Abstract
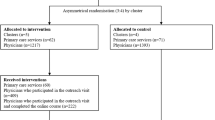
We previously showed that 40 % of clinically stable patients hospitalised for community-acquired pneumonia (CAP) are not switched to oral therapy in a timely fashion because of physicians’ barriers. We aimed to decrease this proportion by implementing a novel protocol. In a multi-centre controlled before-and-after study, we evaluated the effect of an implementation strategy tailored to previously identified barriers to an early switch. In three Dutch hospitals, a protocol dictating a timely switch strategy was implemented using educational sessions, pocket reminders and active involvement of nursing staff. Primary outcomes were the proportion of patients switched timely and the duration of intravenous antibiotic therapy. Length of hospital stay (LOS), patient outcome, education effects 6 months after implementation and implementation costs were secondary outcomes. Statistical analysis was performed using mixed-effects models. Prior to implementation, 146 patients were included and, after implementation, 213 patients were included. The case mix was comparable. The implementation did not change the proportion of patients switched on time (66 %). The median duration of intravenous antibiotic administration decreased from 4 days [interquartile range (IQR) 2–5] to 3 days (IQR 2–4), a decrease of 21 % [95 % confidence interval (CI) 11 %; 30 %) in the multi-variable analysis. LOS and patient outcome were comparable before and after implementation. Forty-three percent (56/129) of physicians attended the educational sessions. After 6 months, 24 % (10/42) of the interviewed attendees remembered the protocol’s main message. Cumulative implementation costs were €5,798 (€20/reduced intravenous treatment day). An implementation strategy tailored to previously identified barriers reduced the duration of intravenous antibiotic administration in hospitalised CAP patients by 1 day, at minimal cost.


Similar content being viewed by others
References
Hospital admissions pneumonia (2011) Statistics Netherlands (Dutch: Ziekenhuisopnamen pneumonie, Centraal Bureau voor Statistiek CBS). Available online at: http://statline.cbs.nl/StatWeb/publication/?VW=T&DM=SLNL&PA=71862ned&LA=NL. Accessed 1 Aug 2011
Athanassa Z, Makris G, Dimopoulos G, Falagas ME (2008) Early switch to oral treatment in patients with moderate to severe community-acquired pneumonia: a meta-analysis. Drugs 68(17):2469–2481
Kozma CM, Dickson M, Raut MK, Mody S, Fisher AC, Schein JR et al (2010) Economic benefit of a 1-day reduction in hospital stay for community-acquired pneumonia (CAP). J Med Econ 13(4):719–727
Engel MF, Postma DF, Hulscher ME, Teding van Berkhout F, Emmelot-Vonk MH, Sankatsing S et al (2013) Barriers to an early switch from intravenous to oral antibiotic therapy in hospitalised patients with CAP. Eur Respir J 41:123–130
Schouten JA, Hulscher ME, Trap-Liefers J, Akkermans RP, Kullberg BJ, Grol RP et al (2007) Tailored interventions to improve antibiotic use for lower respiratory tract infections in hospitals: a cluster-randomized, controlled trial. Clin Infect Dis 44(7):931–941
Baker R, Camosso-Stefinovic J, Gillies C, Shaw EJ, Cheater F, Flottorp S et al (2010) Tailored interventions to overcome identified barriers to change: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 3:CD005470
Hulscher ME, Grol RP, van der Meer JW (2010) Antibiotic prescribing in hospitals: a social and behavioural scientific approach. Lancet Infect Dis 10(3):167–175
Shojania KG, Jennings A, Mayhew A, Ramsay C, Eccles M, Grimshaw J (2010) Effect of point-of-care computer reminders on physician behaviour: a systematic review. CMAJ 182(5):E216–E225
Grimshaw J, Eccles M, Thomas R, MacLennan G, Ramsay C, Fraser C et al (2006) Toward evidence-based quality improvement. Evidence (and its limitations) of the effectiveness of guideline dissemination and implementation strategies 1966–1998. J Gen Intern Med 21(Suppl 2):S14–S20
Davey P, Brown E, Charani E, Fenelon L, Gould IM, Holmes A et al (2013) Interventions to improve antibiotic prescribing practices for hospital inpatients. Cochrane Database Syst Rev 4:CD003543
Ramirez JA, Bordon J (2001) Early switch from intravenous to oral antibiotics in hospitalized patients with bacteremic community-acquired Streptococcus pneumoniae pneumonia. Arch Intern Med 161(6):848–850
Halm EA, Fine MJ, Marrie TJ, Coley CM, Kapoor WN, Obrosky DS et al (1998) Time to clinical stability in patients hospitalized with community-acquired pneumonia: implications for practice guidelines. JAMA 279(18):1452–1457
Menéndez R, Torres A, Rodríguez de Castro F, Zalacaín R, Aspa J, Martín Villasclaras JJ et al (2004) Reaching stability in community-acquired pneumonia: the effects of the severity of disease, treatment, and the characteristics of patients. Clin Infect Dis 39(12):1783–1790
Wiersinga WJ, Bonten MJ, Boersma WG, Jonkers RE, Aleva RM, Kullberg BJ et al (2012) SWAB/NVALT (Dutch Working Party on Antibiotic Policy and Dutch Association of Chest Physicians) guidelines on the management of community-acquired pneumonia in adults. Neth J Med 70(2):90–101
Aleva RM, Boersma WG, Cox AL, van Haren EHJ, Schreurs AJM, Wijnands WJA et al (2003) Diagnosing and treating ‘community-acquired’ pneumonia (CAP). NVALT
Lim WS, Baudouin SV, George RC, Hill AT, Jamieson C, Le Jeune I et al (2009) BTS guidelines for the management of community acquired pneumonia in adults: update 2009. Thorax 64(Suppl 3):iii1–iii55
Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, Dean NC et al (2007) Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis 44(Suppl 2):S27–S72
Lim WS, van der Eerden MM, Laing R, Boersma WG, Karalus N, Town GI et al (2003) Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax 58(5):377–382
Fine MJ, Auble TE, Yealy DM, Hanusa BH, Weissfeld LA, Singer DE et al (1997) A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med 336(4):243–250
Ramirez JA, Srinath L, Ahkee S, Huang A, Raff MJ (1995) Early switch from intravenous to oral cephalosporins in the treatment of hospitalized patients with community-acquired pneumonia. Arch Intern Med 155(12):1273–1276
Robson LS, Shannon HS, Goldenhar LM, Hale AR (2001) Chapter 3. Before-and-after design: a simple evaluation design. Guide to evaluating the effectiveness of strategies for preventing work injuries: how to show whether a safety intervention really works. DHHS (NIOSH) Publication No. 2001-119, Cincinnati, OH, pp 19–20
Kirkpatrick DL, Kirkpatrick JD (2006) Evaluating training programs: the four levels, 3rd edn. Berrett-Koehler, San Francisco. ISBN-13: 978-1576753484
SurveyMonkey.com, LLC. Home page at: http://www.surveymonkey.com
Manual cost research (Dutch: Handleiding voor kostenonderzoek). Available online at: http://www.zorginstituutnederland.nl/binaries/content/documents/zinl-www/documenten/publicaties/overige-publicaties/1007-handleiding-voor-kostenonderzoek/Handleiding+voor+kostenonderzoek.pdf
Oosterheert JJ, Bonten MJ, Buskens E, Schneider MM, Hoepelman IM (2003) Algorithm to determine cost savings of targeting antimicrobial therapy based on results of rapid diagnostic testing. J Clin Microbiol 41(10):4708–4713
Hagaman JT, Yurkowski P, Trott A, Rouan GW (2005) Getting physicians to make “the switch”: the role of clinical guidelines in the management of community-acquired pneumonia. Am J Med Qual 20(1):15–21
McLaughlin CM, Bodasing N, Boyter AC, Fenelon C, Fox JG, Seaton RA (2005) Pharmacy-implemented guidelines on switching from intravenous to oral antibiotics: an intervention study. QJM 98(10):745–752
Avdic E, Cushinotto LA, Hughes AH, Hansen AR, Efird LE, Bartlett JG et al (2012) Impact of an antimicrobial stewardship intervention on shortening the duration of therapy for community-acquired pneumonia. Clin Infect Dis 54:1581–1587
Mertz D, Koller M, Haller P, Lampert ML, Plagge H, Hug B et al (2009) Outcomes of early switching from intravenous to oral antibiotics on medical wards. J Antimicrob Chemother 64(1):188–199
Blasi F, Iori I, Bulfoni A, Corrao S, Costantino S, Legnani D (2008) Can CAP guideline adherence improve patient outcome in internal medicine departments? Eur Respir J 32(4):902–910
Müller U, Exadaktylos A, Roeder C, Pisan M, Eggli S, Jüni P (2004) Effect of a flow chart on use of blood transfusions in primary total hip and knee replacement: prospective before and after study. BMJ 328(7445):934–938
Eccles M, Grimshaw J, Campbell M, Ramsay C (2003) Research designs for studies evaluating the effectiveness of change and improvement strategies. Qual Saf Health Care 12(1):47–52
Oosterheert JJ, Bonten MJ, Schneider MM, Buskens E, Lammers JW, Hustinx WM et al (2006) Effectiveness of early switch from intravenous to oral antibiotics in severe community acquired pneumonia: multicentre randomised trial. BMJ 333(7580):1193
Barlow G, Nathwani D, Williams F, Ogston S, Winter J, Jones M et al (2007) Reducing door-to-antibiotic time in community-acquired pneumonia: controlled before-and-after evaluation and cost-effectiveness analysis. Thorax 62(1):67–74
Fine MJ, Stone RA, Lave JR, Hough LJ, Obrosky DS, Mor MK et al (2003) Implementation of an evidence-based guideline to reduce duration of intravenous antibiotic therapy and length of stay for patients hospitalized with community-acquired pneumonia: a randomized controlled trial. Am J Med 115(5):343–351
Acknowledgments
We would like to thank G.A. de Wit (Associated Professor Medical Technology Assessment, Julius Centre for Health Sciences and Primary Care, University Medical Centre Utrecht) for sharing her expertise on economic evaluations with us. T.H.J. ten Cate (Professor of Medical Education, University Medical Centre Utrecht), thank you for the advice on the evaluation of education effects. Finally, we would like to thank L.C. Stijvers (Datamanager UPOD, University Medical Centre Utrecht) for his efforts in creating the database containing pharmacy data.
For this study, data from the Utrecht Patient Oriented Database (UPOD) were used. UPOD is an infrastructure of relational databases comprising data on patient characteristics, hospital discharge diagnoses, medical procedures, medication orders and laboratory tests for all patients treated at the University Medical Centre Utrecht (UMC Utrecht) since 2004. The UMC Utrecht is a 1,042-bed academic teaching hospital in the centre of the Netherlands, with about 28,000 clinical and 15,000 day-care hospitalizations and 334,000 outpatient visits annually. UPOD data acquisition and management is in accordance with current regulations concerning privacy and ethics. The structure and content of the UPOD have been described in more detail elsewhere (ten Berg MJ, Huisman A, van den Bemt PM, Schobben AF, Egberts AC, van Solinge WW. Linking laboratory and medication data: new opportunities for pharmacoepidemiological research. Clin Chem Lab Med. 2007;45(1):13–9).
Funding
This study was funded by the Netherlands Organisation for Health Research and Development (ZonMW Implementation Project, grant no. 171103003).
Conflict of interest
None to declare.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix 1
Appendix 2
Appendix 3
Appendix 4
Rights and permissions
About this article
Cite this article
Engel, M.F., Bruns, A.H.W., Hulscher, M.E.J.L. et al. A tailored implementation strategy to reduce the duration of intravenous antibiotic treatment in community-acquired pneumonia: a controlled before-and-after study. Eur J Clin Microbiol Infect Dis 33, 1897–1908 (2014). https://doi.org/10.1007/s10096-014-2158-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-014-2158-z