone into apparent complete remission. The patient is alive and well with no signs of residual disease after 12 months of follow-up. We here summarize the clinical, histological, and molecular data of this highly interesting patient case and review the literature for possible common denominators with other patients with disseminated ATC.
Similar content being viewed by others
Introduction
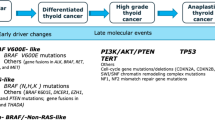
Anaplastic thyroid carcinoma (ATC) is one of the worst human malignancies in terms of patient survival. Although subsets of patients with localized disease live 5 years following diagnosis, the number of surviving patients with regional spread is even fewer, and less than 3% of cases survive over 5 years if distant metastases are detected [1, 2]. ATC shows a female preponderance, and mostly occur in the elderly (60–70 years) [3, 4]. Treatment options include debulking surgery, either directly or following preoperative chemotherapy and external beam radiation therapy (XBRT). In the case of disseminated disease, systemic treatment with different classes of chemotherapy can be considered. The genetic landscape of ATC has been characterized through both exome- and genome-wide analyses [5,6,7]. Although current concepts suggest that subsets of ATCs can arise de novo, the evidence is now mounting that most ATCs derive from pre-existing papillary thyroid carcinoma (PTC) or follicular thyroid carcinoma (FTC), as dictated by genetic analyses suggesting a shared clonal ancestry [6]. Common genetic driver alterations in ATCs include point mutations of the BRAF, NRAS, KRAS, and HRAS proto-oncogenes, and TP53 and TERT promoter mutations have been reported for the majority of cases. Subsets of ATCs are hypermutators with an exceedingly high mutational burden and these cases have been associated to mutations of the mismatch repair gene family (MLH1, MLH3, MSH2, MSH5, and MSH6) (MMR) [5,6,7]. Indeed, defective DNA repair mechanisms and genomic instability have been proposed as crucial for the dedifferentiation process in thyroid tumorigenesis [6,7,8].
Materials and Methods
Review of the Routine Cytological and Histopathological Evaluations
The patient was diagnosed by FNAB and histopathological evaluation performed at the Karolinska University Hospital, Stockholm, Sweden. In order to verify the diagnosis, routine cytological preparations of the FNAB from the primary thyroid lesion and the adrenal metastasis were reviewed by an independent cytologist not responsible for the previous diagnosis (MH). Similarly, routine hematoxylin-eosin-stained sections of representative areas of the primary tumor as well as all immunohistochemical stainings were reviewed by two endocrine pathologists (LSH, CCJ), of which one had taken part in the initial histopathological evaluation (CCJ). In this process, additional immunohistochemical as well as auxiliary genetic analyses were ordered as part of the revision process.
Immunohistochemistry
All immunohistochemical analyses were carried out in our accredited pathology laboratory at Karolinska University Hospital, Stockholm, Sweden, using a Ventana Benchmark Ultra system (Ventana Medical Systems, Tucson, AZ, USA). All stainings were scrutinized via light microscopy by two endocrine pathologists (LSH, CCJ).
Focused Next-Generation Sequencing Screening
The Oncomine Solid Tumor Panel (Ion Torrent S5, Hi-Q Chef; Thermo Scientific) was used to investigate 10 ng of tumor DNA extracted from formalin-fixated paraffin-embedded (FFPE) tissue from the primary ATC tissue. The panel interrogates > 1800 cancer-associated mutations within AKT1, ALK, BRAF, CTNNB1, DDR2, EGFR, ERBB2, ERBB4, FBXW7, FGFR1, FGFR2, FGFR3, KRAS, NRAS, MAP2K1, MET, NOTCH1, PIK3CA, PTEN, SMAD4, STK11, and TP53.
Sanger Sequencing
For TERT, bi-directional Sanger sequencing of the promoter region interrogating the two mutational hotspots C228T and C250T was performed using the Genetic Analyzer 3500, Applied Biosystems, CA, USA [9], and a conventional protocol in a clinically accredited setting. The same Sanger methodology was used for exons 4 to 8 of the TP53 gene, to verify the mutation found through NGS.
Microsatellite Instability Analyses
MSI status was analyzed using quantitative real-time PCR (qRT-PCR) and the Idylla MSI Assay (Biocartis, Mechelen, Belgium). This assay interrogates seven monomorphic microsatellites (ACVR2A, BTBD7, DIDO1, MRE11, RYR3, SEC31A, and SULF2) and MSI is suggested when mutations in ≥ 2 microsatellites are found.
Case Description and Results
The patient is a 64-year old male with a medical history including hypertension and metformin-treated type 2 diabetes, who developed a rapid swelling of the left thyroid lobe in December 2018. He had no local symptoms of stridor or swallowing problems. A CT scan at this time point showed a 65 × 62 × 60-mm lesion in the left thyroid lobe without apparent invasion to adjacent organs but causing tracheal dislocation (Fig. 1a, b). Cytological examination of the left thyroid lobe was performed using ultrasound guidance and four FNABs were undertaken, and the cytology report described enlarged and atypical cells with pleomorphic, hyperchromatic nuclei. Mitoses and necrotic debris were observed. Moreover, oxyphilic cells displaying less evident atypia were also detected. Immunocytochemistry was performed, and the atypical cells stained variable positive for pan-cytokeratin (CKMNF 116), and a proportion of the less atypical tumor cells were also PAX8 positive. TTF1 and p40 were both negative. The diagnosis was consistent with ATC (Bethesda VI). The patient was immediately referred to endocrine surgery where he was planned for pre-operative therapy via the oncology department. A pre-operative combination of chemotherapy (three weekly courses of doxorubicin) and XRBT (3 Gray (Gy) × 15) was administered. Some days after the last XRBT, before surgery, the patient presented with dysphasia where a CT of the brain concluded a minor frontal lobe stroke involving Broca’s area, and he was prescribed clopidogrel and atorvastatin. Moreover, the patient developed a Staphylococcus aureus septicemia and was administered intravenous cloxacillin followed by oral flucloxacillin. He was also administered insulin due to fluctuating levels of blood glucose. After this delay, the patient underwent a left-sided hemithyroidectomy, 5 weeks after the initial presentation at the primary care unit.
Radiological investigations pre- and post-surgical removal of the left thyroid lobe. a, b Preoperative computerized tomography (CT) scan of the neck, visualizing an approximately 7 × 6-cm growth in the left thyroid. c, d Six-week postoperative computerized tomography (CT) scan of the neck showing no evidence of residual or relapsed disease
The left thyroid lobe weighed 124 g and measured 80 × 55 × 40 mm. At the macroscopic grossing, the entire thyroid lobe was replaced by a tumor exhibiting a white-yellowish, compact cut surface with central necrosis and hemorrhages. The pathology report described a lesion built-up by central necrosis and surrounding areas of viable oxyphilic cells growing in follicular and trabecular formations, with enlarged nuclei displaying loose chromatin and prominent nucleoli (Fig. 2a). No PTC-associated features were noted. This tumor was labeled as a well-differentiated oxyphilic tumor that could not be further characterized, but believed to represent a Hürthle cell carcinoma of the thyroid, although the capsular structure and tumor circumscription were not entirely defined (a phenomenon which could possibly be explained by the neoadjuvant treatment). Adjoining this tumor component, atypical cells with apparent pleomorphism were growing in compact formations (Fig. 2b) exhibiting bizarre nuclei as well as multinuclear and osteoclast-like cells. Other areas displayed spindle cell features (Fig. 2c, d). A large number of regular and atypical mitoses were observed, and the tumor was intermingled with a large number of lymphocytes. Morphologically, this tumor component was consistent with an ATC. The tumor had negative surgical margins and did not engage the perithyroidal skeletal muscle (pT3a). Three regional lymph nodes were also sampled, all free from metastasis.
Histopathological evaluation of the ATC specimen. All photomicrographs at × 100 magnification if not otherwise stated. a Routine hematoxylin-eosin (H&E) staining of the well-differentiated oxyphilic tumor component was seen with a predominant microfollicular growth pattern. No nuclear features suggesting oxyphilic papillary thyroid carcinoma was evident. b Routine H&E staining of the well-differentiated tumor component (asterisk) admixed with the anaplastic thyroid carcinoma (ATC) component (arrowhead). c Routine H&E staining of the ATC component displaying hallmarks of this tumor type, with marked nuclear pleomorphism and tumor necrosis. d Routine H&E staining of the ATC component at × 400 magnification. e Thyroglobulin immunohistochemistry displaying widespread immunoreactivity in the well-differentiated tumor component (left), followed by weak to negative staining of the adjacent ATC (right). f Broad spectrum cytokeratin (CKMNF 116) immunohistochemistry of the ATC component revealing subsets of cells with positive cytoplasmic staining, × 400 magnification
The most crucial immunohistochemical analyses are summarized in Table 1. In this workup, we pinpointed expression of CKMNF 116, thyroglobulin, TTF1, and PAX8 in the well-differentiated component, while the ATC component was consistently negative for all these markers apart from focal and weak thyroglobulin and CKMNF116 stainings (Fig. 2e, f). Stainings for mutation-specific BRAF (V600E) were negative for both tumor components, as were calcitonin and CD34 (excluding medullary thyroid carcinoma and primary angiosarcoma). The Ki-67 index reached 30% within the ATC component. P53 immunostaining was widely positive, suggesting an underlying TP53 gene mutation within the ATC. Additional markers for malignant melanoma, neuroendocrine tumors, and sarcoma were negative, as were additional pan-cytokeratin markers (OSCAR, AE1/AE3). PDL1 staining displayed a membranous staining pattern in approximately 80% of ATC cells, and PD1 staining was found in a significant subset of tumor-infiltrating lymphocytes, the latter population predominantly consisting of CD3+/CD4+ T helper cells and CD3+/CD8 T killer cells, while CD20+ B cells were in the minority.
NGS analysis of the primary tumor tissue revealed a c. 469G>T (p.V157F) TP53 gene mutation (COSMIC131481), and additional Sanger sequencing of the TERT promoter displayed a C228T mutation (Table 1). MSI testing using the Idylla Assay proved the tumor to be microsatellite stable (MSS).
The patient was discussed at a multidisciplinary conference where radiological follow-up was recommended. Six weeks postoperatively, radiological examinations showed no evidence of relapse on the neck (Fig. 1d, e) but did raise the suspicion of metastatic deposits in the lung as well as a 24 × 17-mm growth in the left adrenal gland (data not shown). Because of the high level of PD-L1 expression, the patient was referred to the Centre of Clinical Cancer studies at Karolinska (CKC) to discuss treatment with a checkpoint inhibitor within the context of a clinical trial. An ultrasound-guided FNAB of the adrenal was performed after exclusion of hormonal activity, and the aspirated material mostly consisted of necrotic material and cellular debris. Focally, viable cells with small, hyperchromatic nuclei as well as larger, atypical cells were noted amidst necrotic debris (Fig. 3c, d). Immunocytochemical investigations showed that subsets of the atypical cells were PAX8 positive. The diagnosis was metastatic ATC. A follow-up CT scan 1 month later showed that the adrenal mass was growing and measured 35 × 30 mm (Fig. 3a, b).
Radiological investigations and cytological verification of the left adrenal metastasis. a, b Computerized tomography (CT) scan of the abdomen 6 weeks postoperatively, visualizing an approximately 3 × 3-cm mass of the left adrenal. c, d Cytological Giemsa stained preparation of the fine needle aspiration biopsy of the left adrenal mass, displaying large pleomorphic cells, often bizarre, with prominent nucleoli against a necrotic background at × 400 magnification. e, f CT scan 5 months postoperatively, showing complete remission of the adrenal mass
At that moment, there were no available slots to include the patient in a clinical trial and he was referred back to the thyroid oncologist to initiate palliative systemic therapy. Several weeks later, a new CT scan was performed, which showed no evidence of disease, and the adrenal mass was no longer evident (Fig. 3e, f). The lung lesions were reviewed again retrospectively and deemed most probably as having an infectious origin. Ensuing CT scans 7 and 12 months postoperatively were consistent with the preceding and indicated no evidence of residual disease.
Today, more than 1 year after surgery, the patient is alive and well, but closely monitored for eventual signs of relapse.
Discussion
We present a patient with disseminated ATC in complete, spontaneous remission. Although subsets of ATCs can be cured, this is one of very few reports describing a total remission in a patient with a distant metastasis, and to the best of our knowledge probably the first description of such a case in which the metastatic deposit was verified by cytology.
In some studies, clinical predictors such as age < 60 years, lack of extrathyroidal extension, and combinations of XBRT followed by surgical removal of the tumor tissue have been associated with lower cause-specific mortality [4]. Our case mirrors most of these parameters, as the patient did receive XBRT followed by complete surgical excision, and the tumor was localized to the thyroid gland without evident extrathyroidal extension. In a previously published series from our institution covering the outcome of 59 patients diagnosed with ATC between 1997 and 2010, only four survivors were detected, of which three (5%) were free of metastatic disease at the end of follow-up [1]. These three patients exhibited either regional lymph node metastases (n = 2) or no signs of extrathyroidal spread (n = 1) at diagnosis. The resection status of the primary tumor tissue also varied for these three patients, with one resection being classified as R0 (negative margins), one as R1 (intralesional), and one as R2 (tumor reduction only).
As our patient exhibited an adrenal metastasis verified by FNAB, we still lack a credible explanation for the subsequent spontaneous remission, as the patient was not administered any postoperative treatment modalities following the preoperative chemotherapy and XBRT. In the clinical setting, metastatic ATC deposits are often dormant and prone to uncontrollable growth following excision of the primary tumor, a phenomenon that has been described previously [10], in clear contrast to our case. However, spontaneous regression of metastatic disease following removal of the primary tumor has been described previously as an observed phenomenon in neuroblastoma, thymoma, malignant melanoma, and renal cell carcinoma to name a few [11,12,13,14]. This observation has been described on single occasions for well-differentiated thyroid cancer [15] and for ATC with regional lymph node metastasis [16], but the mechanism has to our knowledge not been described for ATC with distant metastases. Little is known regarding the underlying processes that link metastases to the mother tumor, but theories regarding elicited immunological response following the primary tumor removal have been proposed. The primary ATC in this report did display widespread PDL1 membranous immunoreactivity within the tumor cell population (80% of tumor cells), and the tumor-infiltrating lymphocytes frequently exhibited PD-L1 expression. Widely speculative, it is still tempting to believe that the removal of the primary tumor burden resulted in a diminished immune cell inhibition, which may have influenced the overall immunological response to the remaining metastatic deposits. Unfortunately, PDL1 immunostaining or other lymphocyte-related immunocytochemical characterizations were not performed on the FNAB verified adrenal metastasis, so we know little about the interaction between the metastatic ATC lesion and the immune system in this case. Interestingly, significant up-regulation of immune-related gene sets in ATCs compared to other thyroid cancer subtypes, including the immune checkpoint markers PDL1, PDL2, and PD1 have been reported [17]. Also, subsets of ATCs harbor gene amplifications of immune evasion genes, further acknowledging the importance of immune regulation in this disease [7]. Indeed, PDL1 immunoreactivity is evident in a subset of ATCs, often displaying strong and widespread expression in approximately 80% of tumor cells—mirroring the findings in our case [18, 19]. The prognostic significance of this expression pattern is, however, not known, and ATC-related studies with PDL1 inhibitors in the clinical setting are scarce [20, 21], although studies with animal models seem promising [22, 23].
Our case displayed established mutations of the TP53 gene and TERT promoter, two genes known to be recurrently mutated in ATCs. Interestingly, no other evident driver mutations in cancer-associated genes were detected using a focused NGS approach, and no MSI was observed. As a large subgroup of ATCs either carry BRAF or RAS mutations, the underlying driving event in this tumor remains obscure, and the lack of MSI as well as retained MMR protein expression would suggest that the tumor was not a hypermutator [5].
Another interesting aspect is the fact that the ATC was adjoined by a seemingly oxyphilic tumor with a microfollicular growth pattern, vaguely suggesting the co-existence of a well-differentiated tumor. No clear-cut PTC associated nuclear changes were noted, although this could potentially be masked by the preoperative treatment regimes. If the ATC indeed was derived from an oxyphilic follicular thyroid carcinoma (Hürthle cell carcinoma), it is worth mentioning that a significant subgroup of these well-differentiated tumors undergoes spontaneous degeneration following FNAB procedures [24, 25]. However, it is highly speculative to suggest that this feature is transferred to the ATC component. One should perhaps not overlook the potential role of the septicemic event, which the patient developed preoperatively during the neoadjuvant treatment period. Indeed, activation of the immune system through bacterial infections has been suggested as models to engage disseminated malignant tumors [26]. Furthermore, another aspect which could mandate consideration is the patient’s metformin treatment, as this drug has been found to act as a negative regulator of the mitochondrial complexes and mammalian target of rapamycin (mTOR) activity, in addition to exhibiting growth-inhibitory properties in thyroid cancer [27, 28]. As mTOR inhibitor treatment of ATCs has shown promising value in both preclinical and clinical settings, the potential influence of metformin to the positive outcome in our patient cannot be fully excluded as a contributing mechanism [29, 30].
To summarize, we present a rare case of a patient who went into complete remission after a FNAC-verified disseminated ATC. Future pan-genomic characterization of a collection of these patients with exceptional clinical course could potentially identify common genetic aberrancies of value to identify ATC cases with the chance of a potentially favorable outcome.
Availability of Data and Materials
All data is available upon request.
References
Segerhammar I, Larsson C, Nilsson I-L, Bäckdahl M, Höög A, Wallin G, Foukakis T, Zedenius J Anaplastic carcinoma of the thyroid gland: treatment and outcome over 13 years at one institution. J Surg Oncol. 2012;106:981–986.
Gilliland FD, Hunt WC, Morris DM, Key CR. Prognostic factors for thyroid carcinoma. A population-based study of 15,698 cases from the Surveillance, Epidemiology and End Results (SEER) program 1973-1991. Cancer. 1997;79:564–573.
Are C, Shaha AR. Anaplastic thyroid carcinoma: biology, pathogenesis, prognostic factors, and treatment approaches. Ann Surg Oncol. 2006;13:453–464.
Kebebew E, Greenspan FS, Clark OH, Woeber KA, McMillan A. Anaplastic thyroid carcinoma. Treatment outcome and prognostic factors. Cancer. 2005;103:1330–1335.
Kunstman JW, Juhlin CC, Goh G, Brown TC, Stenman A, Healy JM, Rubinstein JC, Choi M, Kiss N, Nelson-Williams C, Mane S, Rimm DL, Prasad ML, Höög A, Zedenius J, Larsson C, Korah R, Lifton RP, Carling T Characterization of the mutational landscape of anaplastic thyroid cancer via whole-exome sequencing. Hum Mol Genet. 2015;24:2318–2329.
Paulsson JO, Backman S, Wang N, Stenman A, Crona J, Thutkawkorapin J, et al. Whole-genome sequencing of synchronous thyroid carcinomas identifies aberrant DNA repair in thyroid cancer dedifferentiation. J Pathol. 2020;250:183–194.
Pozdeyev N, Gay LM, Sokol ES, Hartmaier R, Deaver KE, Davis S, French JD, Borre PV, LaBarbera D, Tan AC, Schweppe RE, Fishbein L, Ross JS, Haugen BR, Bowles DW Genetic analysis of 779 advanced differentiated and anaplastic thyroid cancers. Clin Cancer Res. 2018;24:3059–3068.
Shahedian B, Shi Y, Zou M, Farid NR. Thyroid carcinoma is characterized by genomic instability: evidence from p53 mutations. Mol Genet Metab. 2001;72:155–163.
Hysek M, Paulsson JO, Wang N, Jatta K, Lindh C, Fuentes-Martinez N, Shabo I, Zedenius J, Juhlin CC TERT promoter mutational screening as a tool to predict malignant behaviour in follicular thyroid tumours-three examples from the clinical routine. Virchows Arch. 2018;473:639–643.
Ringel MD. Metastatic dormancy and progression in thyroid cancer: targeting cells in the metastatic frontier. Thyroid. 2011;21:487–492.
Hammad AM, Paris GR, van Heuven WAJ, Thompson IM, Fitzsimmons TD. Spontaneous regression of choroidal metastasis from renal cell carcinoma. Am J Ophthalmol. 2003;135:911–913.
Ritchie AW, Layfield LJ, de Kernion JB. Spontaneous regression of liver metastasis from renal carcinoma. J Urol. 1988;140:596–597.
Deweerd JH, Hawthorne NJ, Adson MA. Regression of renal cell hepatic metastasis following removal of primary lesions. J Urol. 1977;117:790–792.
Ricci SB, Cerchiari U. Spontaneous regression of malignant tumors: importance of the immune system and other factors (Review). Oncol Lett. 2010;1:941–945.
Shim J, Rao J, Yu R. Spontaneous regression of metastatic papillary thyroid cancer in a lymph node. Case Rep Endocrinol. 2018;2018:5873897.
Vadász G, Sápi Z, Erdei M, Lövey G, Bodó M. Spontaneously curing anaplastic carcinoma in the lymph node. Pathol Oncol Res POR. 1997;3:139–141.
Giannini R, Moretti S, Ugolini C, Macerola E, Menicali E, Nucci N, Morelli S, Colella R, Mandarano M, Sidoni A, Panfili M, Basolo F, Puxeddu E Immune profiling of thyroid carcinomas suggests the existence of two major phenotypes: an ATC-like and a PDTC-like. J Clin Endocrinol Metab. 2019;104:3557–3575.
Ahn S, Kim TH, Kim SW, Ki CS, Jang HW, Kim JS, Kim JH, Choe JH, Shin JH, Hahn SY, Oh YL, Chung JH Comprehensive screening for PD-L1 expression in thyroid cancer. Endocr Relat Cancer. 2017;24:97–106.
Zwaenepoel K, Jacobs J, De Meulenaere A, Silence K, Smits E, Siozopoulou V, et al. CD70 and PD-L1 in anaplastic thyroid cancer-promising targets for immunotherapy. Histopathology. 2017;71:357–365.
Aghajani MJ, Cooper A, McGuire H, Jeffries T, Saab J, Ismail K, de Souza P, Bray V, Fazekas de St Groth B, Niles N, Roberts TL Pembrolizumab for anaplastic thyroid cancer: a case study. Cancer Immunol Immunother CII. 2019;68:1921–1934.
Iyer PC, Dadu R, Gule-Monroe M, Busaidy NL, Ferrarotto R, Habra MA, et al. Salvage pembrolizumab added to kinase inhibitor therapy for the treatment of anaplastic thyroid carcinoma. J Immunother Cancer. 2018;6:68.
Gunda V, Gigliotti B, Ndishabandi D, Ashry T, McCarthy M, Zhou Z, Amin S, Freeman GJ, Alessandrini A, Parangi S Combinations of BRAF inhibitor and anti-PD-1/PD-L1 antibody improve survival and tumour immunity in an immunocompetent model of orthotopic murine anaplastic thyroid cancer. Br J Cancer. 2018;119:1223–1232.
Gunda V, Gigliotti B, Ashry T, Ndishabandi D, McCarthy M, Zhou Z, et al. Anti-PD-1/PD-L1 therapy augments lenvatinib’s efficacy by favorably altering the immune microenvironment of murine anaplastic thyroid cancer. Int J Cancer. 2019;144:2266–2278.
Bauman A, Strawbridge HT. Spontaneous disappearance of an atypical Hürthle cell adenoma. Am J Clin Pathol. 1983;80:399–402.
Máximo V, Lima J, Prazeres H, Soares P, Sobrinho-Simões M. The biology and the genetics of Hürthle cell tumors of the thyroid. Endocr Relat Cancer. 2016;23:X2.
Wong S, Slavcev RA. Treating cancer with infection: a review on bacterial cancer therapy. Lett Appl Microbiol. 2015;61:107–112.
Thakur S, Daley B, Klubo-Gwiezdzinska J. The role of the antidiabetic drug metformin in the treatment of endocrine tumors. J Mol Endocrinol. 2019.
Chen G, Xu S, Renko K, Derwahl M. Metformin inhibits growth of thyroid carcinoma cells, suppresses self-renewal of derived cancer stem cells, and potentiates the effect of chemotherapeutic agents. J Clin Endocrinol Metab. 2012;97:E510–E520.
Papewalis C, Wuttke M, Schinner S, Willenberg HS, Baran AM, Scherbaum WA, Schott M Role of the novel mTOR inhibitor RAD001 (everolimus) in anaplastic thyroid cancer. Horm Metab Res. 2009;41:752–756.
Wagle N, Grabiner BC, Van Allen EM, Amin-Mansour A, Taylor-Weiner A, Rosenberg M, et al. Response and acquired resistance to everolimus in anaplastic thyroid cancer. N Engl J Med. 2014;371:1426–1433.
Acknowledgments
The authors are indebted to Professor Lambert Skoog for reviewing the cytological preparations from the adrenal mass. The study was financially supported by the Swedish Cancer Society
Funding
Open access funding provided by Karolinska Institutet.
Author information
Authors and Affiliations
Contributions
AS, JZ, and CCJ conceived and designed the study. LSH, KJ, MH, and CCJ provided the clinical details regarding genetics, pathology, and cytology. ILN operated the patient. AS, RB, and JZ provided clinical details regarding radiology and surgery. MZ and RA provided the oncological details. AS, JZ, and CCJ wrote, edited, and reviewed the manuscript. All authors were involved in analyzing the data, writing the paper, and had final approval of the submitted and published versions.
Corresponding author
Ethics declarations
Ethics Approval, Consent to Participate and Consent for Publication
The patient has given full oral and written consent to the preparation of this case report. In addition, it was approved by the local ethics committee.
Conflict of Interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Stenman, A., Hellgren, L.S., Jatta, K. et al. Metastatic Anaplastic Thyroid Carcinoma in Complete Remission: Morphological, Molecular, and Clinical Work-Up of a Rare Case. Endocr Pathol 31, 77–83 (2020). https://doi.org/10.1007/s12022-020-09606-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12022-020-09606-5