Abstract
Background
Breast cancer (BC) is a disease with variable morphology, clinical behaviour and response to therapy. Identifying factors associated with the progression of early-stage BC can help understand the risk of metastasis and guide treatment decisions. Myxovirus resistance 1 (MX1), which is involved in the cellular antiviral mechanism, plays a role in some solid tumours; however, its role in invasive BC remains unknown. In this study, we aimed to explore the clinicopathological and prognostic significance of MX1 in BC.
Methods
MX1 was assessed at the protein level using tissue microarrays from a large well-annotated BC cohort (n = 845). The expression of MX1 mRNA was assessed at the transcriptomic level using the Molecular Taxonomy of Breast Cancer International Consortium (METABRIC; n = 1980) and validated using three publicly available cohorts on Breast Cancer Gene-Expression Miner (bc-GenExMiner version 4.4). The associations between MX1 expression and clinicopathological factors, and outcome were evaluated.
Results
High MX1 protein expression was associated with features of aggressiveness, including large tumour size, high tumour grade, high Nottingham prognostic index scores, hormone receptor negativity and high Ki67 expression. High MX1 expression showed an association with poor patient outcome and it was an independent predictor of short BC-specific survival (p = 0.028; HR = 1.5; 95% CI = 1.0–2.2). Consistent with the protein results, high MX1 mRNA levels showed an association with features of aggressive behaviour and with shorter survival.
Conclusion
This study identified MX1 as an independent predictor of poor outcome in patients with BC. Further functional studies are needed to investigate the biological role of MX1 in BC and its potential value as a therapeutic target.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer (BC) comprises different diseases that show distinct molecular features, clinical behaviour and response to therapy. Therefore understanding BC biology and defining a personalised therapy method remains a challenge [1]. Deciphering the molecular mechanisms and biological processes controlling BC progression is important to develop better treatment strategies and ultimately improve patient outcome.
One of the interferon‐induced GTPases that belongs to the dynamin superfamily of large GTPases is MX1 protein, also known as MXA, which is encoded by Myxovirus resistance 1 (MX1) gene [2]. Previous studies have indicated that MX1 has many features, including a tendency to self‐assemble, low affinity for guanosine triphosphate (GTP) and high intrinsic rate of GTP hydrolysis. MX1 is mainly localised in the cytoplasm and shows a granular staining pattern that may be associated with cytoskeletal structures [3]. MX1 releases GTP, which plays a role in metabolising the protein that contributes to the cellular antiviral mechanism [4]. MX1 is overexpressed and appeared to play a role in a variety of cancers but its effect remains controversial. Many interferon-stimulated genes (ISGs) can inhibit the motility of the transformed cells and the invasion of normal tissues. In most tissues, MX is highly induced by the ISG, particularly interferon (IFN) α and β. MX1 also has a role in the inhibition of motility and invasiveness in some cancers, such as prostate carcinoma and melanoma [5, 6]. However, MX1 appears to have different effects in other cancers. It was observed that reduced MX1 level can suppress apoptosis during cancer development [6]. In colorectal cancer, MX1 protein is overexpressed and plays a significant role in lymph node metastasis. An in vitro study conducted in colorectal carcinoma indicated that knockdown of MX1 in colon cancer cells inhibits migration and invasion of tumour cells [7]. Overexpression of MX1 in BC has been reported previously in certain IHC subtype, highlighting its correlation with immune response and tumour infiltrating lymphocytes, TILs [8] and it has been associated with anthracycline-based chemotherapy response [9].
MX1 responds to type-1 IFN and acts as a mediated signalling pathway [10]. The decrease in MX1 leads to the imperfection of lymphocytes of early and advanced stages of BC which is a consequence of IFN-α signalling in T and B cells [11]. According to Han et al. [11], IFN-α signalling defects in lymphocytes of early and advanced staged BC is associated with a decrease MX1 level. Type-1-IFN influences tumour reduction and development by acting on tumour, immune, or even endothelial cells [9] and can hinder angiogenesis through vascular endothelial growth fact (VEGF) down-regulation [10]. However, the prognostic value of MX1 in BC remains to be defined. The aim of this study is to investigate the expression of MX1 in early-stage (operable) BC and assess its association with clinicopathological parameters and patient outcome as a potential prognostic factor and a possible therapeutic target in BC.
Materials and methods
Study cohorts
A large well-characterised early-stage primary operable invasive BC cohort from female patients attended at Nottingham City Hospital, Nottingham, UK, between 1998 and 2006 was used in this study as described in previous studies [12, 13]. All patients were aged less than or equal to 70 years and were treated as per a uniform protocol. Clinicopathological data were systematically recorded, including patient age, menopausal status, tumour grade, tumour size and histological type. None of the patients in this study was offered neoadjuvant therapy. During the time of the study cohort presentation, patients were treated based on the Nottingham local protocol, which was based on the Nottingham prognostic index (NPI) and ER status as previously published [14]. Briefly, patients with good prognostic NPI scores (≤ 3.4) were not prescribed adjuvant chemotherapy. Patients with higher NPI scores were treated with adjuvant chemotherapy if they have ER-negative tumours. ER-positive patients were treated with hormone therapy.
Hormonal receptor status including oestrogen receptor (ER) and progesterone receptor (PgR) was available and the positive status was defined as those tumours with ≥ 1% immunoreactivity [15, 16]. HER2 and Ki67 status were also available. Ki67 positivity was considered when > 10% of the tumour cells are positive. The assessment of HER2 status was carried out using immunohistochemistry and a chromogenic in situ hybridisation technique to evaluate the gene amplification for the cases with borderline (+ 2). The definition for HER2 positivity was ≥ 10% of tumour cells showing intense staining of their membranous (score + 3) [15, 17, 18]. Based on the immunohistochemistry (IHC) profile, BC molecular subtype data were used, including luminal A, luminal B, HER2+ and triple negative (TN) defined as (Ki67 < 10% (low proliferation); ER+/HER2−), (Ki67 ≥ 10% (high proliferation); ER+/HER2−), (HER2+ irrespective of ER) and (ER−, PgR− and HER2−), respectively [19]. To further understand the molecular interactions of these biomarkers, basal cytokeratin (CK5, CK17 and EGFR), proliferation marker and epithelial mesenchymal transition (EMT)-associated markers, comprising E-cadherin and N-cadherin, were used [20, 21]. Follow-up data were recorded from the date of the primary surgery to the time of death due to BC, which is defined as BC-specific survival (BCSS) and the time from surgery until developing distant metastasis, which is defined as distant-metastasis-free survival (DMFS).
MX1 protein expression
Western blot (WB) for antibody specificity validation
Using WB, the primary antibody, rabbit polyclonal anti-MX1 antibody (ab95926, Abcam, UK), was validated. BC cell line lysate, MCF7, and human embryonic kidney (HEK) that was used as a control (from the American Type Culture Collection, Rockville, MD, USA) were employed for WB antibody specificity validation. MX1 antibody was used at a dilution of 1:1500 and IRDye 800CW Donkey anti-Rabbit fluorescent secondary antibody (LI-COR Biosciences) was used at a 1:15,000 dilution. For loading control, mouse monoclonal anti-β-actin primary antibody (1:5000, Sigma-Aldrich) was used and followed by incubation with anti-Mouse fluorescent secondary antibody (LI-COR Biosciences). To detect the protein molecular weight, 20 µg of the cell lysate was loaded alongside the protein ladder (Page Ruler Plus Prestained Protein Ladder, Thermo Scientific). A specific band was detected at the predicted molecular weight of ~ 64 kDa using Odyssey Fc scanner and visualised by Image Studio 4.0 software (Supplementary Fig. 1).
Immunohistochemistry (IHC)
To assess the pattern of MX1 expression, a representative full-face tissue section for invasive BC (n = 10) for different molecular BC subtypes, histological types and tumour grade were stained to verify the staining homogeneity before the staining of tissue microarray (TMA). Tumour samples were arrayed as previously prepared as TMA utilising a TMA Grand Master® (3DHISTECH®, Budapest, Hungary) [13, 22]. According to the manufacturer’s recommendations, antigen retrieval using citrate buffer pH 6.0 at 1000 W for 20 min with microwave energy was performed. The MX1 protein expression was evaluated by IHC utilising the Novocastra Novolink™ Polymer Detection Systems kit (Leica, Biosystems, UK). Briefly, tissue sections (4 µm) were incubated for 60 min with rabbit polyclonal MX1 (dilution 1:100). A positive control using normal kidney tissue was used, whereas omitting the primary antibody was used as a negative control.
Scoring of MX1 expression
The evaluation of MX1 cytoplasmic expression was performed utilising a modified histochemical score (H-score) for the semi-quantitative analyses of immunoreactivity [23]. To produce a range of values between 0 and 300, the staining intensity [(0 (negative), 1 (weak), 2 (moderate), 3 (strong)] multiplied by the percentage (0–100%) for each intensity of representative cells in the tissue. All non-informative cores were excluded from the scoring including cores with only normal breast tissue or folded tissues during processing and cores contain < 15% tumour cells. To calculate inter-observer concordance, double scoring was blindly performed by AA with (~ 10%) scored by another scorer (IM). Based on BCSS, X-tile bioinformatics software version 3.6.1 (Yale University, USA) was used to generate cut-off points to dichotomise MX1 protein into high and low expression using an H-score of 110.
MX1 transcriptomic analysis
The Molecular Taxonomy of Breast Cancer International Consortium (METABRIC) (n = 1980) was utilised to assess MX1 mRNA expression [24]. Based on the median, a cut-off to dichotomise the levels of mRNA expression into low and high subgroups was employed. The association between MX1 mRNA level, clinicopathological factors and patient outcome was evaluated. Three more publicly available datasets (bc-GenExMiner) version 4.4 (https://bcgenex.centregauducheau.fr) as a prognostic analytical module were also employed in this study to validate the data of METABRIC cohort (n = 1980), namely, DNA microarrays Affymetrix (n = 4904), RNA-Seq TCGA (n = 1034) and RNA-Seq GSE81540 (n = 3678).
Statistical analysis
SPSS® Statistics 24.0 was utilised for the statistical analysis (SPSS, Inc., Chicago, IL, USA). To evaluate the concordance rate between both scorers, the interclass correlation coefficient (ICC) statistical test was performed. The relationship between the targets and the clinicopathological factors was determined using a χ2 test. The correlation between the transcriptome and protein levels was assessed by Spearman’s rank correlation coefficient. For the univariate survival analysis, log-rank test and Kaplan–Meier curves were used. Cox regression model including other prognostic co-variables (tumour grade, nodal stage, tumour size, HER2 status and basal phenotype) was used to detect the independent prognostic value of MX1. For the whole analysis, p-value of < 0.05 was considered significant.
Results
Patterns of MX1 protein expression
Normal breast terminal ductal lobular units displayed a weak MX1 cytoplasmic staining. In the tumour cells, when present, MX1 was expressed in the cytoplasm with no discernible membranous or nuclear staining observed (Fig. 1).
Photomicrographic images (× 40) for immunohistochemical protein expression of MX1 in breast tissue microarray images; MX1 expression of the cytoplasm in cancer cells was distributed as follows; a normal breast terminal duct-lobular, b negative expression in invasive breast carcinoma, and c positive expression in invasive breast carcinoma (high expression is attributed to H-score cut-off point of 110 or more based on X-tile for dichotomisation)
After the exclusion of non-informative TMA cores, the total number of cases suitable for the scoring was 845 out of 2000 cases. A strong concordance was found between both scorers in MX1 scoring (ICC = 0.959, p < 0.0001). A total of 243/845 (28%) of the BC cases showed high expression of MX1 protein.
Significance of MX1 protein expression
High MX1 protein expression was significantly associated with a large tumour size (p = 0.011), high histological grade, poor NPI, hormonal receptor negativity (ER− and PR−) (all p < 0.0001), younger age at diagnosis (p = 0.047) and premenopausal status (p = 0.040, Table 1). Based on St. Gallen International Expert Guidelines and by using the available data in IBC cohorts, high protein expression of MX1 was significantly associated with the triple negative subtype (p < 0.0001, Table 2).
High MX1 level was also associated with basal-like phenotype as defined by the positivity of CK5 (p < 0.0001), CK17 (p = 0.002), EGFR (p = 0.007) and expression of EMT-related marker E-cadherin negativity (p = 0.003). High MX1 level was also associated with the high expression of the proliferation marker Ki67 (p < 0.0001, Table 3).
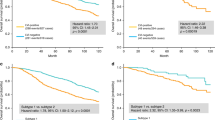
MX1 protein expression and patient outcome
High MX1 protein level showed an association with shorter BCSS (p = 0.006) and DMFS (p = 0.011, Fig. 2a, b). When the cohort was stratified based on adjuvant chemotherapy, high MX1 protein expression was significantly associated with shorter BCSS in patients who did not receive chemotherapy (p = 0.008) but lost its prognostic value in those who were offered such therapy (p = 0.571, Fig. 3a, b). The cohort was then stratified based on MX1 expression (high- versus low expression subgroups) and the association between adjuvant chemotherapy and outcome was tested. This revealed that in the low MX1 subgroup, chemotherapy was associated with shorter BCSS (p = 0.001) whereas in the high MX1 expression subgroup, chemotherapy was not associated with BCSS (p = 0.954, Fig. 3c, d).
Kaplan–Meier survival plot showing the association between the expression of MX1 protein and breast cancer-specific survival in the invasive breast cancer cohort in a patients have not received chemotherapy, b patients received chemotherapy, c chemotherapy vs non-chemotherapy classes in patients with high MX1 and d chemotherapy vs non-chemotherapy classes in patients with low MX1
In multivariate Cox regression analysis, high MX1 protein expression was an independent predictor of shorter BCSS (p = 0.028; HR = 1.5; 95% CI = 1.0–2.2) regardless of tumour grade, nodal stage, tumour size, HER2 status and basal phenotype (Table 4). Multivariate Cox regression analysis was performed when the cohort was stratified based on MX1 expression, in low MX1 protein expression cohort, adjuvant chemotherapy was independent predictor of shorter BCSS (p = 0.017; HR = 0.493; 95% CI = 0.276–0.879) regardless of, tumour grade, nodal stage, tumour size, HER2 status and basal phenotype (Table 5).
MX1 mRNA expression
Based on the spearman’s rank correlation coefficient, a correlation between MX1 protein and MX1 mRNA expression was observed in the Nottingham subset (n = 288) of the METABRIC cohort (r = 0.120, p = 0.042) indicating weak positive correlation.
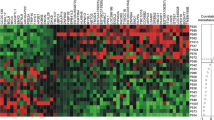
Similar to the protein results, high MX1 mRNA expression was significantly correlated with hormonal status negativity and a high tumour grade (both p < 0.0001), positive axillary lymph node (p = 0.018), basal-like phenotype (p < 0.0001), premenopausal status, younger age (both p = 0.001) and LVI positivity (p = 0.022, Table 6).
In METABRIC, high MX1 mRNA was significantly associated with poor outcome (p < 0.0001, Fig. 2c). Similar results were observed using the bc-GenExMiner version 4.4 for DNA microarray and RNA-Seq cohorts’ analyses. Although no significant difference in the outcome was observed between MX1 high and low expression in TCGA cohort (n = 1034, p = 0.190, Supplementary Fig. 2), a significant difference between the high and low MX1 expressions in correlation with the probability of patients’ survival was recorded in a DNA microarray cohort (Affymetrix) (n = 4904, p = 0.0005, Supplementary Fig. 3) either alone or when combined with METBRIC cohort (n = 10,001, p < 0.0001, Supplementary Fig. 4). Additionally, we have analysed another RNA-Seq cohort, GSE81540 (n = 3678), alone or in combination with TCGA and concluded that high MX1 expression was significantly different from low expression and has poorer prognostic consequences in both situations (p = 0.0020, 0.0086, Supplementary Figs. 5, 6), respectively. All in all, out of four cohorts analysed and, it was only TCGA cohort, when analysed alone, did not show a significant change between the high and low MX1 expression.
Discussion
MX1 contributes to the progression of cancers with different attributions, as noticed in various cancers. Although MX1 protein activity craves for antiviral activities in the immunity system [25, 26], it aids in bringing about a signal that articulates a significant contribution to cancer progression and response to treatments, such as chemotherapy procedures. Moreover, the gene replicates and regulates the gene transcription in which alteration is set to take place within the cancer cells. The progression initiates toward the metastatic processes in which cell proliferation, migration and death by the cancer are sustained or inhibited by MX1 [27].
MX1 has been demonstrated to play a role in various human cancers. It has been speculated that it may be a tumour suppressor for IFN therapy [28]. To evaluate the transcriptomic and protein expression level of MX1 by IHC, we used well-annotated multiple BC cohorts to assess their associations with clinicopathological parameters and patient outcomes. The results showed an association between MX1 expression and the clinicopathological features’ characteristic of aggressive behaviour, which strengthens the putative role of MX1 in tumour progression. The weak correlation between the mRNA and protein expression of MX1 may have resulted from different biological and technical factors. One of these biological factors is the rate of mRNA being translated into proteins which is usually termed ‘translational efficiency’ which has been shown to significantly impact on the correlation between mRNA and protein levels [29]. Another reason might be attributed to the subjectivity of H-score approach in the interpretation of the expression of IHC-staining sections [30] and the fact that the METABRIC cases used whole tissue comprising many different cell types.
A study has revealed that MX1 is a target for repression of SATB1. Genome organiser SATB1 can promote BC tumour growth and can lead to metastasis by reprogramming SATB1 expression [31]. The pro-proliferative PIK3/AKT pathway plays a role in the regulatory cascade-enhancing MX1 expression in response to IFNα. In relapsing patients, the overexpression of MX1 may be a result of the induction of growth signalling by different pathways [32]. In this study, an association between MX1 grade and the proliferation marker Ki67 is identified.
In different types of cancers, ISGs are largely expressed. IFNs play a significant role in various pathways associated with malignancies. A study revealed that in HER2-positive BCs, MX1 is only expressed in the cytoplasm of tumour cells. Moreover, high histological grade and intense infiltrate of TILs are correlated with the expression of MX1 protein. Type I IFNs lead to T-cell exhaustion by the overexpression of tumour programmed cell death ligand 1 (PD-L1) and the increase of PD-L1 level, which can interact with programmed death 1 on T cells [8].
In this study, high MX1 protein was significantly associated with EGFR and the loss of E-cadherin, which can regulate migration, EMT and invasion [33]. Thus, through EMT, which is an important mechanism for metastasis of breast carcinoma cells, MX1 may play an essential role in the regulation of tumour progression [34].
Additionally, high expression of MX1 was associated with the highly proliferative basal phenotype (CK5 and CK17) [35,36,37]. To initiate and establish a metastatic cascade, proliferation and invasion must be occurred to the adjacent tissue by the primary tumour cells. At the same time, the evasion of apoptosis and immune responses occurs with the tumour cells [38]. Thus, in cell proliferation, a prerequisite stage of the metastatic process, MX1 may have a role. Furthermore, the elevated level of these basal cytokeratins (CK5 and CK17) in patients with high MX1 expression confers a poor prognosis. Cytokeratins are strongly associated with aggressive behaviours of the tumours such as high histological grade, hormonal receptor negativity and worse outcome [39, 40]. This further supports our results and implies that MX1 plays a role in tumourigenic pathways.
The results indicate that MX1 is a potential prognostic biomarker in IBC particularly in patients not receiving chemotherapy. Interestingly, our analysis of the overall cohort showed that high MX1 level in patients who were not offered chemotherapy was associated with poor outcome in comparison with those who received chemotherapeutic drugs. Consequently, MX1 prognostic value seems to be invalidated when patients were offered chemotherapy. Whether this phenomenon can be exploited to monitor the chemotherapy effectiveness or not remains ambiguous and required further clinical studies to be approved. The MX1 prognostic value has been validated by the publicly available domains. The results demonstrated that high MX1 expression was correlated with shorter survival in BC patients, in three large datasets out of the four cohorts tested. The correlation between MX1 and outcome was also maintained throughout the follow-up period indicating that the impact of MX1 on the outcome is not time dependent.
Although this study presents interesting findings, some hypothetical limitations were determined. Firstly, it is based on a retrospectively collected cohort. Secondly, the cut-off point used in the protein level analysis was not prespecified and was based on X-tile, which was determined based on the prediction of patient survival and that different cut-off points may result in different categorisation of MX1. Finally, a proper assessment of the expression of MX1 in a well-designed randomised clinical trial where patients are treated in a uniform fashion is recommended.
In conclusion, MX1 plays a role in BC associated with features of aggressive behaviour and is an independent prognostic marker associated with shorter survival. Its prognostic value is influenced by chemotherapy use; however, it is recommended for these results to be verified in a randomised clinical trial setting. Further functional studies in vitro and/or in vivo of the biological role of MX1 in BC cell lines are necessary to investigate its potential use as a therapeutic target in BC.
References
Dawson SJ, Rueda OM, Aparicio S, Caldas C (2013) A new genome-driven integrated classification of breast cancer and its implications. EMBO J 32(5):617–628. https://doi.org/10.1038/emboj.2013.19
Verhelst J, Hulpiau P, Saelens X (2013) Mx proteins: antiviral gatekeepers that restrain the uninvited. Microbiol Mol Biol Rev 77(4):551–566. https://doi.org/10.1128/MMBR.00024-13
Haller O, Kochs G (2002) Interferon-induced mx proteins: dynamin-like GTPases with antiviral activity. Traffic (Cph Den) 3(10):710–717
Boerner JL, Nechiporchik N, Mueller KL, Polin L, Heilbrun L, Boerner SA, Zoratti GL, Stark K, LoRusso PM, Burger A (2015) Protein expression of DNA damage repair proteins dictates response to topoisomerase and PARP inhibitors in triple-negative breast cancer. PLoS ONE 10(3):e0119614. https://doi.org/10.1371/journal.pone.0119614
Borden EC (2015) 53-Interferons. In: Mendelsohn J, Gray JW, Howley PM, Israel MA, Thompson CB (eds) The molecular basis of cancer, 4th edn. Content Repository Only!, Philadelphia, pp 739–752.e737. https://doi.org/10.1016/B978-1-4557-4066-6.00053-6
Calmon MF, Rodrigues RV, Kaneto CM, Moura RP, Silva SD, Mota LD, Pinheiro DG, Torres C, de Carvalho AF, Cury PM, Nunes FD, Nishimoto IN, Soares FA, da Silva AM, Kowalski LP, Brentani H, Zanelli CF, Silva WA Jr, Rahal P, Tajara EH, Carraro DM, Camargo AA, Valentini SR (2009) Epigenetic silencing of CRABP2 and MX1 in head and neck tumors. Neoplasia (New York, NY) 11(12):1329–1339
Croner RS, Sturzl M, Rau TT, Metodieva G, Geppert CI, Naschberger E, Lausen B, Metodiev MV (2014) Quantitative proteome profiling of lymph node-positive vs. -negative colorectal carcinomas pinpoints MX1 as a marker for lymph node metastasis. Int J Cancer 135(12):2878–2886. https://doi.org/10.1002/ijc.28929
Lee SJ, Hwang CS, Kim YK, Lee HJ, Ahn SJ, Shin N, Lee JH, Shin DH, Choi KU, Park DY, Lee CH, Huh GY, Sol MY, Lee HJ, Gong G, Kim JY, Kim A (2017) Expression of myxovirus resistance A (MxA) is associated with tumor-infiltrating lymphocytes in human epidermal growth factor receptor 2 (HER2)-positive breast cancers. Cancer Res Treat Off J Korean Cancer Assoc 49(2):313–321. https://doi.org/10.4143/crt.2016.098
Sistigu A, Yamazaki T, Vacchelli E, Chaba K, Enot DP, Adam J, Vitale I, Goubar A, Baracco EE, Remédios C, Fend L, Hannani D, Aymeric L, Ma Y, Niso-Santano M, Kepp O, Schultze JL, Tüting T, Belardelli F, Bracci L, La Sorsa V, Ziccheddu G, Sestili P, Urbani F, Delorenzi M, Lacroix-Triki M, Quidville V, Conforti R, Spano J-P, Pusztai L, Poirier-Colame V, Delaloge S, Penault-Llorca F, Ladoire S, Arnould L, Cyrta J, Dessoliers M-C, Eggermont A, Bianchi ME, Pittet M, Engblom C, Pfirschke C, Préville X, Uzè G, Schreiber RD, Chow MT, Smyth MJ, Proietti E, André F, Kroemer G, Zitvogel L (2014) Cancer cell-autonomous contribution of type I interferon signaling to the efficacy of chemotherapy. Nat Med 20(11):1301–1309. https://doi.org/10.1038/nm.3708
Zitvogel L, Galluzzi L, Kepp O, Smyth MJ, Kroemer G (2015) Type I interferons in anticancer immunity. Nat Rev Immunol 15(7):405–414. https://doi.org/10.1038/nri3845
Han Y-Y, Liu H-Y, Han D-J, Zong X-C, Zhang S-Q, Chen Y-Q (2013) Role of glycosylation in the anticancer activity of antibacterial peptides against breast cancer cells. Biochem Pharmacol 86(9):1254–1262. https://doi.org/10.1016/j.bcp.2013.08.008
Miligy IM, Gorringe KL, Toss MS, Al-Kawaz AA, Simpson P, Diez-Rodriguez M, Nolan CC, Ellis IO, Green AR, Rakha EA (2018) Thioredoxin-interacting protein is an independent risk stratifier for breast ductal carcinoma in situ. Mod Pathol Off J US Can Acad Pathol 31(12):1807–1815. https://doi.org/10.1038/s41379-018-0086-7
Sonbul SN, Aleskandarany MA, Kurozumi S, Joseph C, Toss MS, Diez-Rodriguez M, Nolan CC, Mukherjee A, Martin S, Caldas C, Ellis IO, Green AR, Rakha EA (2018) Saccharomyces cerevisiae-like 1 (SEC14L1) is a prognostic factor in breast cancer associated with lymphovascular invasion. Mod Pathol Off J US Can Acad Pathol 31(11):1675–1682. https://doi.org/10.1038/s41379-018-0092-9
Rakha EA, El-Sayed ME, Lee AH, Elston CW, Grainge MJ, Hodi Z, Blamey RW, Ellis IO (2008) Prognostic significance of Nottingham histologic grade in invasive breast carcinoma. J Clin Oncol Off J Am Soc Clin Oncol 26(19):3153–3158. https://doi.org/10.1200/jco.2007.15.5986
Rakha EA, Pinder SE, Bartlett JMS, Ibrahim M, Starczynski J, Carder PJ, Provenzano E, Hanby A, Hales S, Lee AHS, Ellis IO, National Coordinating Committee for Breast Pathology (2015) Updated UK Recommendations for HER2 assessment in breast cancer. J Clin Pathol 68(2):93–99. https://doi.org/10.1136/jclinpath-2014-202571
Rakha EA, Agarwal D, Green AR, Ashankyty I, Ellis IO, Ball G, Alaskandarany MA (2017) Prognostic stratification of oestrogen receptor-positive HER2-negative lymph node-negative class of breast cancer. Histopathology 70(4):622–631. https://doi.org/10.1111/his.13108
Green AR, Aleskandarany MA, Agarwal D, Elsheikh S, Nolan CC, Diez-Rodriguez M, Macmillan RD, Ball GR, Caldas C, Madhusudan S, Ellis IO, Rakha EA (2016) MYC functions are specific in biological subtypes of breast cancer and confers resistance to endocrine therapy in luminal tumours. Br J Cancer 114(8):917–928. https://doi.org/10.1038/bjc.2016.46
Hammond MEH, Hayes DF, Dowsett M, Allred DC, Hagerty KL, Badve S, Fitzgibbons PL, Francis G, Goldstein NS, Hayes M, Hicks DG, Lester S, Love R, Mangu PB, McShane L, Miller K, Osborne CK, Paik S, Perlmutter J, Rhodes A, Sasano H, Schwartz JN, Sweep FCG, Taube S, Torlakovic EE, Valenstein P, Viale G, Visscher D, Wheeler T, Williams RB, Wittliff JL, Wolff AC (2010) American Society of Clinical Oncology/College of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. Arch Pathol Lab Med 134(6):907–922. https://doi.org/10.1043/1543-2165-134.6.907
Aljohani AI, Toss MS, Kurozumi S, Joseph C, Aleskandarany MA, Miligy IM, Ansari RE, Mongan NP, Ellis IO, Green AR, Rakha EA (2019) The prognostic significance of wild-type isocitrate dehydrogenase 2 (IDH2) in breast cancer. Breast Cancer Res Treat. https://doi.org/10.1007/s10549-019-05459-7
Abd El-Rehim DM, Ball G, Pinder SE, Rakha E, Paish C, Robertson JFR, Macmillan D, Blamey RW, Ellis IO (2005) High-throughput protein expression analysis using tissue microarray technology of a large well-characterised series identifies biologically distinct classes of breast cancer confirming recent cDNA expression analyses. Int J Cancer 116(3):340–350. https://doi.org/10.1002/ijc.21004
Rakha EA, Elsheikh SE, Aleskandarany MA, Habashi HO, Green AR, Powe DG, El-Sayed ME, Benhasouna A, Brunet J-S, Akslen LA, Evans AJ, Blamey R, Reis-Filho JS, Foulkes WD, Ellis IO (2009) Triple-negative breast cancer: distinguishing between basal and nonbasal subtypes. Clin Cancer Res 15(7):2302. https://doi.org/10.1158/1078-0432.CCR-08-2132
El Ansari R, Craze ML, Miligy I, Diez-Rodriguez M, Nolan CC, Ellis IO, Rakha EA, Green AR (2018) The amino acid transporter SLC7A5 confers a poor prognosis in the highly proliferative breast cancer subtypes and is a key therapeutic target in luminal B tumours. Breast Cancer Res 20(1):21. https://doi.org/10.1186/s13058-018-0946-6
McCarty KS Jr, McCarty KS Sr (1984) Histochemical approaches to steroid receptor analyses. Semin Diagn Pathol 1(4):297–308
Curtis C, Shah SP, Chin SF, Turashvili G, Rueda OM, Dunning MJ, Speed D, Lynch AG, Samarajiwa S, Yuan Y, Graf S, Ha G, Haffari G, Bashashati A, Russell R, McKinney S, Langerod A, Green A, Provenzano E, Wishart G, Pinder S, Watson P, Markowetz F, Murphy L, Ellis I, Purushotham A, Borresen-Dale AL, Brenton JD, Tavare S, Caldas C, Aparicio S (2012) The genomic and transcriptomic architecture of 2,000 breast tumours reveals novel subgroups. Nature 486(7403):346–352. https://doi.org/10.1038/nature10983
Jiang C-Y, Gao Y, Wang X-J, Ruan Y, Bei X-Y, Wang X-H, Jing Y-F, Zhao W, Jiang Q, Li J, Han B-M, Xia S-J, Zhao F-J (2016) Long non-coding RNA lnc-MX1-1 is associated with poor clinical features and promotes cellular proliferation and invasiveness in prostate cancer. Biochem Biophys Res Commun 470(3):721–727. https://doi.org/10.1016/j.bbrc.2016.01.056
Hu J-L, Hua Y-J, Chen Y, Yu B, Gao S (2015) Structural analysis of tumor-related single amino acid mutations in human MxA protein. Chin J Cancer 34(12):583–593. https://doi.org/10.1186/s40880-015-0055-1
Brown SG, Knowell AE, Hunt A, Patel D, Bhosle S, Chaudhary J (2015) Interferon inducible antiviral MxA is inversely associated with prostate cancer and regulates cell cycle, invasion and Docetaxel induced apoptosis. Prostate 75(3):266–279. https://doi.org/10.1002/pros.22912
Donnelly LA, Donnelly CR, Xie Y, Bellile EL, Wolf GT, Lei Y (2017) An expanded cohort analysis of the prognostic value of the Type I interferon signature Gene MX1 in head and neck squamous cell carcinoma. J Oral Maxillofac Surg 75(10):e395–e396. https://doi.org/10.1016/j.joms.2017.07.121
Maier T, Güell M, Serrano L (2009) Correlation of mRNA and protein in complex biological samples. FEBS Lett 583(24):3966–3973. https://doi.org/10.1016/j.febslet.2009.10.036
Rizzardi AE, Johnson AT, Vogel RI, Pambuccian SE, Henriksen J, Skubitz AP, Metzger GJ, Schmechel SC (2012) Quantitative comparison of immunohistochemical staining measured by digital image analysis versus pathologist visual scoring. Diagn Pathol 7:42–42. https://doi.org/10.1186/1746-1596-7-42
Mushinski JF, Nguyen P, Stevens LM, Khanna C, Lee S, Chung EJ, Lee MJ, Kim YS, Linehan WM, Horisberger MA, Trepel JB (2009) Inhibition of tumor cell motility by the interferon-inducible GTPase MxA. J Biol Chem 284(22):15206–15214. https://doi.org/10.1074/jbc.M806324200
Johansson HJ, Sanchez BC, Forshed J, Stal O, Fohlin H, Lewensohn R, Hall P, Bergh J, Lehtio J, Linderholm BK (2015) Proteomics profiling identify CAPS as a potential predictive marker of tamoxifen resistance in estrogen receptor positive breast cancer. Clin Proteomics 12(1):8. https://doi.org/10.1186/s12014-015-9080-y
Masuda H, Zhang D, Bartholomeusz C, Doihara H, Hortobagyi GN, Ueno NT (2012) Role of epidermal growth factor receptor in breast cancer. Breast Cancer Res Treat 136(2):331–345. https://doi.org/10.1007/s10549-012-2289-9
Heerboth S, Housman G, Leary M, Longacre M, Byler S, Lapinska K, Willbanks A, Sarkar S (2015) EMT and tumor metastasis. Clin Transl Med 4(1):6. https://doi.org/10.1186/s40169-015-0048-3
Laakso M, Loman N, Borg Å, Isola J (2005) Cytokeratin 5/14-positive breast cancer: true basal phenotype confined to BRCA1 tumors. Mod Pathol 18(10):1321–1328. https://doi.org/10.1038/modpathol.3800456
Badve S, Dabbs DJ, Schnitt SJ, Baehner FL, Decker T, Eusebi V, Fox SB, Ichihara S, Jacquemier J, Lakhani SR, Palacios J, Rakha EA, Richardson AL, Schmitt FC, Tan P-H, Tse GM, Weigelt B, Ellis IO, Reis-Filho JS (2010) Basal-like and triple-negative breast cancers: a critical review with an emphasis on the implications for pathologists and oncologists. Mod Pathol 24:157. https://doi.org/10.1038/modpathol.2010.200
Inwald EC, Klinkhammer-Schalke M, Hofstädter F, Zeman F, Koller M, Gerstenhauer M, Ortmann O (2013) Ki-67 is a prognostic parameter in breast cancer patients: results of a large population-based cohort of a cancer registry. Breast Cancer Res Treat 139(2):539–552. https://doi.org/10.1007/s10549-013-2560-8
Hunter KW, Crawford NPS, Alsarraj J (2008) Mechanisms of metastasis. Breast Cancer Res 10(Suppl 1):S2. https://doi.org/10.1186/bcr1988
Alshareeda AT, Soria D, Garibaldi JM, Rakha E, Nolan C, Ellis IO, Green AR (2013) Characteristics of basal cytokeratin expression in breast cancer. Breast Cancer Res Treat 139(1):23–37. https://doi.org/10.1007/s10549-013-2518-x
Kordek R, Potemski P, Kusinska R, Pluciennik E, Bednarek A (2010) Basal keratin expression in breast cancer by quantification of mRNA and by immunohistochemistry. J Exp Clin Cancer Res 29:39. https://doi.org/10.1186/1756-9966-29-39
Acknowledgements
Abrar Aljohani is supported and funded by Taif University, Kingdom of Saudi Arabia. The authors are part of the PathLAKE Digital Pathology Consortium. These new Centres are supported by a £50m investment from the Data to Early Diagnosis and Precision Medicine Strand of the Government’s Industrial Strategy Challenge Fund, managed and delivered by UK Research and Innovation (UKRI).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
All authors declare that they have no conflicts of interest.
Research involving human participants and/or animals
This article does not contain any studies with human participants or animals performed by any of the authors. This work obtained ethics approval to use the human tissue samples by the North West: Greater Manchester Central Research Ethics Committee under the title; Nottingham Health Science Biobank (NHSB), Reference Number 15/NW/0685.
Informed consent
Informed consent was obtained from all individuals prior to surgery to use their tissue materials in research. This study was performed according to the REMARK guidelines for tumour prognostic studies
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Aljohani, A.I., Joseph, C., Kurozumi, S. et al. Myxovirus resistance 1 (MX1) is an independent predictor of poor outcome in invasive breast cancer. Breast Cancer Res Treat 181, 541–551 (2020). https://doi.org/10.1007/s10549-020-05646-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-020-05646-x