Abstract
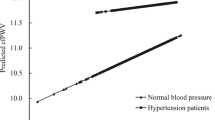
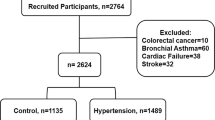
Elevated blood pressure is regarded as an independent risk factor for cardiovascular diseases and diabetes. We examined the relation between hematocrit and pre-hypertension as well as the effect of sex, obesity, fasting glucose, and lipids in Chinese adults. The study samples were from a community-based health examination survey in China and included a total of 2,3691 patients with blood pressure in normal range. The odds ratios [ORs, 95 % confidence interval (CI)] of pre-hypertension across increasing quartiles of hematocrit were 1.000, 1.176 (1.050–1.318), 1.213 (1.081–1.363), and 1.364 (1.209–1.540) (P for trend < 0.001), when adjusted for age, sex, body mass index, glutamic-pyruvic transaminase, glutamic-oxalocetie transaminase, serum uric acid, glucose, and lipids. Associations were significant in both men and women, but not in individuals older than 60 years. In addition, low-density lipoprotein cholesterol significantly interacted with hematocrit (P for interaction <0.024). The associations were more evident in patients with low (P < 0.001) and median LDL-C levels (P < 0.013) than those with high glucose levels. Hematocrit was associated with pre-hypertension, and was independent of metabolic risk factors. These associations were not significant in older individuals and low-density lipoprotein cholesterol may modify these associations.

Similar content being viewed by others
References
Wang, Y., & Wang, Q. J. (2004). The prevalence of pre-hypertension and hypertension among us adults according to the new joint national committee guidelines: New challenges of the old problem. Archives of Internal Medicine, 164, 2126–2134.
Elliott, W. J., & Black, H. R. (2007). Prehypertension. Nature Clinical Practice. Cardiovascular Medicine, 4, 538–548.
Hsia, J., Margolis, K. L., Eaton, C. B., Wenger, N. K., Allison, M., Wu, L., et al. (2007). Prehypertension and cardiovascular disease risk in the women’s health initiative. Circulation, 115, 855–860.
Zhang, Y., Galloway, J. M., Welty, T. K., Wiebers, D. O., Whisnant, J. P., Devereux, R. B., et al. (2008). Incidence and risk factors for stroke in American Indians: the strong heart study. Circulation, 118, 1577–1584.
Sironi, A. M., Pingitore, A., Ghione, S., De Marchi, D., Scattini, B., Positano, V., et al. (2008). Early hypertension is associated with reduced regional cardiac function, insulin resistance, epicardial, and visceral fat. Hypertension, 51, 282–288.
Matsuura, H. (2008). Prehypertension and metabolic syndrome: prevention of hypertension and cardiovascular events. Hypertension Research, 31, 1275–1276.
Onat, A., Yazici, M., Can, G., Kaya, Z., Bulur, S., & Hergenc, G. (2008). Predictive value of prehypertension for metabolic syndrome, diabetes, and coronary heart disease among Turks. American Journal of Hypertension, 21, 890–895.
Zhang, Y., Lee, E. T., Devereux, R. B., Yeh, J., Best, L. G., Fabsitz, R. R., et al. (2006). Prehypertension, diabetes, and cardiovascular disease risk in a population based sample: The strong heart study. Hypertension, 47, 410–414.
Facchini, F. S., Carantoni, M., Jeppesen, J., & Reaven, G. M. (1998). Hematocrit and hemoglobin are independently related to insulin resistance and compensatory hyperinsulinemia in healthy, non-obese men and women. Metabolism, 47, 831–835.
Barbieri, M., Ragno, E., Benvenuti, E., Zito, G. A., Corsi, A., Ferrucci, L., et al. (2001). New aspects of the insulin resistance syndrome: Impact on haematological parameters. Diabetologia, 44, 1232–1237.
Ellinger, V. C., Carlini, L. T., Moreira, R. O., & Meirelles, R. M. (2006). Relation between insulin resistance and hematological parameters in a Brazilian sample. Arquivos Brasileiros de Endocrinologia e Metabologia, 50, 114–117.
Tulloch-Reid, M. K., Hanson, R. L., Saremi, A., Looker, H. C., Williams, D. E., Krakoff, J., et al. (2004). Hematocrit and the incidence of type 2 diabetes in the pima indians. Diabetes Care, 27, 2245–2246.
Shuo, W., Lin, H., Zhang, C., et al. (2013). Association between erythrocyte parameters and metabolic syndrome in urban Han Chinese: A longitudinal cohort study. BMC Public Health, 13, 989–1001.
Melkumyants, A. M., Balashov, S. A., & Khayutin, V. M. (1989). Endothelium dependent control of arterial diameter by blood viscosity. Cardiovascular Research, 23, 741–747.
Vázquez, B. Y. S., Martini, J., Tsai, A. G., et al. (2010). The variability of blood pressure due to small changes of hematocrit. American Journal of Physiology Heart and Circulatory Physiology, 299, H863–H867.
Smiesko, V., & Johnson, P. C. (1993). The arterial lumen is controlled by flow related shear stress. News in Physiological Sciences, 8, 34–38.
Brun, J. F., Bouchahda, C., Chaze, D., et al. (2000). The paradox of hematocrit in exercise physiology: Which is the “normal” range from an hemorheologist’s viewpoint? Clinical Hemorheology and Microcirculation, 22, 287–303.
Lopes, E. P., Sette, L. H., Sette, J. B., et al. (2009). Serum alanine aminotransferase levels, hematocrit rate and body weight correlations before and after hemodialysis session. Clinics (Sao Paulo), 64, 941–945.
Bowers, A. S., Pepple, D. J., & Reid, H. L. (2011). Optimal haematocrit in subjects with normal haemoglobin genotype (HbAA), sickle cell trait (HbAS), and homozygous sickle cell disease (HbSS). Clinical Hemorheology and Microcirculation, 47, 253–260.
Olsson, A. G., Blomback, M., & Ekelund, L. G. (1980). The relation between plasma fibrinogen, blood hematocrit and exercise ST segment depressions in hyperlipoproteinemia. Artery, 7, 215–223.
Loute, G., Pieters, D., Jadot, J. P., Bosly, A., & Moriau, M. (1987). Effect of the variation of hematocrit on the proteinuria of a patient with polycythemia and congenital heart disease. Nephron, 46, 109–111.
Richardson, M. X., de Bruijn, R., & Schagatay, E. (2009). Hypoxia augments apnea-induced increase in hemoglobin concentration and hematocrit. European Journal of Applied Physiology and Occupational Physiology, 105, 63–68.
Crisa, E., Venturino, E., Passera, R., Prina, M., Schinco, P., et al. (2010). A retrospective study on 226 polycythemia vera patients: Impact of median hematocrit value on clinical outcomes and survival improvement with anti-thrombotic prophylaxis and non-alkylating drugs. Annals of Hematology, 89, 691–699.
Li, G., Hui, H., Shi, W., et al. (2012). Elevated hematocrit in nonalcoholic fatty liver disease: A potential cause for the increased risk of cardiovascular disease? Clinical Hemorheology and Microcirculation, 51, 59–68.
Hightower, C. M., Hightower, J. D., Salazar Vázquez, B. Y., & Intaglietta, M. (2009). Seasonal hematocrit variation and health risks in the adult population of Kinshasa, Democratic Republic of Congo. Vascular Health and Risk Management, 5, 1001–1005.
Simmonds, M. J., Meiselman, H. J., & Baskurt, O. K. (2013). Blood rheology and aging. Journal of Geriatric Cardiology, 10, 291–301.
Baskurt, O. K., Yalcin, O., & Meiselman, H. J. (2004). Hemorheology and vascular control mechanisms. Clinical Hemorheology and Microcirculation, 30, 169–178.
Stepp, D. W., Ou, J., Ackerman, A. W., et al. (2002). Native LDL and minimally oxidized LDL differentially regulate superoxide anion in vascular endothelium in situ. American Journal of Physiology Heart and Circulatory Physiology, 283, H750–H759.
Cominacini, L., Rigoni, A., & Pasini, A. F. (2001). The binding of oxidized low density lipoprotein (ox-LDL) to ox-LDL receptor-1 reduces the intracellular concentration of nitric oxide in endothelial cells through an increased production of superoxide. Journal of Biological Chemistry, 276(17), 13750–13755.
Chen, J., Mehta, J. L., & Haider, N. (2004). Role of caspases in Ox-LDL-induced apoptotic cascade in human coronary artery endothelial cells. Circulation Research, 94(3), 370–376.
Acknowledgments
This research was sponsored by Jiangsu Provincial Bureau of Health foundation (H201356) & International Exchange Program and Jiangsu Six Talent Peaks Program (2013-WSN-013). This study was also supported by Xuzhou Outstanding Medical Academic Leader Project and Xuzhou Science and Technology Grant (XM13B066). We thank all subjects for participating in this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Xuekhi Liu, Jun Liang and Qinqin Qiu have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Liu, X., Liang, J., Qiu, Q. et al. Association of Hematocrit and Pre-hypertension Among Chinese Adults: The CRC Study. Cell Biochem Biophys 71, 1123–1128 (2015). https://doi.org/10.1007/s12013-014-0318-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12013-014-0318-5