Abstract
Purpose
Sleep surgery and mandibular advancement devices (MAD) are treatments for obstructive sleep apnea (OSA), but their comparative efficacy remains unclear. We compared their efficacy using various parameters.
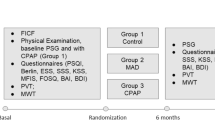
Methods
Subjects treated for OSA with sleep surgery or MAD (n = 30/group)—matched for sex, body mass index (BMI), and baseline apnea–hypopnea index (AHI)—were enrolled. The efficacy of these treatments according to polysomnographic parameters, sleep quality questionnaires, and heart rate variability (HRV) time- and frequency-domain parameters were compared between pre-treatment and 3-month post-treatment.
Results
Polysomnographic and sleep quality questionnaire parameters improved significantly in both groups. In time-domain HRV analysis, average normal-to-normal intervals increased significantly in the surgery (942.2 ± 140.8 to 994.6 ± 143.1, P = 0.008) and MAD (901.1 ± 131.7 to 953.7 ± 123.1, P = 0.002) groups. Low frequency (LF) decreased significantly in the surgery group (P = 0.012); high frequency (HF) remained unchanged in both groups. The LF/HF ratio decreased in both groups (2.9 ± 1.8 to 2.3 ± 1.7, P = 0.017, vs. 3.0 ± 1.8 to 2.4 ± 1.4, P = 0.025). Normalized high frequency increased significantly in both groups (31.0 ± 13.2 to 36.8 ± 13.7, P = 0.009, vs. 29.1 ± 10.7 to 33.7 ± 12.5, P = 0.024), in contrast to normalized low frequency. However, no HRV parameter changes differed significantly between the groups after adjusting for age, BMI, and AHI.
Conclusion
Sleep surgery and MAD are equally effective treatments for OSA according to cardiac autonomic activity.

Similar content being viewed by others
References
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S (1993) The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 328(17):1230–1235. https://doi.org/10.1056/NEJM199304293281704
Bliwise DL, Bliwise NG, Partinen M, Pursley AM, Dement WC (1988) Sleep apnea and mortality in an aged cohort. Am J Public Health 78(5):544–547. https://doi.org/10.2105/ajph.78.5.544
Hung J, Whitford EG, Parsons RW, Hillman DR (1990) Association of sleep apnoea with myocardial infarction in men. Lancet 336(8710):261–264. https://doi.org/10.1016/0140-6736(90)91799-g
Kales A, Bixler EO, Cadieux RJ, Schneck DW, Shaw LC 3rd, Locke TW, Vela-Bueno A, Soldatos CR (1984) Sleep apnoea in a hypertensive population. Lancet 2(8410):1005–1008. https://doi.org/10.1016/s0140-6736(84)91107-3
McNicholas WT, Bonsigore MR, Management Committee of ECAB (2007) Sleep apnoea as an independent risk factor for cardiovascular disease: current evidence, basic mechanisms and research priorities. Eur Respir J 29(1):156–178. https://doi.org/10.1183/09031936.00027406
Holley AB, Lettieri CJ, Shah AA (2011) Efficacy of an adjustable oral appliance and comparison with continuous positive airway pressure for the treatment of obstructive sleep apnea syndrome. Chest 140(6):1511–1516. https://doi.org/10.1378/chest.10-2851
Lam B, Sam K, Mok WY, Cheung MT, Fong DY, Lam JC, Lam DC, Yam LY, Ip MS (2007) Randomised study of three non-surgical treatments in mild to moderate obstructive sleep apnoea. Thorax 62(4):354–359. https://doi.org/10.1136/thx.2006.063644
Huang Y, White DP, Malhotra A (2005) The impact of anatomic manipulations on pharyngeal collapse: results from a computational model of the normal human upper airway. Chest 128(3):1324–1330. https://doi.org/10.1378/chest.128.3.1324
Gotsopoulos H, Kelly JJ, Cistulli PA (2004) Oral appliance therapy reduces blood pressure in obstructive sleep apnea: a randomized, controlled trial. Sleep 27(5):934–941. https://doi.org/10.1093/sleep/27.5.934
Pang KP, Pang EB, Pang KA, Vicini C, Chan YH, Rotenberg BW (2018) Upper airway surgery for obstructive sleep apnea reduces blood pressure. Laryngoscope 128(2):523–527. https://doi.org/10.1002/lary.26759
Reuter H, Herkenrath S, Treml M, Halbach M, Steven D, Frank K, Castrogiovanni A, Kietzmann I, Baldus S, Randerath WJ (2018) Sleep-disordered breathing in patients with cardiovascular diseases cannot be detected by ESS, STOP-BANG, and Berlin questionnaires. Clin Res Cardiol 107(11):1071–1078. https://doi.org/10.1007/s00392-018-1282-7
Heart rate variability: Standards of measurement, physiological interpretation and clinical use. Task force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology (1996). Circulation 93 (5):1043–1065
Somers VK, White DP, Amin R, Abraham WT, Costa F, Culebras A, Daniels S, Floras JS, Hunt CE, Olson LJ, Pickering TG, Russell R, Woo M, Young T, American Heart Association Council for High Blood Pressure Research Professional Education Committee CoCC, American Heart Association Stroke C, American Heart Association Council on Cardiovascular N, American College of Cardiology F (2008) Sleep apnea and cardiovascular disease: an American Heart Association/american college of Cardiology Foundation scientific statement from the American Heart Association Council for high blood pressure research professional education committee, council on clinical cardiology, stroke council, and council on cardiovascular nursing. In collaboration with the National Heart, Lung, and Blood Institute National Center on sleep disorders research (National Institutes of Health). Circulation 118(10):1080–1111. https://doi.org/10.1161/CIRCULATIONAHA.107.189375
Vanninen E, Tuunainen A, Kansanen M, Uusitupa M, Lansimies E (1996) Cardiac sympathovagal balance during sleep apnea episodes. Clin Physiol 16(3):209–216. https://doi.org/10.1111/j.1475-097x.1996.tb00569.x
Choi JH, Yi JS, Lee SH, Kim CS, Kim TH, Lee HM, Lee BJ, Lee SH, Chung YS (2012) Effect of upper airway surgery on heart rate variability in patients with obstructive sleep apnoea syndrome. J Sleep Res 21(3):316–321. https://doi.org/10.1111/j.1365-2869.2011.00978.x
Glos M, Penzel T, Schoebel C, Nitzsche GR, Zimmermann S, Rudolph C, Blau A, Baumann G, Jost-Brinkmann PG, Rautengarten S, Meier JC, Peroz I, Fietze I (2016) Comparison of effects of OSA treatment by MAD and by CPAP on cardiac autonomic function during daytime. Sleep Breath 20(2):635–646. https://doi.org/10.1007/s11325-015-1265-0
Sullivan CE, Issa FG, Berthon-Jones M, Eves L (1981) Reversal of obstructive sleep apnoea by continuous positive airway pressure applied through the nares. Lancet 1(8225):862–865. https://doi.org/10.1016/s0140-6736(81)92140-1
S Sharma, H Fox, F Aguilar, U Mukhtar, L Willes, B Bozorgnia, T Bitter, O Oldenburg (2019) Auto positive airway pressure therapy reduces pulmonary pressures in adults admitted for acute heart failure with pulmonary hypertension and obstructive sleep apnea. The ASAP-HF Pilot Trial. Sleep 42 (7). https://doi.org/10.1093/sleep/zsz100
Eastwood PR, Barnes M, MacKay SG, Wheatley JR, Hillman DR, Nguyên XL, Lewis R, Campbell MC, Pételle B, Walsh JH, Jones AC, Palme CE, Bizon A, Meslier N, Bertolus C, Maddison KJ, Laccourreye L, Raux G, Denoncin K, Attali V, Gagnadoux F, Launois SH (2019) Bilateral hypoglossal nerve stimulation for treatment of adult obstructive sleep apnea. Eur Respir J 10. Pii: 1901320. doi: https://doi.org/10.1183/13993003.01320-2019
Süslü AE, Pamuk G, Pamuk AE, Özer S, Jafarov S, Önerci TM (2017) Effects of expansion sphincter Pharyngoplasty on the apnea-hypopnea index and heart rate variability. J Oral Maxillofac Surg 75(12):2650–2657. https://doi.org/10.1016/j.joms.2017.06.005
Dal-Fabbro C, Garbuio S, D'Almeida V, Cintra FD, Tufik S, Bittencourt L (2014) Mandibular advancement device and CPAP upon cardiovascular parameters in OSA. Sleep Breath 18(4):749–759. https://doi.org/10.1007/s11325-014-0937-5
Kufoy E, Palma JA, Lopez J, Alegre M, Urrestarazu E, Artieda J, Iriarte J (2012) Changes in the heart rate variability in patients with obstructive sleep apnea and its response to acute CPAP treatment. PLoS One 7(3):e33769. https://doi.org/10.1371/journal.pone.0033769
Gula LJ, Krahn AD, Skanes A, Ferguson KA, George C, Yee R, Klein GJ (2003) Heart rate variability in obstructive sleep apnea: a prospective study and frequency domain analysis. Ann Noninvasive Electrocardiol 8(2):144–149
Coruzzi P, Gualerzi M, Bernkopf E, Brambilla L, Brambilla V, Broia V, Lombardi C, Parati G (2006) Autonomic cardiac modulation in obstructive sleep apnea: effect of an oral jaw-positioning appliance. Chest 130(5):1362–1368. https://doi.org/10.1378/chest.130.5.1362
Sumi K, Chin K, Takahashi K, Nakamura T, Matsumoto H, Niimi A, Mishima M (2006) Effect of nCPAP therapy on heart rate in patients with obstructive sleep apnoea-hypopnoea. QJM 99(8):545–553. https://doi.org/10.1093/qjmed/hcl074
La Rovere MT, Pinna GD, Hohnloser SH, Marcus FI, Mortara A, Nohara R, Bigger JT Jr, Camm AJ, Schwartz PJ, Tone AIA, Reflexes After Myocardial I (2001) Baroreflex sensitivity and heart rate variability in the identification of patients at risk for life-threatening arrhythmias: implications for clinical trials. Circulation 103(16):2072–2077. https://doi.org/10.1161/01.cir.103.16.2072
Hedner J, Darpo B, Ejnell H, Carlson J, Caidahl K (1995) Reduction in sympathetic activity after long-term CPAP treatment in sleep apnoea: cardiovascular implications. Eur Respir J 8(2):222–229. https://doi.org/10.1183/09031936.95.08020222
Mark AL, Victor RG, Nerhed C, Wallin BG (1985) Microneurographic studies of the mechanisms of sympathetic nerve responses to static exercise in humans. Circ Res 57(3):461–469. https://doi.org/10.1161/01.res.57.3.461
Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV (2004) Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep 27(7):1255–1273. https://doi.org/10.1093/sleep/27.7.1255
Lee WH, Hong SN, Kim HJ, Rhee CS, Lee CH, Yoon IY, Kim JW (2016) A comparison of different success definitions in non-continuous positive airway pressure treatment for obstructive sleep apnea using cardiopulmonary coupling. J Clin Sleep Med 12(1):35–41. https://doi.org/10.5664/jcsm.5388
Lee WH, Wee JH, Lee CH, Kim MS, Rhee CS, Yun PY, Yoon IY, Kim JW (2013) Comparison between mono-bloc and bi-bloc mandibular advancement devices for obstructive sleep apnea. Eur Arch Otorhinolaryngol 270(11):2909–2913. https://doi.org/10.1007/s00405-013-2417-0
Tanyeri H, Polat S, Kirisoglu CE, Serin GM (2012) Long-term efficacy of submucosal uvulopalatopharyngoplasty for obstructive sleep apnea syndrome. Eur Arch Otorhinolaryngol 269(9):2069–2074. https://doi.org/10.1007/s00405-011-1919-x
Brillante R, Cossa G, Liu PY, Laks L (2012) Rapid eye movement and slow-wave sleep rebound after one night of continuous positive airway pressure for obstructive sleep apnoea. Respirology 17(3):547–553. https://doi.org/10.1111/j.1440-1843.2012.02147.x
Koo BB, Wiggins R, Molina C (2012) REM rebound and CPAP compliance. Sleep Med 13(7):864–868. https://doi.org/10.1016/j.sleep.2012.03.019
Manzar MD, BaHammam AS, Hameed UA, Spence DW, Pandi-Perumal SR, Moscovitch A, Streiner DL (2018) Dimensionality of the Pittsburgh sleep quality index: a systematic review. Health Qual Life Outcomes 16(1):89. https://doi.org/10.1186/s12955-018-0915-x
Kendzerska TB, Smith PM, Brignardello-Petersen R, Leung RS, Tomlinson GA (2014) Evaluation of the measurement properties of the Epworth sleepiness scale: a systematic review. Sleep Med Rev 18(4):321–331. https://doi.org/10.1016/j.smrv.2013.08.002
Spiesshoefer J, Aries J, Giannoni A, Emdin M, Fox H, Boentert M, Bitter T, Oldenburg O (2019) APAP therapy does not improve impaired sleep quality and sympatho-vagal balance: a randomized trial in patients with obstructive sleep apnea and systolic heart failure. Sleep Breath 25:273–280. https://doi.org/10.1007/s11818-017-0124-6
Funding
This study was funded by 2019 Kangwon National University Hospital Grant (#2019-02-004), SNUBH grant (#18-2018-013), and the Bio & Medical Technology Development Program of the National Research Foundation (NRF) funded by the Korean government (MSIT) (# NRF-2015M3A9D7066973).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
The need for written informed consent was waived by the institutional review board. For this type of study, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, W.H., Kwon, S.O. & Kim, JW. Effectiveness of sleep surgery versus a mandibular advancement device for obstructive sleep apnea in terms of nocturnal cardiac autonomic activity. Sleep Breath 24, 1695–1703 (2020). https://doi.org/10.1007/s11325-020-02048-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-020-02048-7