Abstract
Objective
The purpose of the study was to determine the angiogenic capacity of sera in early and late pregnancy and in umbilical blood serum after childbirth, and to define how angiogenic properties assessed in a functional in vitro test are related to individual angiogenic proteins in six women with pre-eclampsia and in six healthy pregnant controls.
Methods
Maternal first and third trimester serum samples, and umbilical blood samples after childbirth, were tested in an in vitro human adipose stromal cell—human umbilical vein endothelial cell (hASC-HUVEC) vasculogenesis/angiogenesis assay. The angiogenic properties of the samples were measured by quantifying tubule formation. Concentrations of total placental growth factor (PlGF), total vascular endothelial growth factor (VEGF), soluble fms-like tyrosine kinase 1 (sFlt-1) and soluble endoglin (sEng) were determined by immunoassay.
Results
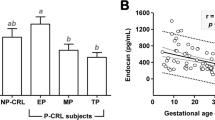
First-trimester maternal sera of both groups had a stimulatory effect on angiogenesis in vitro and levels of angiogenic proteins did not differ between the groups. Third-trimester maternal sera in the pre-eclampsia group had an inhibitory effect on tubule formation, while those from normal pregnancies remained stimulatory. Compared with the first trimester there was a significant change in the concentrations of angiogenic proteins toward an anti-angiogenic state in pre-eclampsia. Umbilical blood serum exhibited strong anti-angiogenic effects without a significant difference between groups.
Conclusions
Third-trimester serum of pre-eclamptic patients is anti-angiogenic. This phenomenon is not yet present in the first trimester. Umbilical blood serum shows inhibitory effects on angiogenesis after normal as well as pre-eclamptic pregnancy.



Similar content being viewed by others
References
Maynard S, Karumanchi A (2011) Angiogenic factors and preeclampsia. Semin Nephrol 31:33–46
McElrath T, Lim KH, Pare E, Rich-Edwards J, Pucci D, Troisi R, Parry S (2012) Longitudinal evaluation of predictive value for preeclampsia of circulating angiogenic factors through pregnancy. Am J Obstet Gynecol 207:407.e1–407.e7
Rana S, Karumanchi SA, Lindheimer MD (2014) Angiogenic factors in diagnosis, management, and research in preeclampsia. Hypertension 63:198–202
Levine R, Maynard S, Qian C, Lim K-H, England L, Yu KF, Schisterman EF, Thadhani R, Sachs B, Epstein F, Sibai B, Sukhatme V, Karumanchi S (2004) Circulating angiogenic factors and the risk of preeclampsia. N Engl J Med 350:672–683
Schaarschmidt W, Rana S (2013) The course of angiogenic factors in early- vs. late-onset preeclampsia and HELLP syndrome. J Perinat Med 41:511–516
Staff AC, Braekke K, Kittelsen N, Lyberg T, Holthe M (2005) Circulating concentrations of sFlt1 (soluble fms-like tyrosine kinase 1) in fetal and maternal serum during pre-eclampsia. Eur J Obstet Gynecol Reprod Biol 122:33–39
Blanco MV, Vega HR, Giuliano R, Grana DR, Azzato F, Lerman J, Milei J (2011) Histomorphometry of umbilical cord blood vessels in preeclampsia. J Clin Hypertens 13:30–34
Toimela T, Huttala O, Sabell E, Mannerström M, Sarkanen JR, Ylikomi T, Heinonen T (2017) Intra-laboratory validated human cell-based in vitro vasculogenesis/angiogenesis test with serum-free medium. Reprod Toxicol 70:116–125
Sarkanen JR, Mannerström M, Vuorenpää H, Uotila J, Ylikomi T, Heinonen T (2011) Intra-laboratory pre-validation of a human cell based in vitro angiogenesis assay for testing angiogenesis modulators. Front Pharmacol 1:147
Virtanen A, Toimela T, Tihtonen K, Sarkanen JR, Huttala O, Heinonen T, Uotila J (2016) Strong inhibitory effect of pre-eclampsia serum on angiogenesis detected in vitro by human cell-based angiogenesis tests. Pregnancy Hypertens 6:367–373
Huttala O, Vuorenpaa H, Toimela T, Uotila J, Kuokkanen H, Ylikomi T, Sarkanen JR, Heinonen T (2015) Human vascular model with defined stimulation medium—a characterization study. ALTEX 32:125–136
Brown MA, Lindheimer MD, de Swiet M, Van Assche A, Moutquin JM (2001) The classification and diagnosis of the hypertension disorders of pregnancy: statement from the International Society for the Study of Hypertension in Preganancy (ISSHP). Hypertens Pregnancy 20:IX–XIV
Sibai B, Dekker G, Kupferminc M (2005) Pre-eclampsia. Lancet 365:785–799
Turner J (2010) Diagnosis and management of pre-eclampsia: an update. Int J Womens Health 2:327–337
Sankilampi U, Hannila M-L, Saari A, Gissler M, Dunkel L (2013) New population-based references for birth weight, length, and head circumference in singletons and twins from 23 to 43 gestation weeks. Ann Med 45:446–454
Sarkanen JR, Vuorenpää H, Huttala O, Mannerström B, Kuokkanen H, Miettinen S, Heinonen T, Ylikomi T (2012) Adipose stromal cell tubule network model provides a versatile tool for vascular research and tissue engineering. Cells Tissues Organs 196:385–397
Chaiworapongsa T, Chaemsaithong P, Yeo L, Romero R (2014) Pre-eclampsia part 1: current understanding of its pathophysiology. Nat Rev Nephrol 10:466–480
Kaufmann P, Mayhew TM, Charnock-Jones DS (2004) Aspects of human fetoplacental vasculogenesis and angiogenesis. II. Changes during normal pregnancy. Placenta 25:114–126
Maynard S, Min J, Merchan J, Lim K, Li J, Mondal S, Libermann T, Morgan J, Sellke F, Stillman I, Epstein F, Sukhatme V, Karumanchi S (2003) Excess placental soluble fms-like tyrosine kinase 1 (sFlt1) may contribute to endothelial dysfunction, hypertension, and proteinuria in preeclampsia. J Clin Invest 111:649–658
Kleinrouweler CE, Wiegerinck MM, Ris-Stalpers C, Bossuyt PM, van der Post JA, von Dadelszen P, Mol BW, Pajkrt E, EBM CONNECT Collaboration (2012) Accuracy of circulating placental growth factor, vascular endothelial growth factor, soluble fms-like tyrosine kinase 1 and soluble endoglin in the prediction of pre-eclampsia: a systematic review and meta-analysis. BJOG 119:778–787
Kusanovic J, Romero R, Chaiworapongsa T, Erez O, Mittal P, Vaisbuch E, Mazaki-Tovi S, Gotsch F, Edwin S, Gomez R, Yeo L, Conde-Agudelo A, Hassan S (2009) A prospective cohort study of the value of maternal plasma concentrations of angiogenic and anti-angiogenic factors in early pregnancy and midtrimester in the identification of patients destined to develop preeclampsia. J Matern Fetal Neonatal Med 22:1021–1038
Akolekar R, de Cruz J, Foidart JM, Munaut C, Nicolaides KH (2010) Maternal plasma soluble fms-like tyrosine kinase-1 and free vascular endothelial growth factor at 11 to 13 weeks of gestation in preeclampsia. Prenat Diagn 30:191–197
Erez O, Romero R, Espinoza J, Fu W, Todem D, Kusanovic JP, Gotsch F, Edwin S, Nien JK, Chaiworapongsa T, Mittal P, Mazaki-Tovi S, Than NG, Gomez R, Hassan SS (2008) The change in concentrations of angiogenic and anti-angiogenic factors in maternal plasma between the first and second trimesters in risk assessment for the subsequent development of preeclampsia and small-for-gestational age. J Matern Fetal Neonatal Med 21:279–287
Spurway J, Logan P, Pak S (2012) The development, structure and blood flow within the umbilical cord with particular reference to the venous system. Australas J Ultrasound Med 15:97–102
Sezer SD, Küçük M, Yenisey C, Yüksel H, Odabaşı AR, Türkmen MK, Çetinkaya Çakmak B, Ömürlü IK (2012) Comparison of angiogenic and anti-angiogenic factors in maternal and umbilical cord blood in early- and late-onset pre-eclampsia. Gynecol Endocrinol 28:628–632
Paredes V, Espinoza-Caicedo J, Salazar-Pousada D, Escobar G, Perez-Lopez F, Chedraui P (2017) Lower placental growth factor and higher free β-hCG and PAPP-A levels in the circulation of near-term pregnancies complicated with severe preeclampsia. J Gynecol Endocrinol 33:79–81
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Virtanen, A., Huttala, O., Tihtonen, K. et al. Angiogenic capacity in pre-eclampsia and uncomplicated pregnancy estimated by assay of angiogenic proteins and an in vitro vasculogenesis/angiogenesis test. Angiogenesis 22, 67–74 (2019). https://doi.org/10.1007/s10456-018-9637-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10456-018-9637-2