Abstract
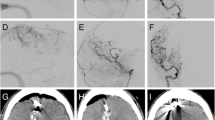
One of the most life-threatening complications after the obliteration of intracranial arteriovenous malformations is the development of oedema and/or multifocal haemorrhage. Two main theories have been postulated so far in order to explain this situation. On one hand, “normal perfusion pressure breakthrough phenomenon” is based on the loss of cerebral vessel autoregulation due to the chronic vasodilation of perinidal microcirculation. On the other hand, the “occlusive hyperaemia” deals with thrombotic and venous obstruction phenomena that may also generate such manifestations. The aim of this study is to resume the main concepts of the “normal perfusion pressure breakthrough phenomenon” theory as well as the related animal models described up to date, their advantages and disadvantages, and the main conclusions obtained as a result of the experimental research.



Similar content being viewed by others
References
Al-Rodhan NRF, Sundt TM Jr, Piepgras DG, Nichols DA, Rüfenacht D, Stevens LN (1993) Occlusive hyperemia: a theory for the hemodynamic complications following resection of intracerebral arteriovenous malformations. J Neurosurg 78:167–175
Attia W, Tada T, Hongo K, Nagashima H, Takemae T, Tanaka Y et al (2003) Microvascular pathological features of immediate perinidal parenchyma in cerebral arteriovenous malformations: giant bed capillaries. J Neurosurg 98:823–827
Batjer HH, Devous MD Sr, Meyer YJ, Purdy PD, Samson DS (1988) Cerebrovascular hemodynamics in arteriovenous malformation complicated by normal perfusion pressure breakthrough. Neurosurgery 22:503–509
Bederson JB, Wiestler OD, Bruestle O, Roth P, Frick R, Yasargil MG (1991) Intracranial venous hypertension and the effects of venous outflow obstruction in a rat model of arteriovenous fistula. Neurosurgery 29:341–350
Carvi y Nievas MN (2005) Experimental cerebral arteriovenous fistulas. Neurol Res 27:857–863
Chyatte D (1997) Normal pressure perfusion breakthrough after resection of arteriovenous malformation. J Stroke Cerebrovasc Dis 6:130–136
Constantino A, Vinters HV (1986) A pathogenic correlate of the “steal” phenomenon in a patient with cerebral arteriovenous malformation. Stroke 17:103–106
De Salles AA, Manchola I (1994) CO2 reactivity in arteriovenous malformations of the brain: a transcranial Doppler ultrasound study. J Neurosurg 80:624–630
De Salles AAF, Solberg TD, Mischel P, Maasoud TF, Plasencia A, Goetsch S (1996) Arterivenous malformation animal model for radiosurgery: the rete mirabile. AJNR Am J Neuroradiol 17:1451–1458
Folkow B, Sivertsson R (1968) Adaptive changes in “reactivity” and wall/lumen ratio in cat blood vessels exposed to prolonged transmural pressure difference. Life Sci 7:1283–1289
Folkow B, Gurevich M, Hallbäck Y, Lundgren Y, Weiss L (1971) The hemodynamic consequences of regional hypotension in spontaneously hypertensive and normotensive rats. Acta Physiol Scand 83:532–541
Fry DL (1968) Acute vascular endothelial changes associated with increased blood velocity gradients. Circ Res 22:165–197
Gao P, Zhu Y, Ling F, Shen F, Lee B, Gabriel RA et al (2009) Nonischemic cerebral venous hypertension promotes a proangiogenic stage via HIF-1 downstream genes and leukocyte-derived MMP-9. J Cerebr Blood Flow Metab 29:1482–1490
Gurdjian ES, Webser JE, Martin FA (1950) Carotid internal jugular anastomosis in the Rhesus monkey. J Neurosurg 7:467–472
Hai J, Ding M, Guo Z, Wang B (2002) A new rat model of chronic cerebral hypoperfusion associated with arteriovenous malformations. J Neurosurg 97:1198–1202
Hai J, Li ST, Lin Q, Pan QG, Gao F, Ding MX (2003) Vascular endothelial growth factor expression and angiogenesis induced by chronic cerebral hypoperfusion in the rat brain. Neurosurgery 53:963–970
Hai J, Lin Q, Li ST, Pan QG (2004) Chronic cerebral hypoperfusion and reperfusion injury of restoration of normal perfusion pressure contributes to the neuropathological changes in rat brain. Brain Res Mol Brain Res 126:137–145
Homan RW, Devous MD Sr, Stokely EM, Bonte FJ (1986) Quantification of intracerebral steal in patients with arteriovenous malformation. Arch Neurol 43:779–785
Irikura K, Morii S, Miyasaka Y, Ymada M, Tokiwa K, Yda K (1996) Impaired autoregulation in an experimental model of chronic cerebral hypoperfusion in rats. Stroke 27:1399–1404
Kader A, Young WL (1996) The effects of intracranial arteriovenous malformations on cerebral hemodynamics. Neurosurg Clin N Am 7:767–781
Klisch J, Requejo F, Yin L, Eissner B, Schumacher M (2001) The two-in-one model: a new variation of the arteriovenous malformation model in swine. Neuroradiology 43:393–397
Kojima T, Miyachi S, Sahara Y, Nakai K, Okamoto T, Hattori K et al (2007) The relationship between venous hypertension and expression of vascular endothelial growth factor: hemodynamic and immunohistochemical examinations in a rat venous hypertension model. Surg Neurol 68:277–284
Kulik T, Kusano Y, Aronhime S, Snadler AL, Winn HR (2008) Regulation of cerebral vasculature in normal and ischemic brain. Neuropharmacology 55:281–288
Lylyk P, Viñuela F, Vinters VH, Dion J, Bentson J, Duckwiler G et al (1990) Use of a new mixture for embolization of intracranial vascular malformations: preliminary experimental experience. Neuroradiology 32:304–310
Massoud TF, Ji C, Viñuela F, Guglielmi G, Robert J, Duckwiler GR et al (1994) An experimental arteriovenous malformation model in swine: anatomic basis and construction technique. AJNR Am J Neuroradiol 15:1537–1545
Massoud TF, Ji C, Vinuela F, Turjman F, Guglielmi G, Duckwiler GR et al (1996) Laboratory simulations and training in endovascular embolotherapy with a swine arteriovenous malformation model. AJNR Am J Neuroradiol 17:271–279
Massoud TF (2000) Experimental arteriovenous malformations modelling in laboratory sheep versus swine. AJNR Am J Neuroradiol 21:985–990
Miyasaka Y, Tokiwa K, Irikura K, Kurata A, Tanaka R, Morii S et al (1994) The effects of a carotid-jugular fistula on cerebral blood flow in the cat: an experimental study in the acute period. Surg Neurol 41:396–398
Morgan MK, Johnston I, Besser M, Baines D (1987) Cerebral arteriovenous malformations, steal, and the hypertensive breakthrough threshold. An experimental study in rats. J Neurosurg 66:563–567
Morgan MK, Anderson RE, Sundt TM (1989) A model of the pathophysiology of cerebral arteriovenous malformations by a carotid jugular fistula in the rat. Brain Res 496:241–250
Muruyama Y, Massoud RF, Vinuela F (1998) Hemodynamic changes in arterial feeders and draining veins during embolotherapy of arteriovenous malformations: an experimental study in a swine model. Neurosurgery 43:96–104
Muruyama Y, Vinuela F, Ulhoa A, Akiba Y, Duckwiler GR, Gobin YP et al (1998) Nonadhesive liquid embolic agent for cerebral arteriovenous malformations: preliminary histopathological studies in swine rete mirabile. Neurosurgery 43:1164–1175
Nornes H, Grip A (1980) Hemodynamic aspects of cerebral arteriovenous malformations. J Neurosurg 53:456–464
Qian Z, Climent S, Maynar M, Usón-Garallo J, Lima-Rodrigues MA, Calles C et al (1999) A simplified arteriovenous malformation model in sheep: feasibility study. AJNR Am J Neuroradiol 20:765–770
Pennings FA, Ince C, Bouma GJ (2006) Continuous real-time visualization of the human cerebral microcirculation during arteriovenous malformation surgery using orthogonal polarization spectral imaging. Neurosurgery 59:167–171
Pietilä TA, Zabramski JM, Thèllier-Janko A, Duveneck K, Bichard WD, Brock M et al (2000) Animal model for cerebral arteriovenous malformation. Acta Neurochir (Wien) 142:1231–1240
Sakaki T, Tsujimoto S, Nishitani M, Ishida Y, Morimoto T (1992) Perfusion pressure breakthrough threshold of cerebral autoregulation in the chronically ischemic brain: an experimental study in cats. J Neurosurg 76:478–485
Schumacher M, Schellhammer F (1999) Experimental pseudo arteriovenous malformation—a model for training and research. Intervent Neuroradiol 5:213–217
Scott BB, McGillicuddy JE, Seeger JF, Kindt GW, Giannotta SL (1978) Vascular dynamics of an experimental cerebral arteriovenous shunt in the primate. Surg Neurol 10:34–38
Sekhon LHS, Morgan MK, Spence I, Weber NC (1997) Chronic cerebral hypoperfusion: pathological and behavioural consequences. Neurosurgery 40:548–556
Sekhon LH, Morgan MK, Spence I (1997) Normal perfusion pressure breakthrough: the role of capillaries. J Neurosurg 86:519–524
Siekmann R, Wakhloo AK, Lieber BB, Gounis MJ, Divani AA, Hopkins LN (2000) Modification of a previously described arteriovenous malformation model in the swine: endovascular and combined surgical/endovascular construction and hemodynamics. AJNR Am J Neuroradiol 21:1722–1725
Spetzler RF, Wilson CB, Weinstein P, Mehdorn M, Townsend J, Telles D (1978) Normal perfusion pressure breakthrough theory. Clin Neurosurg 25:651–672
Tokiwa K, Myasaka Y, Irijura K, Tanaka R, Yamada M (1995) The effects of a carotid-jugular fistula on cerebral blood flow in the cat: an experimental study in the chronic period. Neurol Res 17:297–300
Wade JPH, Hachinski VC (1987) Cerebral steal: robbery or maldistribution? In: Wood JH (ed) Cerebral blood flow: physiologic and clinical aspects. McGraw-Hill Book Co, New York, pp 467–480
Yassari R, Sayama T, Jahromi BS, Aihara Y, Stoodley M, Macdonald RL (2004) Angiographic, hemodynamic and histological characterization of an arteriovenous fistula in rats. Acta Neurochir (Wien) 146:495–504
Young WL, Solomon RA, Prohovnik I, Ornstein E, Weinstein J, Stein BM (1988) 133Xe blood flow monitoring during arteriovenous malformation resection: a case of intraoperative hyperperfusion with subsequent brain swelling. Neurosurgery 22:765–769
Young WL, Kader A, Prohovnik I, Ornstein E, Fleischer LH, Ostapkovich N et al (1993) Pressure autoregulation is intact after arteriovenous malformation resection. Neurosurgery 32:491–496
Young WL, Pile-Spellman J, Prohovnik I, Kader A, Stein BM (1994) Evidence for adaptative autoregulatory displacement in hypotensive cortical territories adjacent to arteriovenous malformations. Columbia University AVM Study Project. Neurosurgery 34:601–611
Acknowledgments
The authors thank Cristina Ruiz Quevedo for assistance in the translation of the manuscript.
Sources of funding
None.
Disclosures
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
K.-P. Sein and I. Erol Sandalcioglu, Hannover, Germany
The treatment of cerebral arteriovenous malformations (AVM) remains challenging, not only in terms of determining the right treatment indication and treatment strategy. Once obliteration of the nidus is achieved, the knowledge and understanding of hemodynamic changes is of utmost importance to guide the patient after treatment through this period in order to prevent haemorrhage. Since the normal perfusion pressure breakthrough theory was introduced in 1978, numerous experimental and animal models have been suggested. Gutierrez-Gonzalez and coworkers nicely summarized the pathophysiological concepts and different animal models and their major results. As the authors also point out the limitations of the listed studies, the need of valuable models for future investigations becomes evident.
Peter Nakaji, Phoenix, USA
The original paper proposing the theory of normal perfusion pressure breakthrough (NPPB) with arteriovenous malformations is now four decades old. Since that time, much debate has been had on the subject, though for many it has become an accepted, if uncommon, phenomenon. More frequently, postoperative haemorrhage has been attributed to incomplete closure of fragile AVM feeding vessels, and edema and brain swelling have been felt to be due to loss of normal venous drainage in the course of AVM resection. In this review by Dr. Raquel Gutierrez-Gonzalez et al., the authors describe and examine the experimental models for studying NPPB.
The questions that a cerebrovascular neurosurgeon has about NPPB revolve around predicting who might have a state of chronic steal-induced vasodilation and thus be at risk, and what to do about it, preferably before haemorrhage and swelling occur. For example, one strategy I routinely employ in my practice at the Barrow Neurological Institute is to induce relative mild hypotension on an empiric basis on my post-resection AVM patients (e.g. target SBP first 24 h 100 mmHg, then 120 mmHg for 24 h, then 140 mmHg for 24 h, followed by ‘normal’ blood pressure for that patient). However, this practice is not actually tailored to the individual patient, about whose regional haemodynamics we know little.
So how can the experimental models clarify things further? Animal models often have anatomy very different from a human and are largely based on fistula creation, which, while similar, is not the same as an AVM. The fistulas made are often at a distance to the brain (e.g. in the neck) and may not have the same combination of hypotension on the brain and hypertension in the venous drainage bed as a real AVM has. Furthermore, all AVMs have been in place a very long time, whereas any changes occurring in response to a fistula are relatively short term. The authors voice similar concerns. Their review of this field leads to the conclusion that despite admirable efforts of researchers to date, better models are needed.
Perhaps the best model is the real patient. In the modern era, an increase in observations obtained from humans with AVMs may be the most productive direction for such investigation. Pre- and postoperative flow imaging using perfusion MRI coupled with intraoperative pre- and post-resection direct brain visualization using laser speckle imaging, for example, might be more illuminating. Even the placement of a flow probe into the brain near the operative bed for postoperative monitoring would be both ethical and reasonable, given the risks patients must tolerate in the periresection period. In short, the authors remind us that there are still many opportunities for meaningful investigation in the NPPB field.
Rights and permissions
About this article
Cite this article
Gutiérrez-González, R., Pérez-Zamarron, A. & Rodríguez-Boto, G. Normal perfusion pressure breakthrough phenomenon: experimental models. Neurosurg Rev 37, 559–568 (2014). https://doi.org/10.1007/s10143-014-0549-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-014-0549-3