Abstract
With the expected rise of patients with osteoporosis-induced fractures, it has become increasingly urgent to design and use specialized health education materials to ease pain and improve bodily functions. This study designed web-based app for pain relief instructions for women with spinal compression fractures. An observational study was conducted at an educational hospital in northern Taiwan between October 2018 and September 2019. Using random assignment based on their presentation order, we divided patients into an experimental (n = 87) and control (n = 84) group. The experimental and control groups received web app healthcare instructions for relieving back pain and regular nursing care instructions, respectively. Taiwanese versions of the Brief Pain Inventory and 36-Item Short Form Health Survey were used to collect data. We collected patients’ pain rating data the day before, one month after, and three months after providing them with the instructions. Pain intensity differed significantly between the two groups, and it interacted with time. Pain impact did not significantly differ between groups; however, it interacted with time. Relieving back pain is a primary concern for those affected by it. This study presents a consistent, easy-to-use instructional healthcare web-based app that may provide knowledge of pain relief and reduce mobility impairments.
Trial registration
first registration on 18/05/2022, NCT05386212.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The average life span in Taiwan has substantially increased due to scientific advances and improvements in the socio-economic environment. A 2004–2014 report indicated that the average life span for women was 79.04 years [1, 2]. A more recent 10-year epidemiological study found that approximately 20% of Taiwanese women aged >65 years had osteoporosis-induced spinal compression fractures [3]. The probability of having a spinal compression fracture is about two to four times higher than having cerebrovascular disease—one of Taiwan’s top three causes of death [3]. The most observed symptom of spinal compression fractures in female patients is severe chronic lower back pain—a form of non-cancer-related pain that typically affects patients’ quality of life (QOL) [4, 5]. Research suggests that spinal compression fractures lead to acute and chronic back pain, reduced bodily function, and anxiety regarding recurrence [6]. Ballane et al. also stated that back pain hinders patients’ ability to perform physical activities because they fear the recurrence of pain or fracture [7]; Hindered activities include bending down, carrying objects, cooking, household chores, and climbing stairs [8].
Current health education regarding pain treatment primarily focuses on cancer-related and postoperative pain, along with preventive measures against such pain [9, 10]. Patients with spinal fractures are typically provided with only general healthcare instructions, which lack consistency and standardization [11]. A survey on using a one-page health education flyer found that only 52.2% of the patients who read the flyer followed its directions; the study indicated that participants had difficulty keeping track and delivered only limited guidance [12]. The essential needs of patients with spinal compression fractures include appropriate pain relief methods, supplementary instruments (e.g., back racks), recovery of bodily functions, reduction of fracture recurrences, and the avoidance of high medical costs [11]. However, due to long-term negligence concerning pain care, associated medical resources, and educational insufficiencies, back pain has been ineffectively addressed in the worldwide [13]. As the population with osteoporosis-induced fractures is expected to rise, it is increasingly urgent that specialized health education materials to ease pain, improve bodily functions, and enhanced QOL be designed and utilized.
1.1 Compression fractures of the spine
Women typically lose 2–3% of their osteoid tissue every 6–10 years after menopause due to a lack of estrogen. While bone composition remains unchanged, its density starts to decrease; this indicates reduced amounts of minerals inside osteoid tissue, referred to as osteoporosis [1, 13]. Spinal compression fractures, caused by gaps between vertebrae that widen and become flimsy due to the loss of osteoid tissue, are one result of osteoporosis [7, 8]. Back and waist pain, a hunched back, and height loss can be triggered after the vertebrae deteriorate to a certain degree. As osteoporosis in an individual worsens, the risk of spinal compression fractures caused by sitting or falling increases [14].
According to a study by the National Osteoporosis Foundation, 15% of post-menopausal American women and 35% of women aged >65 years had osteoporosis. In the U.S., 1.5 million people experience fractures of the spine, hipbone, and wrist each year (40%, 20%, and 15%, respectively). In Taiwan, 60,000 people experience osteoporosis-induced fractures yearly, most seen in middle-aged and older women [15]. The frequency and intensity of spinal fractures are similar to those in hip fractures, which may lead to fractures of other body parts, acute and chronic back pain, reduced QOL, or even death [2].
1.2 Back pain
Back pain is a symptom rather than a concrete diagnosis [3,4,5]. It can refer to the entire back, including the waistband and areas surrounding the spine on both sides of the body. Uncomfortable feelings in the areas mentioned above are thus defined as back pain [15]. When classified in the affected location, spinal compression fractures typically result in middle back pain, which occurs below the shoulder blade’s middle part and above the ribs, i.e., the area where the thoracic vertebrae meet the lumbar vertebrae. Depending on specific characteristics, pain can also be distributed to the fourth and fifth lumbar vertebrae because of muscular spasms, broadly defined as low back pain in clinical diagnoses [13, 14].
Recently, back pain from spinal compression fractures has been classified by the World Health Organization (WHO) as a form of non-cancer-related pain [4]. The most significant concern when caring for patients with spinal compression fractures is the overuse of painkillers and the resulting side effects. Some people cease receiving medical care because of this concern [13]. Jun et al. found that the more confident patients with cancer are regarding painkillers, the fewer the effects they experience, resulting in more severe pain [14]. A study on low back pain found that chronic back pain induced nausea, weakness, and low blood pressure [15]. Prolonged activities or unchanged gestures exacerbated the degree of pain, which could typically be observed through patients’ facial and vocal expressions. A lifestyle change can alter a patients’ degree of pain, and lingering pain affects patients’ QOL [9,10,11]. In 2017, the WHO urged healthcare professionals to treat pain by emphasizing that chronic pain is a disease.
Back pain also affects post-menopausal women. One study noted that having a sore waist or backache are significant health complaints among menopausal women, causing 80% of the medical expenses for such women [7, 14]. In the U.S., such pain-related expenditures amounted to approximately NT $10 billion a decade ago [13, 14]. Gibbs also noted that back pain caused about 2–5% of the losses in overall U.S. productivity and an 8% reduction in total salaries [15]. A survey of Taiwan’s 2018 outpatient services found that there were 5.4 million such cases that year; these cases cost NT $3 billion in medical expenses and were the third most common cause for seeking outpatient services [13]. A 2017 study found back pain to be the second most common problem treated through outpatient services, following the common cold [16, 17], and spinal compression fractures have been reported among the top five most common diagnoses [18]. Phinyomark et al. stated that the best way to address back pain is through education and prevention [19]. Health education promotes patient knowledge regarding various diseases to change their mindsets and behaviors. Gibbs and Liu noted that health education consists of pre-meditated learning experiences promoting self-discipline in healthcare [15, 20]. One reason to apply health education to the issue of back pain is to enhance patients’ ability to maintain their own health and promote their QOL. Hospital health education improves communication between healthcare providers and patients and reduces disease recurrence, thus decreasing disputes and medical costs [21]. The more time spent on health education during outpatient services, the less often disease recurrence will occur [22].
McCarthy argued that pain-related education enhances the ability to treat pain and teaches patients to take effective steps to ease their pain [23]. A biomechanics study regarding low back pain evaluation and prevention found that back pain prevention education affects patients’ mindsets [18,19,20]. However, there is little data available showing any associated behavioral changes. A study conducted in Taiwan found that patients with osteoporosis-induced spinal compression fractures could see significant improvements in their symptoms within 2–3 weeks if they followed advice to use a back rack, paid attention to their movements during daily activities, and took proper osteoporosis medications or painkillers [24].
In an effectiveness study concerning oral health instructions, McCarthy found that 24% of patients did not follow doctors’ suggestions regarding medication, resulting in U.S. $1.368 billion in medical expenses each year [25, 26]. In another effectiveness analysis of individual health education on patients’ knowledge of disease, attitudes toward healthcare, and behaviors, the health education manual combined with one-on-one instructions resulted in better responses than the manual alone [27].
1.3 QOL
QOL is an abstract concept with objective and subjective components broadly used since the 1960s. It is a personal feeling, and it indicates life satisfaction and happiness [28], depending on the context. For patients, it is a vital part of the healthcare process [29]. In a study of the QOL of patients with lumbar vertebra, Addington demonstrated that the more pain patients feel, the less satisfied they were with work, family, social contacts, and life in general [30]. Garg et al. conducted a medical survey of female patients with spinal compression fractures using the SF-36 QOL Scale; they discovered that these patients displayed lower scores on the scale’s psychological and physical aspects [25,26,27]. Stanghelle et al. conducted another survey of menopausal women with and without spinal compression fractures using the Orthognathic QOL questionnaire; they found that 40% of patients with a spinal fracture were depressed and had an unsatisfactory QOL because their bodily functions were reduced by fracture-induced back pain [29]. Yangyang et al. used the SF-36 to analyze how back pain is related to patients’ QOL. They observed that patients with back pain had lower QOL scores due to mental and physical problems and limited bodily functions [31].
Researchers have also used the SF-36 scale for patients with slipped discs and found that their QOL was affected by their degree of symptoms and pain [26,27,28], with 47% of the QOL results being related to their symptoms. Shangjin et al. conducted the Euro-QOL parallel survey with 751 European menopausal women with low osteoid density. They found patients had less pain recognition, worse bodily functions, and poorer health conditions than women without the condition [29, 30]. Their study used the QOL questionnaire to survey 105 osteoporotic female patients and revealed that 63% of QOL can be explained by spinal fractures, health recognition, and demographic factors [31]. In a study of eight major chronic diseases (including back pain), Huang et al. found that bodily functions and health recognition were the main factors indicating health-related QOL [32].
2 Method
2.1 Study plan
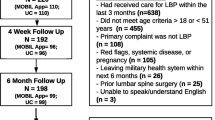
We investigated how low back pain health education affects patients’ health at different time points using a longitudinal experimental research design. An experimental group (n = 87) and a control group (n = 84) were measured regarding their degree of pain and QOL. The experimental group received a web app health education consultation and the control group received regular healthcare instructions. Patients’ degree of back pain was evaluated in the first and second months after hospital discharge. Patients were randomly allocated into groups by block randomization, and they did not interact with each other (see Fig. 1).
2.2 Objective
This study primarily involved the development of an app-based instant feedback system that provides prompt guidance regarding the relevant issues to be considered when suffering from back pain. The system provides the public with a convenient and proper source of home health care knowledge, which can improve their knowledge, perceptions, and skills concerning medication safety and health care and consequently enhance the quality and value of self-care.
2.3 Design
This study adopted an observational study design and a random allocation method based on the patients’ clinic visits from October 2018 to September 2019. A total of 171 people were recruited; using random assignment based on their presentation order, we divided participants into an experimental (n = 87) and control (n = 84) group. This study explored the effect of the back pain health care web app on lower back pain and changes in taking medicine related knowledge. The experimental and control groups were surveyed using a questionnaire, and their back pain knowledge with activities was evaluated during the pre-test. The experimental group received a back pain healthcare web app regarding patient self-care. The control group received routine outpatient treatment and nursing guidance. A post-test was conducted three months later to assess if there was any improvement regarding their lower back pain.
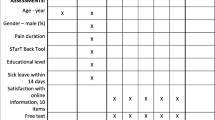
2.4 Research tools
2.4.1 Basic patient information questionnaire
The questionnaire content included items such as age, age at menopause, age at first fracture, marital status, education level, occupation, financial status, religious affiliation, height, weight, medical history, history of back pain, duration of back pain, management of back pain and affected areas, number of fractures, use of alternative rehabilitation therapies and the related costs, and use of analgesics.
2.4.2 The Chinese version of the brief pain inventory
We used the Taiwanese version of the Brief Pain Inventory, designed initially to measure cancer-related pain. Taiwanese scholars translated this scale from the Pain Scale developed by Cleeland for cancer pain [33]. The measurement utilizes a horizontal, equidistant 0–10 scale (0 = no pain and 10 = extreme pain). The inventory allows for the examination of time points over a 24-hour or week-long period. The evaluation comprises two primary components: pain intensity (current pain level, average pain intensity, and highest and lowest pain level experienced) and pain impact (activities of daily living, emotions, walking ability, interpersonal relationships, sleep, and leisure). In a study of Taiwanese patients, the four-item pain intensity scale of the inventory had a test-retest reliability of 0.79 and a Cronbach’s α of 0.81. The values for the seven-item pain interference scale were 0.81 and 0.89, respectively. Cronbach’s α in the present study was 0.83 [31, 33].
2.4.3 SF-36 QOL scale
We used the Taiwanese version of the SF-36 QOL Scale (Medical Outcomes Survey—Short Form), translated and consolidated by Prof. Jui-Fen Lu [34]. The original scale comprised 36 questions and eight dimensions: physical functioning (P.F.), role limitations due to physical problems (R.P.), role limitations due to emotional problems (RE), body pain (B.P.), general health (G.H.), vitality (V.T.), social function (S.F.), mental health (M.H.), and reported health transition. Lyons et al. performed an SF-36 reliability and validity test focusing on elderly patients and found that the eight subscales all had Cronbach’s α values that exceeded 0.80; this indicates that the scale can effectively distinguish health statuses. In another study, local scholars used the Taiwanese version of the SF-36 to examine the QOL of adults aged ≥50 years who underwent health checkups; they found that Cronbach’s α values of the eight dimensions ranged from 0.80–0.90, and the discriminant validity was 100%.
2.4.4 Back pain health care web app design
The web app content was developed based on the clinical experiences of the researchers and resources gathered from numerous experts (including physicians, specialist nurse practitioners, dieticians, and physical therapists). Patients were educated on home care for treating back pain primarily through pictures and texts and by applying the Q&A format. The educational content comprised four main components: understanding spinal compression fractures, the characteristics of back pain, related measures, physical activities, precautions, and simple self-assessment of the web app.
2.5 Statistical analysis
We analyzed the data with IBM SPSS for Windows 25.0 and a general linear mixed effect model (GLMM). Descriptive methods such as independent sample t-tests, percentages, and chi-square (χ2) tests were applied to two sets of demographic data and disease specifications. Independent and paired samples t-tests were conducted regarding the change in QOL before and after implementing the intervention. P-values < .05 were deemed significant.
This study used the GLMM because it is suitable for measuring changes over time and repeated pain measurements for individual cases. This method enhances statistical power and elicits more accurate results for long-term change forecasts since it considers whether the time and group change the degree of pain. Thus, it is an adjustable, re-measurable variable.
3 Results
3.1 Comparing the basic data and pre-test dependent variable data between groups
The basic data of the experimental and control groups are as follows. The average ages were 66.92 ± 4.79 and 66.47 ± 7.423, respectively. Menopause ages were 50.95 ± 1.84 and 50.88 ± 1.86 years, respectively. The mean fracture times were 1.385 ± 0.49 and 1.185 ± 0.39 times, respectively. The participants’ age at the time of primary fracture were 62.51 ± 3.22 and 61.82 ± 3.89 years, respectively. Most participants were married, unemployed, and living with their families. The length of time pain lasted was typically from 6 to 12 months. Most participants sought folk customs and alternative therapies and took painkillers as back pain treatment. Regarding back pain treatment costs, most treatments were more than NTD 5000 per year. Based on the above data and the analysis results of the Chi-square and independent t-tests, the experimental and control groups were compared in terms of basic data. There were no statistically significant differences in age, menopausal age, fracture times, age of fractures, marital status, occupation, whether participants live with family members, onset of back pain, back pain treatment, presence/absence of regular painkiller use, or whether the costs of back pain treatment were more than NTD 5000 (P > 0.05). The homogeneity of the two groups was high (see Table 1).
This study’s independent t-tests and χ2 results showed no significant differences between the control and experimental groups, indicating that the two groups had a high degree of homogeneity. Fisher’s skewness coefficient was used to test whether the data were normally distributed, which revealed no deviation (± 1.96) for the following items: age at menopause, age at fracture, education level, onset of back pain, back pain management methods, and the regular use of analgesics. Regarding the pre-test data for the pain-related items and sub-items and the QOL dimensions between groups, there were no significant differences. The two groups’ pre-test dependent variable data shared a high degree of homogeneity.
3.2 Comparing back pain, QOL, and other data between groups
As assessed by the Chinese version of the brief pain Inventory (BPI-C), the average pain intensity scores in the pre- and post-tests (1 month) of the experimental and control groups were 5.83 ± 0.852, 4.38 ± 0.929 vs. 5.74 ± 0.828, 4.66 ± 0.857. The difference in mean pain intensity between the two groups was statistically significant, as measured by an independent t-test (P = 0.007, P < 0.05). The difference between the experimental and control groups in the pre- and post-tests (2 months) was also statistically significant (P = 0.001, P < 0.01). There was a statistically significant difference in the mean pain impact between the two groups in the pre- and post-tests (1 month) (P = 0.001, P < 0.05). The mean effect of back pain was also statistically significant between the pre- and post-tests (2 months) (P = 0.003, P < 0.01). The pain intensity and impact of the cases was repeatedly measured in this study; whether time and group (fixed effects) and the random effect of the participants would cause various changes in pain intensity were considered. Therefore, the General Linear Mixed-effect Model (GLMM) was applied to the analysis to correct for interactions between repeated measurement variables. The results indicate an interaction between time and group regarding mean pain intensity. The mean predictive value (β) was 7.044, P = 0.001, and the group effect value (β) was 3.566, P = 0.001. Tracking observations in the experimental and control groups over time, the predicted value (β) one month after the intervention was −1.263 and the standard error (S.E.) was 0.068, P = 0.001, which is statistically significant. The predicted value (β) two months after the intervention was −1.512, and the standard error (S.E.) was 0.130, P = 0.001, which is also statistically significant. The findings indicate that the experimental group showed significant differences between the two groups after the intervention; the effect was achieved within one month, which could be postponed to two months (see Table 2).
There was an interaction between time and group for average pain intensity and impact. Follow-up observations of the control and experimental groups over time indicated a significant difference between the data collected prior to the intervention and one month after the intervention and a significant difference between the data collected prior to and two months after the intervention (see Fig. 2). Significant differences were also observed regarding the average QOL scores of the two groups. Comparing the differences in the eight QOL dimensions showed no significant difference, except for the physiological function dimension (P = .364), as shown in Table 3 and Fig. 3. As for the differences between the groups concerning pre- and post-test data, regarding the regular use of analgesics and costs over NT $5000 for back pain treatments, χ2 was 9.117. This indicates significant differences between the groups. The McNemar test revealed a significant difference in the experimental group regarding the regular use of analgesics and the cost of over NT $5000 for back pain treatments. However, no significant differences were detected in the control group, as shown in Table 4.
3.2.1 Subjective appraisal of the web app’s effectiveness by the participants in the experimental group
The subjective appraisal of the web app’s effectiveness by the participants in the experimental group included the following: clarification of misconceptions regarding the use of analgesics, willingness to express one’s feelings of pain, the ability to engage in self-care (empowerment), and physical exercises, acquiring the ability to self-monitor and record back pain levels, and an increase in one’s confidence in engaging in rehabilitation exercises. More than half the participants felt that the web app could be conveniently accessed, helped substantially regarding self-care at home, could increase patients’ confidence, and was worth promoting.
4 Discussion
The average time of the first fracture for participants in the present study was 12 years after the onset of menopause, which was compared to the results of overseas studies. Patients were prone to spinal compression fractures 6–10 years after the onset of menopause. Future studies should examine when treatments are sought to explore whether the above trend was caused by a lag between the time at first fracture and when patients seek Western medical treatment.
This study’s pre-test data for the use of analgesics indicated that more than half the participants in both groups were not taking analgesics regularly; hence, there were non-significant differences between groups. For back pain, the web app and personal consultation-based intervention reduced the barriers hindering the use of analgesics in several areas: clarifying drug types, effects, and side effects; the willingness to express one’s feelings of pain; and the role of being a good patient [13, 14]. During the post-test period, there was a substantial increase in the number of experimental group participants who used analgesics regularly. In contrast, there was a decrease in the number of participants who did so in the control group. The differences between groups can be attributed to the app’s detailed descriptions of analgesic use and personal phone consultations [25]. This study’s findings indicate that back pain education should include not just back pain management and precautions but also address the problems linked to misconceptions regarding analgesic use.
Excluding the monthly cost of outpatient surgical treatments for spinal back pain, participants in both groups incurred monthly expenses of over NT $5000 for folk and alternative therapies. Furthermore, given the current absence of clear regulations to manage these therapies, and the lack of data regarding the public’s understanding of them, there is significant room for exploring the problems associated with such forms of therapy.
While the effects of average pain intensity were observed in the first month and persisted into the second month, no previous studies have examined the pain associated with spinal compression fractures. Although local studies of a pain education intervention for patients with cancer have shown that implementing proper pain education can effectively alleviate pain intensity. However, no follow-up was performed to ascertain the persistent effects of such interventions. Furthermore, the participants of these two studies had been diagnosed with different diseases, making it challenging to compare. In the present study, the control group’s average pain intensity exhibited a floating trend and declined during the post-test and post-post-test periods (compared to the pre-test period); however, an increase was observed between the post-test and post-post-test periods. This could be attributed to providing a single care routine guidance session and a single health education leaflet only during the pre-test period; this could have resulted in the lack of continuing consultation and, consequently, the differences between groups [35,36,37].
This study’s findings concerning the effectiveness of the intervention for pain impact sub-items were as follows. Group and time shared an interactional relationship concerning general activities (such as eating, toilet use, and bathing), walking ability, normal work ability (going out to work or daily cleaning), interactions with others, and leisure activities. However, no significant effects were observed between the groups. Moreover, group and time shared an interactional relationship concerning emotions and sleep, and a significant effect was observed between groups. These results were similar to those for the implementation of interventional pain education for patients with cancer; that is, the implementation of proper pain education can quickly (after a week) elicit improvements regarding pain impact, leisure activities, and emotions, leading to improvements in the items, general activities, interactions with others, and sleep only after a moderate time period (after two weeks). Since no follow-up has been conducted, it was not possible to ascertain whether these improvements persisted [36, 38, 39].
The health education intervention did not achieve a significant difference for the PF QOL dimension. The reasons are as follows, examined the effects of medical interventions on QOL linked to eight chronic diseases (including back pain). They found that the P.F. and G.H. dimensions were influenced to a greater degree. These findings differ from the present study. This difference could be attributed to the fact that researcher. Examined medical interventions, including surgical treatment for patients with back pain, while our study examined a health education intervention. Second, the P.F. questionnaire is unsuitable for female patients with spinal compression fractures. Regarding treatments for their specific conditions, the patients were informed that they should not perform bending motions, lift heavy objects, or engage in strenuous activities. Patients with spinal compression fractures were also prohibited from lifting heavy objects while undergoing health education. However, the P.F. questionnaire content primarily covers strenuous and moderate activities. Since these patients could engage in the activities listed in the questionnaire, no significant differences were identified between groups. Third, the patients had a mean age of 66.69 ± 1.85 years and did not engage in strenuous, time-consuming, or continual activities. Therefore, no significant differences between groups were identified. Finally, the health education intervention affected patients’ overall QOL after two months. Concerning overall QOL, the experimental and control groups’ post-post-test scores (two months) were, on average, higher than their pre-test scores (25.22 ± 6.71 vs. 13.42 ± 5.30). This indicates that both groups experienced improved QOL. Thus, the health education intervention positively affected overall QOL. However, the continuing health education and consultation that the experimental group received allowed the participants to achieve better results than those in the control group [11, 40].
5 Conclusion
This study explored the effectiveness of web-based app that may provide knowledge of pain relief and reduce mobility impairments and improving the QOL of female patients with spinal compression fractures and back pain. Implementing back pain health education led to a greater degree of improvement in the experimental group compared to the control group. Concerning the difference in the post-test (one month) and post-post-test (two months) results for average pain intensity and pain impact, both groups showed improvement over time; the experimental group experienced a significantly greater degree of improvement than the control group. Second, the intervention and consultation helped to clarify patients’ misconceptions concerning analgesic use. Third, two months after the intervention and consultation, significant improvements were observed in seven dimensions: RP, BP, GH, VT, S.F., RE, and MH.
Data availability
The data presented in this study are openly available in Research Data Alliance repository, https://www.rd-alliance.org/node/58743/file-repository
References
Bandeira PM, Reis FJJ, Sequeira VCC, Chaves ACS, Fernandes O, Arruda-Sanchez T (2021) Heart rate variability in patients with low back pain: a systematic review. Scand J Pain 21:426–433. https://doi.org/10.1515/sjpain-2021-0006
Buchbinder R, Johnston RV, Rischin KJ, Homik J, Jones CA, Golmohammadi K, Kallmes DF (2018) Percutaneous vertebroplasty for osteoporotic vertebral compression fracture. Cochrane Database Syst Rev 4:CD006349. https://doi.org/10.1002/14651858.CD006349.pub4
Chu W, Tsuei YC, Liao PH, Lin JH, Chou WH, Chu WC, Young ST (2013) Decompressed percutaneous vertebroplasty: a secured bone cement delivery procedure for vertebral augmentation in osteoporotic compression fractures. Inj 44:813–818. https://doi.org/10.1016/j.injury.2012.10.017
Feng L, Feng C, Chen J, Wu Y, Shen JM (2018) The risk factors of vertebral refracture after kyphoplasty in patients with osteoporotic vertebral compression fractures: a study protocol for a prospective cohort study. BMC Musculoskelet Disord 19:195. https://doi.org/10.1186/s12891-018-2123-6
Gambacciani M, Levancini M (2014) Management of postmenopausal osteoporosis and the prevention of fractures. Panminerva Med 56:115–131
Rizzo M, Tammaro G, Guarino A, Basso M, Cozzolino A, Mariconda M (2022) Quality of life in osteoporotic patients. Orthop Rev 14:38562. https://doi.org/10.52965/001c.38562
Ballane G, Cauley JA, Luckey MM, El-Hajj Fuleihan G (2017) Worldwide prevalence and incidence of osteoporotic vertebral fractures. Osteoporos Int 28:1531–1542. https://doi.org/10.1007/s00198-017-3909-3
Byun JH, Jang S, Lee S, Park S, Yoon HK, Yoon BY et al (2017) The efficacy of bisphosphonates for prevention of osteoporotic fracture: an update meta-analysis. J Bone Metab 24:37–49. https://doi.org/10.11005/jbm.2017.24.1.37
Vambheim SM, Kyllo TM, Hegland S, Bystad M (2021) Relaxation techniques as an intervention for chronic pain: a systematic review of randomized controlled trials. Heliyon 7:e07837. https://doi.org/10.1016/j.heliyon.2021.e07837y
Fillingim RB (2017) Individual differences in pain: understanding the mosaic that makes pain personal. Pain 158:S11–S18. https://doi.org/10.1097/j.pain.0000000000000775
Traeger A, Buchbinder R, Harris I, Maher C (2017) Diagnosis and management of low-back pain in primary care. CMAJ 189:E1386–E1395. https://doi.org/10.1503/cmaj.170527
Chen YC, Zhang L, Li EN, Ding LX, Zhang GA, Hou Y, Yuan W (2019) Unilateral versus bilateral percutaneous vertebroplasty for osteoporotic vertebral compression fractures in elderly patients: a meta-analysis. Medicine 98:e14317. https://doi.org/10.1097/MD.0000000000014317
Balkarli H (2015) Treatment of osteoporotic vertebral compression fractures with percutaneous vertebroplasty under local anesthesia: clinical and radiological results. Int J Clin Exp Med 8:16287–16293
Jun M, Dou W, Xu XS, Qiang L (2020) Comparison of early results of vesselplasty and percutaneous vertebroplasty in the treatment of elderly patients with osteoporotic vertebral compression fracture. Res Square https://doi.org/10.21203/rs.3.rs-17452/v1. Accessed 17
Gibbs JC, MacIntyre NJ, Ponzano M, Templeton JA, Thabane L, Papaioannou A, Giangregorio LM (2019) Exercise for improving outcomes after osteoporotic vertebral fracture. Cochrane Database Syst Rev CD008618 https://doi.org/10.1002/14651858.CD008618.pub3
Wang BJ, Syu FJ (2016) Acceptability of mobile health apps for medical care measured using UTAUT2. J Gerontechnol Serv Manage 4:483–494
Kaushik S, Gandhi C (2022) Capability-based access control with trust for effective healthcare systems. Int J Cloud Appl Comput 12:1–28. https://doi.org/10.4018/IJCAC.297107
Halilaj E, Rajagopal A, Fiterau M, Hicks JL, Hastie TJ, Delp SL (2018) Machine learning in human movement biomechanics: best practices, common pitfalls, and new opportunities. J Biomech 81:1–11. https://doi.org/10.1016/j.jbiomech.2018.09.009
Phinyomark A, Petri G, Ibáñez-Marcelo E, Osis ST, Ferber R (2018) Aalysis of big data in gait biomechanics: current trends and future directions. J Med Biol Eng 38:244–260. https://doi.org/10.1007/s40846-017-0297-2
Liu HY, Chen TJ (2017) Current state and development of m-health app usage. Clin Med 80:507–510
Ching WY (2014) The user-centric based mobile health apps to facilitate patients while receiving medical treatments. J Hosp Bimonth 47:25–29
Jafari J, Moonaghi HK, Zary N, Masiello I (2016) Exploring educational needs and design aspects of internet-enabled patient education for persons with diabetes: a qualitative interview study. BMJ Open 6:1–7. https://doi.org/10.1136/bmjopen-2016-013282
McCarthy J, Davis A (2016) Diagnosis and management of vertebral compression fractures. Am Fam Physician 94:44–50
Fisher C, Tee J (2016) Editorial: the utility of the modified frailty index for risk stratification in patients undergoing spine surgery. J Neurosurg Spine 25:535–536. https://doi.org/10.3171/2016.1.SPINE151261
Partridge JS, Harari D, Dhesi JK (2012) Frailty in the older surgical patient: a review. Age Ageing 41:142–147. https://doi.org/10.1093/ageing/afr182
Garg B, Dixit V, Batra S, Malhotra R, Sharan A (2017) Non-surgical management of acute osteoporotic vertebral compression fracture: a review. J Clin Orthop Trauma 8:131–138. https://doi.org/10.1016/j.jcot.2017.02.001
Amoretti A (2018) Percutaneous vertebroplasty in tumoral spinal fractures with posterior vertebral wall involvement: feasibility and safety. Eur J Radiol 104:38–42. https://doi.org/10.1016/j.ejrad.2018.04.010
Huang ZF, Xiao SX, Liu K, Xiong W (2019) Effectiveness analysis of percutaneous kyphoplasty combined with zoledronic acid in treatment of primary osteoporotic vertebral compression fractures. Pain Physician 22:63–68
Stanghelle B, Bentzen H, Giangregorio L, Pripp AH, Bergland A (2019) Associations between health-related quality of life, physical function and pain in older women with osteoporosis and vertebral fracture. BMC Geriatr 19:298. https://doi.org/10.1186/s12877-019-1268-y
Lin S, Cai X, Cheng Q, Chen C, Cao X, Yang F, Fan Y (2022) Association between bone turnover markers, BMD and height loss of cemented vertebrae after percutaneous vertebroplasty in patients with osteoporotic vertebral compression fractures. J Orthop Surg Res 17:202. https://doi.org/10.1186/s13018-022-03087-4
Ma Y, Wu X, Xiao X, Ma Y, Feng L, Yan W, Chen J, Yang D (2020) Effects of teriparatide versus percutaneous vertebroplasty on pain relief, quality of life and cost-effectiveness in postmenopausal females with acute osteoporotic vertebral compression fracture: a prospective cohort study. Bone 31:115154. https://doi.org/10.1016/j.bone.2019.115154
Kong M, Zhou C, Zhu K, Zhang Y, Song M, Zhang H, Tu Q, Ma X (2019) 12-month teriparatide treatment reduces new vertebral compression fractures incidence and back pain and improves quality of life after percutaneous kyphoplasty in osteoporotic women. Clin Interv Aging 14:1693–1703. https://doi.org/10.2147/CIA.S224663
Ger LP, Ho ST, Sun WZ, Wang MS, Cleeland CS (1999) Validation of the brief pain inventory in a Taiwanese population. J Pain Symptom Manag 18:316–322. https://doi.org/10.1016/s0885-3924(99)00087-1
Lu JF, Tseng HM, Tsai YJ (2003) Assessment of health-related quality of life in Taiwan (I): development and psychometric testing of SF-36 Taiwan version. Taiwan J Public Health 22:501–511
Yu C, Li J, Li X, Ren X, Gupta BB (2018) Four-image encryption scheme based on quaternion Fresnel transform, chaos and computer generated hologram. Multimed Tools Appl 77:4585–4608. https://doi.org/10.1007/s11042-017-4637-6
Dwivedi RK, Kumar R, Buyya R (2021) Gaussian distribution-based machine learning scheme for anomaly detection in healthcare sensor cloud. Int J Cloud Appl Comput 11:52–72. https://doi.org/10.4018/IJCAC.2021010103
Peraković D, Gaurav A, Psannis K (2021) Security of cloud-based medical internet of things (MIoTs): a survey. Int J Softw Sci Comput Intell 14:1–16. https://doi.org/10.4018/IJSSCI.285593
Kaur M, Singh D, Kumar V, Gupta BB, Abd El-Latif AA (2021) Secure and energy efficient-based e-health care framework for green internet of things. IEEE Trans Green Commun Netw 5:1223–1231. https://doi.org/10.1109/TGCN.2021.3081616
Zhang JN, He X, Fan Y, Du JP, Hao DJ (2019) Risk factors for conservative treatment failure in acute osteoporotic vertebral compression fractures (OVCFs). Arch Steoporos 14:24. https://doi.org/10.1007/s11657-019-0563-8
Gao W, Chen Y, Wang X, Liu G, Cui K, Guo J, Zheng J, Hao Y (2023) Establishment and verification of a predictive nomogram for new vertebral compression fracture occurring after bone cement injection in middle-aged and elderly patients with vertebral compression fracture. Orthop Surg 15:961–972. https://doi.org/10.1111/os.13655
Acknowledgements
The authors thank the staff of the Medical Quality Center, Cheng Hsin General Hospital for their assistance in the research process.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The research plan was approved by the Institution Review Board of Cheng Hsin General Hospital (IRB number: 108A-06). All methods were carried out in accordance with relevant guidelines and regulations. Participants’ written informed consents were obtained prior to the study. All patient/personal identifiers were removed or disguised for anonymity.
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liao, PH., Chu, W. Exploring the impact of an instructional web-based healthcare app for relieving back pain from spinal compression fractures: an observational study. Multimed Tools Appl 83, 33295–33311 (2024). https://doi.org/10.1007/s11042-023-16801-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11042-023-16801-z