Abstract
Purpose
Ineffective use of continuous positive airway pressure (CPAP) therapy can result in inconvenience and additional costs in patients with obstructive sleep apnea (OSA). This study investigated the predictive value of body mass index (BMI) to assess the efficacy of CPAP in patients with OSA.
Methods
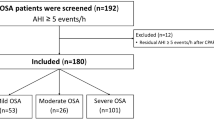
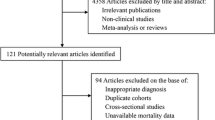
Data were extracted from a retrospective study performed in Silkeborg Hospital. The primary outcome was the improvement of Apnea-Hypopnea Index (AHI) after CPAP treatment. Association between BMI and improvement of AHI was assessed by multivariable linear regression. Interactions between BMI, baseline AHI severity (≥ 30 or < 30), and diabetes were also evaluated.
Results
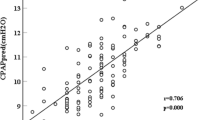
Four hundred eighty-one patients were included in the study. After adjusting for confounders, high BMI (coefficient [coef], 0.80; 95% confidence interval [CI], 0.59–1.00; p < 0.001) and high AHI severity (AHI ≥ 30) (coef, 29.2; 95% CI, 26.7–31.7; p < 0.001) were associated with greater improvement of AHI after CPAP treatment, while diabetes was associated with less improvement of AHI (coef, − 4.91; 95% CI, − 9.40 to − 0.42; p = 0.032). Baseline AHI severity, diabetes, and BMI showed significant interactions (p < 0.001). On subgroup analysis, the association between BMI and improvement of AHI remained significant only in patients belonging to high AHI severity subgroup (coef, 1.18; 95% CI, 0.8–1.49; p < 0.001) and that without diabetes (coef, 1.42; 95% CI, 1.11–1.72; p < 0.001).
Conclusions
Patients with OSA having high BMI, without diabetes, are more likely to benefit from CPAP therapy. Future studies should explore the predictors of the efficacy of CPAP in more depth.

Similar content being viewed by others
References
Keropian B, Murphy N (2014) The prevalence of OSA in snorers presenting with various chief complaints: a pilot study. Cranio 32(3):217–218. https://doi.org/10.1179/0886963414Z.00000000032
Sanchez-de-la-Torre M, Khalyfa A, Sanchez-de-la-Torre A, Martinez-Alonso M, Martinez-Garcia MA, Barcelo A, Lloberes P, Campos-Rodriguez F, Capote F, Diaz-de-Atauri MJ, Somoza M, Gonzalez M, Masa JF, Gozal D, Barbe F, Spanish Sleep N (2015) Precision medicine in patients with resistant hypertension and obstructive sleep apnea: blood pressure response to continuous positive airway pressure treatment. J Am Coll Cardiol 66(9):1023–1032. https://doi.org/10.1016/j.jacc.2015.06.1315
Dalmar A, Singh M, Pandey B, Stoming C, Heis Z, Ammar KA, Jan MF, Choudhuri I, Chua TY, Sra J, Tajik AJ, Jahangir A (2018) The beneficial effect of weight reduction on adverse cardiovascular outcomes following bariatric surgery is attenuated in patients with obstructive sleep apnea. Sleep 41(5). https://doi.org/10.1093/sleep/zsy028
Kushida CA, Nichols DA, Holmes TH, Quan SF, Walsh JK, Gottlieb DJ, Simon RD Jr, Guilleminault C, White DP, Goodwin JL, Schweitzer PK, Leary EB, Hyde PR, Hirshkowitz M, Green S, McEvoy LK, Chan C, Gevins A, Kay GG, Bloch DA, Crabtree T, Dement WC (2012) Effects of continuous positive airway pressure on neurocognitive function in obstructive sleep apnea patients: the Apnea Positive Pressure Long-term Efficacy Study (APPLES). Sleep 35(12):1593–1602. https://doi.org/10.5665/sleep.2226
Patil SP, Ayappa IA, Caples SM, Kimoff RJ, Patel SR, Harrod CG (2019) Treatment of adult obstructive sleep apnea with positive airway pressure: an American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med
Lojander J, Maasilta P, Partinen M, Brander PE, Salmi T, Lehtonen H (1996) Nasal-CPAP, surgery, and conservative management for treatment of obstructive sleep apnea syndrome. A randomized study. Chest 110(1):114–119
Zhu B, Ma C, Chaiard J, Shi C (2018) Effect of continuous positive airway pressure on glucose metabolism in adults with type 2 diabetes: a systematic review and meta-analysis of randomized controlled trials. Sleep Breath 22(2):287–295. https://doi.org/10.1007/s11325-017-1554-x
Krieger J, Weitzenblum E, Monassier JP, Stoeckel C, Kurtz D (1983) Dangerous hypoxaemia during continuous positive airway pressure treatment of obstructive sleep apnoea. Lancet 2(8364):1429–1430
Mulgrew AT, Lawati NA, Ayas NT, Fox N, Hamilton P, Cortes L, Ryan CF (2010) Residual sleep apnea on polysomnography after 3 months of CPAP therapy: clinical implications, predictors and patterns. Sleep Med 11(2):119–125. https://doi.org/10.1016/j.sleep.2009.05.017
Mulgrew AT, Fox N, Ayas NT, Ryan CF (2007) Diagnosis and initial management of obstructive sleep apnea without polysomnography: a randomized validation study. Ann Intern Med 146(3):157–166
Nurwidya F, Susanto AD, Juzar DA, Kobayashi I, Yunus F (2016) Continuous positive airway pressure for the treatment of obstructive sleep apnea. Pneumologia 65(2):72–75
Billings ME, Kapur VK (2013) Medicare long-term CPAP coverage policy: a cost-utility analysis. J Clin Sleep Med 9(10):1023–1029. https://doi.org/10.5664/jcsm.3074
Hansen KW, Eriksen F, Thorup L, Erlandsen M, Damgård MB, Jacobsen AR, Hansen RW, Kirkegaard MG (2017) Data from: determinants for adherence to continuous positive airway pressure therapy in obstructive sleep apnea. Dryad Digital Repository. https://doi.org/10.5061/dryad.0dq86
Jacobsen AR, Eriksen F, Hansen RW, Erlandsen M, Thorup L, Damgard MB, Kirkegaard MG, Hansen KW (2017) Determinants for adherence to continuous positive airway pressure therapy in obstructive sleep apnea. PLoS One 12(12):e0189614. https://doi.org/10.1371/journal.pone.0189614
Weaver TE, Grunstein RR (2008) Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc 5(2):173–178. https://doi.org/10.1513/pats.200708-119MG
Jong CB, Li HY, Pan SL, Hsieh MY, Su FY, Chen KC, Yin WH, Chan SH, Wu YW, Wang KY, Chang KC, Hwang JJ, Wu CC (2019) Relationship between body mass index, antidiabetic agents, and midterm mortality in patients with both type 2 diabetes mellitus and acute coronary syndrome. J Am Heart Assoc 8(7):e011215. https://doi.org/10.1161/JAHA.118.011215
Young T, Skatrud J, Peppard PE (2004) Risk factors for obstructive sleep apnea in adults. JAMA 291(16):2013–2016. https://doi.org/10.1001/jama.291.16.2013
Kulkas A, Leppanen T, Sahlman J, Tiihonen P, Mervaala E, Kokkarinen J, Randell J, Seppa J, Toyras J, Tuomilehto H (2015) Amount of weight loss or gain influences the severity of respiratory events in sleep apnea. Med Biol Eng Comput 53(10):975–988. https://doi.org/10.1007/s11517-015-1290-y
Schwartz AR, O’Donnell CP, Baron J, Schubert N, Alam D, Samadi SD, Smith PL (1998) The hypotonic upper airway in obstructive sleep apnea: role of structures and neuromuscular activity. Am J Respir Crit Care Med 157(4 Pt 1):1051–1057. https://doi.org/10.1164/ajrccm.157.4.9706067
Schwab RJ (2005) Genetic determinants of upper airway structures that predispose to obstructive sleep apnea. Respir Physiol Neurobiol 147(2-3):289–298. https://doi.org/10.1016/j.resp.2005.06.006
Soriano-Co M, Vanhecke TE, Franklin BA, Sangal RB, Hakmeh B, McCullough PA (2011) Increased central adiposity in morbidly obese patients with obstructive sleep apnoea. Intern Med J 41(7):560–566. https://doi.org/10.1111/j.1445-5994.2010.02283.x
Suratt PM, McTier RF, Wilhoit SC (1988) Upper airway muscle activation is augmented in patients with obstructive sleep apnea compared with that in normal subjects. Am Rev Respir Dis 137(4):889–894. https://doi.org/10.1164/ajrccm/137.4.889
Mezzanotte WS, Tangel DJ, White DP (1992) Waking genioglossal electromyogram in sleep apnea patients versus normal controls (a neuromuscular compensatory mechanism). J Clin Invest 89(5):1571–1579. https://doi.org/10.1172/JCI115751
Carrera M, Barbe F, Sauleda J, Tomas M, Gomez C, Santos C, Agusti AG (2004) Effects of obesity upon genioglossus structure and function in obstructive sleep apnoea. Eur Respir J 23(3):425–429
Ferguson KA, Ono T, Lowe AA, Ryan CF, Fleetham JA (1995) The relationship between obesity and craniofacial structure in obstructive sleep apnea. Chest 108(2):375–381
Reutrakul S, Mokhlesi B (2017) Obstructive sleep apnea and diabetes: a state of the art review. Chest 152(5):1070–1086. https://doi.org/10.1016/j.chest.2017.05.009
Tantucci C, Scionti L, Bottini P, Dottorini ML, Puxeddu E, Casucci G, Sorbini CA (1997) Influence of autonomic neuropathy of different severities on the hypercapnic drive to breathing in diabetic patients. Chest 112(1):145–153
Bottini P, Redolfi S, Dottorini ML, Tantucci C (2008) Autonomic neuropathy increases the risk of obstructive sleep apnea in obese diabetics. Respiration 75(3):265–271. https://doi.org/10.1159/000100556
Guest CB, Park MJ, Johnson DR, Freund GG (2008) The implication of proinflammatory cytokines in type 2 diabetes. Front Biosci 13:5187–5194
Ahima RS, Osei SY (2008) Adipokines in obesity. Front Horm Res 36:182–197. https://doi.org/10.1159/0000115365
Funding
Xuxia Tang received grants from the Natural Science Foundation of Zhejiang Province (Y17H130009).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants
Ethical approval was obtained in the original study.
Informed consent
The requirement for informed consent was waived because of the retrospective study design.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Huang, X., Bao, L., Tang, X. et al. Association between body mass index and effectiveness of continuous positive airway pressure in patients with obstructive sleep apnea: a retrospective study. Sleep Breath 24, 1075–1081 (2020). https://doi.org/10.1007/s11325-019-01960-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-019-01960-x