Abstract
Purpose
The strict lockdown implemented due the COVID-19 pandemic is generating a great impact on wellbeing and health-related quality of life (HRQoL) in people with cancer. We aimed to evaluate the efficacy and feasibility of an online home-based exercise intervention performed during a lockdown period analysing its effects on body composition, physical fitness, and HRQoL in breast cancer survivors.
Methods
Fifteen women with breast cancer receiving hormonal therapy (55.5 ± 6.7 years) were included in the study. The exercise intervention consisted of two weekly sessions of remotely supervised functional training (60 min per day) and two weekly sessions of unsupervised aerobic training (20–30 min/session; 60–85% of maximum heart rate) for a total of 16 weeks. DXA absorptiometry was used for the assessment of body composition. Functional assessment included cardiorespiratory fitness (CRF) by Rockport walking test, upper and lower body strength (grip strength, arm curl test, and chair stand test), walking speed (brisk walking test), and agility (8-foot up-and-go test). The HRQoL was evaluated with the QLQ-BR23 questionnaire. The adherence to the intervention was measured as the percentage of online classes attended.
Results
Rate of adherence for the online exercise intervention was 90 ± 17%. The exercise intervention induced significant (p < 0.05) improvements in physical fitness: CRF (+ 9%), right arm and lower limb strength (+ 10% and + 18%, respectively) and lower limbs lean mass (+ 2% and + 3.5% for left and right leg, respectively).
Conclusion
This feasibility study suggests that an online home-based exercise intervention during COVID-19 lockdown could improve physical fitness and body composition in breast cancer survivors even in a context of heightened concern for future health.
Similar content being viewed by others
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has caused an unprecedented international crisis. The World Health Organization (WHO) declared this situation a public health emergency of international concern [1]. Initial measures adopted by different countries to control of COVID-19 included important mobility restrictions with governments applying strict lockdowns that lasted several weeks or even months. Unfortunately, these measurements have had negative implications in population health and lifestyle. In fact, several studies have reported a reduction in physical activity (PA) levels [2, 3] with an increase in sedentary behavior produced by the afore-mentioned mobility restrictions.
In the area of oncology, the lockdown among cancer patients has entailed a great negative impact in their global wellbeing and consequently in their health-related quality of life (HRQoL). On this basis, a recent study reported that about 9 out of 10 of cancer patients showed an impairment in their security and daily functionality due to the COVID-19 pandemic [4, 5]. The benefits associated to physical exercise in cancer survivors as an adjuvant therapy have been widely described [6, 7]. In fact, over the last decades, supervised exercise interventions have shown multiple biopsychosocial benefits for people with cancer [8, 9]. However, due to this pandemic scenario, the global governments and the public health policies have framed “staying at home” as a preventive strategy. In this current situation associated with a global lockdown and restricted mobility, it is necessary to identify and explore new approaches and intervention strategies that enable adequate PA promotion among people with cancer. A possible solution tailored to this population could be the development of an online home-based exercise intervention [10, 11]. Specifically, for patients with cancer and survivors who are more vulnerable due to their global health status with an increased risk of exposure and virus infection.
In cancer survivors, home-based exercise has been considered as a safe and effective strategy to improve markers of health such as body composition, fatigue, functional capacity and HRQoL [12,13,14,15,16,17]. Focusing on breast cancer, home-based exercise programs have been developed during the last decades [18]. In these programs, patients are assessed and followed on a periodic basis, and perform exercise routines with the support of brochures, practical guides, or electronic materials [19]. Consequently, counseled exercise intervention could be an effective option for certain circumstances since a recent study suggested that a home-based exercise intervention developed during home confinement improved QoL in women who had suffered breast cancer [20]. Nonetheless, this was a pilot study and should be interpreted with caution due to the low number of participants (n = 2) [20].
One of the main limitations of an online home-based exercise intervention is that most are performed without supervision and consequently basic training variables such as the technique of the performed exercises, intensity or volume are not controlled and adapted for each participant [21]. Therefore, the previously mentioned variables could increase the risk of injury and adverse effects, generating a low training adherence. All these aspects underline the importance of developing a supervised exercise intervention adapted to the circumstances of each oncologic participant, in order to produce quantifiable improvements in physical function and HRQoL benefits in cancer survivors during COVID-19 lockdown. Hence, the aim of this study was to evaluate the efficacy and feasibility of an online home-based exercise intervention performed with a face-to-face and synchronous supervision during a lockdown period and, specifically, to analyze its effects on body composition, physical fitness and HRQoL in breast cancer survivors receiving hormonal therapy.
Material and methods
Study design
This is a quasi-experimental study with a pre-post design without a control group. The intervention had a duration of 16 weeks with the baseline assessment taking place in February 2020 while the follow-up assessment took place in June 2020. Initially, the intervention was designed to be performed with a face-to-face and supervised intervention. However, due to the unforeseen pandemic circumstance and the sudden lockdown, it was changed to an online home-based exercise intervention.
Data were collected at the beginning and the end of the study through face-to-face interviews. This was possible because pre-assessment was carried out 2-week before lockdown in Spain, and post-assessment took place in June, when social distancing and isolation measures were much more flexible. The intervention, however, did take place during the state of emergency and period of home confinement in Spain (from February to May 2020).
Participants and recruitment strategy
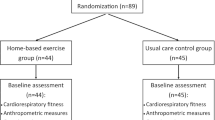
Twenty-one breast cancer women survivors were selected to participate in the study. Six abandoned the study (5 due to personal reasons and 1 was excluded because she had to stop the training due to COVID-19). Therefore, the final sample included 15 women (Fig. 1). All the participants belonged to the Asociación de mujeres aragonesas de cáncer genital y de mama (AMACGEMA) of Zaragoza (Spain). All participants were recruited for the study via email. A non-probabilistic convenience sampling was developed through an informative meeting that took place in January 2020 in the AMACGEMA venue.
The aims of the project and evaluations were explained in the mentioned meeting. Those that meet the following inclusion criteria were selected to participate in the present study: (i) age between 18 and 75 years old; (ii) diagnosed of breast cancer (stages I–III); (iii) > 6 months post-treatment (surgery, chemotherapy or radiotherapy); (iv) to be in active hormonal therapy; (v) no exercise medical contraindications (e.g., cardiovascular disease or neuromuscular disorders); and (vi) signing the written informed consent.
The exclusion criteria were (i) participants with cancer cachexia (body mass index < 20 kg/m2) [22]; (ii) being diagnosed of another primary and/or secondary tumor or being in metastatic stage; (iii) cardiac and or lung diagnosed problems (e.g., myocardial infarction, arrhythmia, angina, heart failure or chronic obstructive pulmonary disease); (iv) to have participated in an exercise program during the previous 6 months; or (v) to have severe immunosuppression or fever.
Sociodemographic variables
A self-constructed questionnaire contained 10 items was designed to describe the participants’ sociodemographic characteristics, education level, marital status, and other disease-related questions (received treatment, symptoms, and secondary effects).
Ethical committee
Eligible participants were informed about the project aims and purpose, and participation in the study was voluntary. All participants gave written informed consent prior their inclusion to the study. The present project was carried out in accordance with the principles of the Declaration of Helsinki and Good Clinical Practice guidelines. The project was approved by the Ethical Committee of the University of San Jorge (Zaragoza, Spain [nº006-19/20]). All participants were informed of the protocol of this study and agreed to participate voluntarily signing an informed consent.
Measures
Anthropometry and body composition
Height was measured with a stadiometer with 0.1 cm precision (SECA 225®, SECA, Hamburg, Germany), while weight was measured with a portable scale with a precision of 0.1 kg (SECA 861®, SECA, Hamburg, Germany). Waist and hip circumference were measured at the midpoint between the lowest rib and iliac crest at the end of a normal expiration and at the maximum diameter over the buttocks, respectively. Both measurements were performed with a non-elastic measuring tape with 0.1 cm precision (SECA 212®, SECA, Hamburg, Germany) with participants standing in anatomic position.
Dual-energy X-ray absorptiometry QDR-Explorer (QDR-Explorer, Hologic Corp., Software versión 12.4, Walthman, MA, USA) was used for the assessment of body composition. Body fat (kg and %) and lean body mass (kg) were obtained from whole-body scan. Lean body mass was obtained by subtracting bone mineral content from nonfat mass. The following sub-regions were also analyzed from the whole-body scan: lower and upper extremities and trunk.
Physical fitness assessment
The physical fitness related to functional capacity performance of participants was assessed with different tests.
A digital handgrip dynamometer (0.1 kg precision by Takey Smedley III T-19®, Scientific Instruments Co. Ltd., Niigata, Japan) was used to assess maximal handgrip strength. The “Arm Curl Test” was developed to assess upper limb strength [23]. Participants were asked to perform as many arm curls as possible in 30 s with a dumbbell of 2.5 kg weight.
The “chair stand test” was used to assess lower limb strength [23]. From a sitting position, participants were asked to repeatedly stand up and sit back down as fast as possible for 30 s. The number of stands was recorded.
The “8-foot up-and-go test” was used to assess agility [23]. From a sitting position, participants were asked to stand up and walk to a cone placed at 2.45 m, turn and return to a seated position. The time required was reported.
The “brisk walking test” was used to evaluate walking speed. Participants were asked to walk 30 m as fast as possible (running was not permitted). The time required was reported. Finally, cardiorespiratory fitness was (CRF) assessed by “Rockport walking test” [24]; the participants walked as fast as possible for one mile (1609 m). Post walk, heart rate, and time required were registered immediately after completion of the test.
All tests were repeated twice with a minute rest between attempts except for the “chair stand test”, “arm curl test”, and the “Rockport test” that were only performed once. The best attempt of each test was selected for further analyses.
Health-related quality of life
The European Organization for Research and Treatment of Cancer [25] Quality of Life Questionnaire and Breast Cancer specific module (EORTC-QLQ-BR23) [26] was used to evaluate HRQoL. This questionnaire contains 23 items that are divided into two dimensions. The first dimension includes four functional scales (body image [4 items], sexual functioning [2 items], sexual enjoyment [1 item], and future perspective [1 item]) while the second includes four symptom scales (systemic therapy side effects [7 items], breast symptoms [4 items], arm symptoms [3 items], upset by hair loss [1 item]). Each item is scored from 1 to 4. Scores were after linearly transformed to a 0 to 100 score. The highest scores are related to better functioning (except for sexual functioning and sexual enjoyment). On the other hand, higher scores in the symptom scale dimension are associated with a higher persistence of the symptoms.
Online home-based exercise program
The supervised exercise intervention had a duration of 16 weeks. The first 2 weeks were focused on exercise familiarization. All the sessions were developed through ZOOM (Zoom Video Communications, Inc., 2020) (Fig. 2).
The exercise intervention included four weekly training sessions divided into two functional supervised training sessions and two aerobic unsupervised training sessions. The supervised part consisted of the trainer leading the session by connecting online synchronously with the participants and directing the training. During the connection, the participants could watch the performance, were encouraged, and could interact and give feedback or ask questions. The trainer could also assess the participants performance and give individual or group feedback or corrections when necessary.
The supervised sessions had a duration of 60 min. Each session was divided into warm-up (10 min), a main part of the training (40 min), and cool down (10 min). All the sessions included a combined circuit of 8–12 functional exercises to improve strength and CRF (squats, split squat, walking lunges, calf rise, glute bridge, band pull down, core, walking/jogging on the spot, lateral step up with biceps curl or shoulder press, punches, jumping jack). Exercises were developed with body weight, elastic bands, and home available material (such as small plastic bottles of water or milk, or shopping bags). For the functional strength exercises, a 10–12 repetition protocol was developed, while the aerobic exercises lasted around 30 s. Two series were performed until week 12 and three series from week 13 to 16. A minimum rest of 90 s was established between exercises.
Participants were asked to use a heart rate monitor during all the sessions. The work intensities ranged from 60 to 85% of maximum heart rate (HRmax) obtained from the Rockport test and calculated through the Karvonen formula [27]. Rating of perceived exertion was also registered at the end of the warm-up and main training using the Borg scale [28].
Finally, to improve the specificity of the program and follow the WHO physical activity recommendations, we recommended participants to add each week two home aerobic unsupervised sessions (20–30 min/session; 60–85% HRmax). These aerobic sessions could include self-selected exercises such as dancing choreographies, indoor cycling, elliptical bike, or the use of other home available tools that would elicit a similar stimulus.
Safety and adherence
Daily adherence and safety to the intervention were monitored by means of a register of attendance. Moreover, to ensure the safety and welfare of participants involved in the research, the protect rights of human subjects and occurrence of adverse events were monitored. Finally, to determine adherence to the training, we considered a session to be completed when 80–90% of the planned exercises were successfully performed.
Statistical analyses
The Shapiro–Wilk test was used to test the normality of the outcomes. Mean, standard deviation, and confidence intervals 95% are presented for continuous outcomes. Categorical outcomes are expressed as absolute values and percentages. To test the differences between different moments of the intervention (pre-post) for the same group, the paired samples t test was used. The relative change (change percentage) was calculated to test the effect of the intervention. Additionally, the standardized effect size (ES) was calculated by Cohen’s d, with values from 0.2–0.5 representing small effect; 0.5–0.8 moderate effect and > 0.8 large effect.
All the analyses were performed with SPSS v.21 (SPSS Institute Inc., IL, EUA). The level of significance was set at p < 0.05.
Results
Participants main characteristics
Sociodemographic characteristics (age, education level, and marital status) and variables associated with the disease (received treatment, disease recurrence, symptoms, and negative effects) are presented in Table 1.
Safety and adherence
No adverse events or health issues during the exercise intervention were noted. Adherence to the intervention averaged 90 ± 17%.
Physical performance
Results for the baseline and post-intervention are presented in Table 2. Significant improvements were found for handgrip strength of the right arm, lower limbs strength, and CRF (all p < 0.05; ES: 0.84, 0.76, and 1.17, respectively).
Anthropometry and body composition
Anthropometric characteristics and body composition variables are presented in Table 3. Breast cancer survivors increased lean mass at both right and left legs from the beginning to the end of the exercise intervention (p < 0.05; ES 0.74 and 1.01 for left and right leg, respectively). No significant changes were found for the other variables evaluated (all p > 0.05).
Health-related quality of life
HRQoL results are presented in Table 4. Significant changes were found for the future perspectives domain which were lower at the end of the program (75.60 ± 29.45 vs 45.34 ± 36.10; p < 0.05; ES 0.90). No other significant differences were found for the rest of the assessed dimensions. Participants did not provide responses to the scales on sexual enjoyment and hair loss.
Discussion
The results of the present study show that an online home-based exercise intervention is an effective and safe strategy to improve physical fitness and lower limbs lean mass on breast cancer survivors.
The COVID-19 pandemic has impacted every aspect of life producing increased levels of sedentary time and reduced physical activity levels. These changes will be deleterious for the health of the global population and will be critical for cancer survivors. Consequently, home-based exercise interventions could be an excellent choice for people affected by cancer.
The use of e-Health in oncology has started a new era that goes beyond the traditional health care model [29]. Home-based exercise interventions have been shown as a valid strategy that can provide benefits in CRF, strength, PA levels, HRQoL, and body composition on cancer survivors [15, 30]. Results obtained in the present study show that an online home-based exercise intervention performed in a context of lockdown enables the maintenance of physical function in female breast cancer survivors (our participants improved the score obtained in the chair stand test, that measures the ability of participants to stand and sit on a chair a task that everyone develops daily). Our results are in overall agreement and extend those of DeNysschen et al. [14], who with an 8-week home-based exercise intervention applied in female breast cancer survivors (n = 26), who were receiving prolonged hormonal treatment, showed improvements in handgrip strength, arm curl test and chair stand test, but not in CRF [14]. The differences in CRF between studies can be attributed to both the duration of the exercise training program (8 weeks vs 16 weeks) and the test used to assess the CRF (3 min step test vs Rockport test).
It is important to understand that a reduction of muscle mass is currently considered a prognostic factor of the disease and is associated with a higher degree of functional limitations and dependency, and with lower cancer survival rates [31, 32]. Several studies have demonstrated a pronounced muscle strength decline (upper- and lower-body) in breast cancer survivors [32,33,34]. Nowadays, handgrip strength is known as one of the prognostic factors of sarcopenia [35, 36]. Focusing on breast cancer, handgrip strength has been directly associated with HRQoL and inversely with the adverse secondary effects of cancer treatment [37]. Our results, similarly to those of Denysschen et al. [14], have shown handgrip strength improvements, with an increase of the right arm (19.7 kg pre- vs. 21.7 kg post- intervention). Also, in a recent case study developed during the COVID-19 lockdown, one of the two participants included in the study showed improvements in handgrip strength (27.4 kg pre- vs. 34.9 kg post-intervention) after a 16-week exercise intervention [38].
Functional training in cancer patients and survivors is an emerging topic. For years, most researchers have focused on determining the effectivity of exercise programs based on traditional strength exercises. Jones et al. [39], in a recent study developed in breast cancer survivors (n = 51), implemented a 12-week intervention based on a combined aerobic and resistance circuit, observing positive changes in physical fitness (CRF and upper and lower limbs strength), similar to those found in our study.
Regarding body composition, Lahart et al. [40] in a 6-month home-based PA intervention in breast cancer survivors found significant improvements in body weight and BMI. However, in our study only changes on legs lean mass from baseline to the end of the online program were detected. A possible reason for these differences between studies could be due to the duration of the studies (16 weeks vs 6 months). Moreover, the method to assess body composition was not the same (dual-energy X-ray absorptiometry vs bioelectrical impedance). It is also important to note that our study was performed in a context of COVID-19 lockdown in which people have been forced to stay at home and, consequently, probably had to modify their lifestyle [2, 41, 42].
Cancer patients express clinically increased psychological symptoms (depression and anxiety) during the disease [43] and an online intervention could be a viable strategy to improve HRQoL and motivation towards exercise and, consequently, reduce these symptoms [15]. The results of the present study obtained with the EORTC-QLQ-BR23 did not show a positive effect of exercise on body image or secondary treatment effects. Surprisingly, we found a significant decrease in future perspective scores. This could be partially explained by the confinement that all participants had to suffer while the intervention took place, a situation that could generate uncertainty, anxiety, or fear to the near future. In the same line, a recent study demonstrated that the COVID-19 pandemic negatively affected the emotional health of women diagnosed with primary breast cancer who showed higher general emotional vulnerability due to the disruption of treatments generated by COVID-19 [44].
There are some limitations in this study that should be noted. First, our sample size was limited. Furthermore, no sample size calculation was performed, as the cohort analyzed in the present study was a convenience sample (i.e., all participants belonged to the AMACGEMA meeting the eligibility criteria). However, it is important to note that this study has been undertaken thought special circumstances due to the COVID-19 pandemic. Therefore, it was extremely difficult to have a greater number of participants. Second, the absence of a control group did not allow to establish a solid relationship of these findings. However, given that physical exercise in breast cancer survivors is highly recommended because of its health benefits, and the circumstances of pandemic and confinement made it highly likely that regular physical activity would decrease, we considered that it was unethical to leave a group without a training program. Another limitation is the lack of control on nutritional variables or dietary habits, which can largely influence body composition.
Nonetheless, the present study has several strengths such as the possibility of adapting the study methodology to the circumstances of the COVID-19 pandemic and the associated lockdown. Also, noteworthy is the high adherence of participants to the online home-based exercise intervention under these circumstances.
Conclusion
This feasibility study suggests that an online home-based exercise intervention performed during a confinement period is safe and beneficial for breast cancer survivors who showed improvements in physical fitness and lower limbs lean mass. Further larger studies (particularly, controlled trials) are needed to evaluate which is the best intervention to improve both physical and psychological health-related markers.
Data availability
All data that support the findings of this study are available from the corresponding author upon reasonable request. Source data are provided with this paper.
Code availability
Not applicable.
References
World Health Organization (2020) W.H.O. COVID-19 Public Health Emergency of International Concern (PHEIC) Global research and innovation forum. Available from: https://www.who.int/publications/m/item/covid-19-public-health-emergency-of-international-concern-(pheic)-global-research-and-innovation-forum
Ammar A et al (2020) Effects of COVID-19 home confinement on eating behaviour and physical activity: results of the ECLB-COVID19 International Online Survey. Nutrients 12(6):1583
Burtscher J, Burtscher M, Millet GP (2020) (Indoor) isolation, stress, and physical inactivity: Vicious circles accelerated by COVID-19? Scand J Med Sci Sports 30(8):1544–1545
Ciazynska M et al (2020) Quality of life of cancer patients during coronavirus disease (COVID-19) pandemic. Psychooncology 29 (9): o. 1377–1379
Qian Y et al (2020) A survey on physical and mental distress among cancer patients during the COVID-19 epidemic in Wuhan, China. J Palliat Med 23(7):888–889
Christensen JF, Simonsen C, Hojman P (2018) Exercise training in cancer control and treatment. Compr Physiol 9(1):165–205
Segal R et al (2017) Exercise for people with cancer: a systematic review. Curr Oncol 24(4):e290–e315
Liska TM, Kolen AM (2020) The role of physical activity in cancer survivors’ quality of life. Health Qual Life Outcomes 18(1):197
Hilfiker R et al (2018) Exercise and other non-pharmaceutical interventions for cancer-related fatigue in patients during or after cancer treatment: a systematic review incorporating an indirect-comparisons meta-analysis. Br J Sports Med 52(10):651–658
Baez M et al (2017) Effects of online group exercises for older adults on physical, psychological and social wellbeing: a randomized pilot trial. Peer J 5:e3150
Dong X et al (2019) The effects of the combined exercise intervention based on internet and social media software (CEIBISMS) on quality of life, muscle strength and cardiorespiratory capacity in Chinese postoperative breast cancer patients:a randomized controlled trial. Health Qual Life Outcomes 17(1):109
Stefani L et al (2019) Effects of a home-based exercise rehabilitation program for cancer survivors. J Sports Med Phys Fitness 59(5):846–852
Kim SH et al (2018) The effect on bone outcomes of home-based exercise intervention for prostate cancer survivors receiving androgen deprivation therapy: a pilot randomized controlled trial. Cancer Nurs 41(5):379–388
DeNysschen CA et al (2014) Exercise intervention in breast cancer patients with aromatase inhibitor-associated arthralgia: a pilot study. Eur J Cancer Care (Engl) 23(4):493–501
Jacobsen PB et al (2013) Effects of self-directed stress management training and home-based exercise on quality of life in cancer patients receiving chemotherapy: a randomized controlled trial. Psychooncology 22(6):1229–1235
Natalucci V et al (2021) Effects of a home-based lifestyle intervention program on cardiometabolic health in breast cancer survivors during the COVID-19 lockdown. J Clin Med 10(12)
Soriano-Maldonado A et al (2022) Effects of a 12-week supervised resistance training program, combined with home-based physical activity, on physical fitness and quality of life in female breast cancer survivors: the EFICAN randomized controlled trial. J Cancer Surviv
Coughlin SS et al (2019) A review of home-based physical activity interventions for breast cancer survivors. Curr Cancer Rep 1(1):6–12
Support MC (2015) Get active, feel good exercise DVD; Available from: https://be.macmillan.org.uk/Downloads/CancerInformation/LivingWithAndAfterCancer/MAC14016DVDFeelGoodDVDBooklet.pdf
Grazioli EC et al (2020) New strategy of home-based exercise during pandemic COVID-19 in breast cancer patients: a case study. Sustainability 12
Lopez C et al (2020) Variability and limitations in home-based exercise program descriptions in oncology: a scoping review. Support Care Cancer 28(9):4005–4017
Dev R (2019) Measuring cachexia-diagnostic criteria. Ann Palliat Med 8(1):24–32
Rikli RE, Jones CJ (2013) Senior fitness test manual. Human kinetics
Kline GM et al (1987) Estimation of VO2max from a one-mile track walk, gender, age, and body weight. Med Sci Sports Exerc 19(3):253–259
EORTC (2001) EORTC-C30 scoring manual. 3rd edn:[Available from: https://www.eortc.org/app/uploads/sites/2/2018/02/SCmanual.pdf
Sprangers MA et al (1996) The European Organization for Research and Treatment of Cancer breast cancer-specific quality-of-life questionnaire module: first results from a three-country field study. J Clin Oncol 14(10):2756–2768
Campbell KL et al (2019) Exercise Guidelines for Cancer Survivors: Consensus Statement from International Multidisciplinary Roundtable. Med Sci Sports Exerc 51(11):2375–2390
Williams N (2017) The Borg Rating of Perceived Exertion (RPE) scale. Occup Med 67(5):404–405
Penedo FJ et al (2020) The increasing value of eHealth in the delivery of patient-centred cancer care. Lancet Oncol 21(5):e240–e251
Batalik L et al (2021) Home-based aerobic and resistance exercise interventions in cancer patients and survivors: a systematic review. Cancers (Basel) 13(8)
Chindapasirt J (2015) Sarcopenia in cancer patients. Asian Pac J Cancer Prev 16(18):8075–8077
Christensen JF et al (2014) Muscle dysfunction in cancer patients. Ann Oncol 25(5):947–958
Neil-Sztramko SE et al (2014) Aerobic capacity and upper limb strength are reduced in women diagnosed with breast cancer: a systematic review. J Physiother 60(4):189–200
Kroenke CH et al (2004) Functional impact of breast cancer by age at diagnosis. J Clin Oncol 22(10):1849–1856
Cruz-Jentoft AJ et al (2019) Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 48(1):16–31
Benavides-Rodriguez L et al. (2017) Relationship between handgrip strength and muscle mass in female survivors of breast cancer: a mediation analysis. Nutrients 9(7)
Cantarero-Villanueva I et al (2012) The handgrip strength test as a measure of function in breast cancer survivors: relationship to cancer-related symptoms and physical and physiologic parameters. Am J Phys Med Rehabil 91(9):774–782
Grazioli E et al (2020) New strategy of home-based exercise during pandemic COVID-19 in breast cancer patients: a case study. Sustainability 12(17):6940
Jones LM et al (2020) Circuit resistance training and cardiovascular health in breast cancer survivors. Eur J Cancer Care (Engl) 29(4):e13231
Lahart IM et al (2016) Randomised controlled trial of a home-based physical activity intervention in breast cancer survivors. BMC Cancer 16:234
Di Renzo L et al (2020) Eating habits and lifestyle changes during COVID-19 lockdown: an Italian survey. J Transl Med 18(1):229
Bhutani S, Cooper JA (2020) COVID-19-Related Home Confinement in Adults: Weight Gain Risks and Opportunities. Obesity (Silver Spring) 28(9):1576–1577
Carlson LE et al (2004) High levels of untreated distress and fatigue in cancer patients. Br J Cancer 90(12):2297–2304
Swainston J et al (2020) COVID-19 Lockdown and Its Adverse Impact on Psychological Health in Breast Cancer. Front Psychol 11:2033
Acknowledgements
The authors are also grateful to all the participants whose cooperation made this study possible.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Each author has substantially contributed to conducting the underlying research and drafting this manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The present project was carried out in accordance with the principles of the Declaration of Helsinki and Good Clinical Practice guidelines. The project was approved by the Ethical Committee of the University of San Jorge, Spain (nº006-19/20).
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflicts of interests
The authors declare that they have no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sagarra-Romero, L., Butragueño, J., Gomez-Bruton, A. et al. Effects of an online home-based exercise intervention on breast cancer survivors during COVID-19 lockdown: a feasibility study. Support Care Cancer 30, 6287–6297 (2022). https://doi.org/10.1007/s00520-022-07069-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-022-07069-4