Abstract
The present narrative review on albumin dialysis provides evidence-based and expert opinion guidelines for clinicians caring for adult patients with different types of liver failure. The review was prepared by an expert panel of 13 members with liver and ntensive care expertise in extracorporeal liver support therapies for the management of patients with liver failure. The coordinating committee developed the questions according to their importance in the management of patients with liver failure. For each indication, experts conducted a comprehensive review of the literature aiming to identify the best available evidence and assessed the quality of evidence based on the literature and their experience. Summary statements and expert’s recommendations covered all indications of albumin dialysis therapy in patients with liver failure, timing and intensity of treatment, efficacy, technical issues related to the device and safety. The panel supports the data from the literature that albumin dialysis showed a beneficial effect on hepatic encephalopathy, refractory pruritus, renal function, reduction of cholestasis and jaundice. However, the trials lacked to show a clear beneficial effect on overall survival. A short-term survival benefit at 15 and 21 days respectively in acute and acute-on-chronic liver failure has been reported in recent studies. The technique should be limited to patients with a transplant project, to centers experienced in the management of advanced liver disease. The use of extracorporeal albumin dialysis could be beneficial in selected patients with advanced liver diseases listed for transplant or with a transplant project. Waiting future large randomized controlled trials, this panel experts’ statements may help careful patient selection and better treatment modalities.




Similar content being viewed by others
Abbreviations
- ABT:
-
Albumin-bound toxin
- ACLF:
-
Acute-on-chronic liver failure
- ALF:
-
Acute liver failure
- DAMP:
-
Damage-associated molecular proteins
- HE:
-
Hepatic encephalopathy
- HLI:
-
Hypoxic liver injury
- HSA:
-
Human serum albumin
- ICU:
-
Intensive care unit
- LTx:
-
Liver transplantation
- MARS™:
-
Molecular Adsorbent Recirculating System
- MELD:
-
Model of end-stage liver disease (score)
- MOST:
-
Multiorgan support organ support therapies
- PHLF:
-
Post-hepatectomy liver failure
- RCA:
-
Regional citrate anticoagulation
- HVPE:
-
High volume plasma exchange
- RCT:
-
Randomized controlled trial
- SMT:
-
Standard medical therapy
- VAS:
-
Visual analogue scale
References
Saliba F, Samuel D (2015) Artificial liver support: a real step forward. Minerva Med 106:35–43
Camus C, Locher C, Saliba F, Goubaux B, Bonadona A, Lavayssiere L, Paugam C, Quinart A, Barbot O, Dharancy S, Delafosse B, Pichon N, Barraud H, Galbois A, Veber B, Cayot S, Souche B (2020) Outcome of patients treated with molecular adsorbent recirculating system albumin dialysis: a national multicenter study. JGH Open Open Access J Gastroenterol Hepatol 4:757–763
Kanjo A, Ocskay K, Gede N, Kiss S, Szakács Z, Párniczky A, Mitzner S, Stange J, Hegyi P, Molnár Z (2021) Efficacy and safety of liver support devices in acute and hyperacute liver failure: a systematic review and network meta-analysis. Sci Rep 11:4189
Alshamsi F, Alshammari K, Belley-Cote E, Dionne J, Albrahim T, Albudoor B, Ismail M, Al-Judaibi B, Baw B, Subramanian RM, Steadman R, Galusca D, Huang DT, Nanchal R, Al Quraini M, Yuan Y, Alhazzani W (2020) Extracorporeal liver support in patients with liver failure: a systematic review and meta-analysis of randomized trials. Intensive Care Med 46:1–16
Tandon R, Froghi S (2021) Artificial liver support systems. J Gastroenterol Hepatol 36:1164–1179
Ocskay K, Kanjo A, Gede N, Szakács Z, Pár G, Erőss B, Stange J, Mitzner S, Hegyi P, Molnár Z (2021) Uncertainty in the impact of liver support systems in acute-on-chronic liver failure: a systematic review and network meta-analysis. Ann Intensive Care 11(1):10. https://doi.org/10.1186/s13613-020-00795-0
Ronco C, Ricci Z, Husain-Syed F (2019) From multiple organ support therapy to extracorporeal organ support in critically ill patients. Blood Purif 48:99–105
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schunemann HJ (2008) GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336:924–926
Bernardi M, Angeli P, Claria J, Moreau R, Gines P, Jalan R, Caraceni P, Fernandez J, Gerbes AL, O’Brien AJ, Trebicka J, Thevenot T, Arroyo V (2020) Albumin in decompensated cirrhosis: new concepts and perspectives. Gut 69:1127–1138
Peters TJ (1995) All about albumin: biochemistry, genetics, and medical applications. Academic Press, San Diego
Quinlan GJ, Martin GS, Evans TW (2005) Albumin: biochemical properties and therapeutic potential. Hepatology 41:1211–1219
Sleep D (2015) Albumin and its application in drug delivery. Expert Opin Drug Deliv 12:793–812
Merlot AM, Kalinowski DS, Richardson DR (2014) Unraveling the mysteries of serum albumin-more than just a serum protein. Front Physiol 5:299
Bern M, Sand KM, Nilsen J, Sandlie I, Andersen JT (2015) The role of albumin receptors in regulation of albumin homeostasis: implications for drug delivery. J Control Release Off J Control Release Soc 211:144–162
Galis Z, Ghitescu L, Simionescu M (1988) Fatty acids binding to albumin increases its uptake and transcytosis by the lung capillary endothelium. Eur J Cell Biol 47:358–365
Larsen FS, Schmidt LE, Bernsmeier C, Rasmussen A, Isoniemi H, Patel VC, Triantafyllou E, Bernal W, Auzinger G, Shawcross D, Eefsen M, Bjerring PN, Clemmesen JO, Hockerstedt K, Frederiksen HJ, Hansen BA, Antoniades CG, Wendon J (2016) High-volume plasma exchange in patients with acute liver failure: an open randomised controlled trial. J Hepatol 64:69–78
O’Grady JG, Gimson AE, O’Brien CJ, Pucknell A, Hughes RD, Williams R (1988) Controlled trials of charcoal hemoperfusion and prognostic factors in fulminant hepatic failure. Gastroenterology 94:1186–1192
Mitzner S, Klammt S, Stange J, Schmidt R (2006) Albumin regeneration in liver support-comparison of different methods. Ther Apher Dial Off Peer-Rev J Int Soc Apher Jpn Soc Apher Jpn Soc Dial Ther 10:108–117
Saliba F, Camus C, Durand F, Mathurin P, Letierce A, Delafosse B, Barange K, Perrigault PF, Belnard M, Ichai P, Samuel D (2013) Albumin dialysis with a noncell artificial liver support device in patients with acute liver failure: a randomized, controlled trial. Ann Intern Med 159:522–531
Ilonen I, Koivusalo AM, Repo H, Höckerstedt K, Isoniemi H (2008) Cytokine profiles in acute liver failure treated with albumin dialysis. Artif Organs 32:52–60
Schmidt LE, Tofteng F, Strauss GI, Larsen FS (2004) Effect of treatment with the Molecular Adsorbents Recirculating System on arterial amino acid levels and cerebral amino acid metabolism in patients with hepatic encephalopathy. Scand J Gastroenterol 39:974–980
Kantola T, Koivusalo AM, Höckerstedt K, Isoniemi H (2008) The effect of molecular adsorbent recirculating system treatment on survival, native liver recovery, and need for liver transplantation in acute liver failure patients. Transpl Int 21:857–866
Camus C, Lavoué S, Gacouin A, Compagnon P, Boudjéma K, Jacquelinet C, Thomas R, Le Tulzo Y (2009) Liver transplantation avoided in patients with fulminant hepatic failure who received albumin dialysis with the molecular adsorbent recirculating system while on the waiting list: impact of the duration of therapy. Ther Apher Dial Off Peer-Rev J Int Soc Apher Jpn Soc Apher Jpn Soc Dial Ther 13:549–555
Gerth HU, Pohlen M, Thölking G, Pavenstädt H, Brand M, Wilms C, Hüsing-Kabar A, Görlich D, Kabar I, Schmidt HH (2017) Molecular adsorbent recirculating system (MARS) in acute liver injury and graft dysfunction: results from a case-control study. PLoS One 12:e0175529
MacDonald AJ, Subramanian RM, Olson JC, Speiser JL, Durkalski-Mauldin VL, Abraldes JG, Bigam DL, Flynn MM, Rapaka B, Shropshire BM, Vora RS, Karvellas CJ (2022) Use of the molecular adsorbent recirculating system in acute liver failure: results of a multicenter propensity score-matched study. Crit Care Med 50(2):286–295
Arroyo V, Moreau R, Jalan R (2020) Acute-on-chronic liver failure. N Engl J Med 382:2137–2145
Sen S, Davies NA, Mookerjee RP, Cheshire LM, Hodges SJ, Williams R, Jalan R (2004) Pathophysiological effects of albumin dialysis in acute-on-chronic liver failure: a randomized controlled study. Liver Transpl Off Publ Am Assoc Study Liver Dis Int Liver Transpl Soc 10:1109–1119
Catalina MV, Barrio J, Anaya F, Salcedo M, Rincón D, Clemente G, Bañares R (2003) Hepatic and systemic haemodynamic changes after MARS in patients with acute on chronic liver failure. Liver Int Off J Int Assoc Study Liver 23(Suppl 3):39–43
Laleman W, Wilmer A, Evenepoel P, Elst IV, Zeegers M, Zaman Z, Verslype C, Fevery J, Nevens F (2006) Effect of the molecular adsorbent recirculating system and Prometheus devices on systemic haemodynamics and vasoactive agents in patients with acute-on-chronic alcoholic liver failure. Crit Care (Lond, Engl) 10:R108
Sen S, Mookerjee RP, Cheshire LM, Davies NA, Williams R, Jalan R (2005) Albumin dialysis reduces portal pressure acutely in patients with severe alcoholic hepatitis. J Hepatol 43:142–148
Stadlbauer V, Krisper P, Aigner R, Haditsch B, Jung A, Lackner C, Stauber RE (2006) Effect of extracorporeal liver support by MARS and Prometheus on serum cytokines in acute-on-chronic liver failure. Crit Care (Lond, Engl) 10:R169
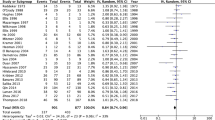
Banares R, Ibanez-Samaniego L, Torner JM, Pavesi M, Olmedo C, Catalina MV, Albillos A, Larsen FS, Nevens F, Hassanein T, Schmidt H, Heeman U, Jalan R, Moreau R, Arroyo V (2019) Meta-analysis of individual patient data of albumin dialysis in acute-on-chronic liver failure: focus on treatment intensity. Ther Adv Gastroenterol 12:1–12
Khuroo MS, Khuroo MS, Farahat KL (2004) Molecular adsorbent recirculating system for acute and acute-on-chronic liver failure: a meta-analysis. Liver Transpl Off Publ Am Assoc Study Liver Dis Int Liver Transpl Soc 10:1099–1106
Liu Y, Kang YZ, Xia WZ, Zhou HC, Wang Y, Gao Y (2009) Artificial and bioartificial liver support systems for acute and acute-on-chronic liver failure: a meta-analysis. Nan Fang Yi Ke Da Xue Xue Bao 29:1529–1532
Stutchfield BM, Simpson K, Wigmore SJ (2011) Systematic review and meta-analysis of survival following extracorporeal liver support. Br J Surg 98:623–631
Vaid A, Chweich H, Balk EM, Jaber BL (2012) Molecular adsorbent recirculating system as artificial support therapy for liver failure: a meta-analysis. ASAIO J 58:51–59
Zheng Z, Li X, Li Z, Ma X (2013) Artificial and bioartificial liver support systems for acute and acute-on-chronic hepatic failure: a meta-analysis and meta-regression. Exp Ther Med 6:929–936
Banares R, Nevens F, Larsen FS, Jalan R, Albillos A, Dollinger M, Saliba F, Sauerbruch T, Klammt S, Ockenga J, Pares A, Wendon J, Brunnler T, Kramer L, Mathurin P, de la Mata M, Gasbarrini A, Mullhaupt B, Wilmer A, Laleman W, Eefsen M, Sen S, Zipprich A, Tenorio T, Pavesi M, Schmidt HH, Mitzner S, Williams R, Arroyo V (2013) Extracorporeal albumin dialysis with the molecular adsorbent recirculating system in acute-on-chronic liver failure: the RELIEF trial. Hepatology 57:1153–1162
Hassanein TI, Tofteng F, Brown RS Jr, McGuire B, Lynch P, Mehta R, Larsen FS, Gornbein J, Stange J, Blei AT (2007) Randomized controlled study of extracorporeal albumin dialysis for hepatic encephalopathy in advanced cirrhosis. Hepatology 46:1853–1862
Heemann U, Treichel U, Loock J, Philipp T, Gerken G, Malago M, Klammt S, Loehr M, Liebe S, Mitzner S, Schmidt R, Stange J (2002) Albumin dialysis in cirrhosis with superimposed acute liver injury: a prospective, controlled study. Hepatology 36:949–958
Mitzner SR, Stange J, Klammt S, Risler T, Erley CM, Bader BD, Berger ED, Lauchart W, Peszynski P, Freytag J, Hickstein H, Loock J, Löhr JM, Liebe S, Emmrich J, Korten G, Schmidt R (2000) Improvement of hepatorenal syndrome with extracorporeal albumin dialysis MARS: results of a prospective, randomized, controlled clinical trial. Liver Transpl Off Publ Am Assoc Study Liver Dis Int Liver Transpl Soc 6:277–286
Kribben A, Gerken G, Haag S, Herget-Rosenthal S, Treichel U, Betz C, Sarrazin C, Hoste E, Van Vlierberghe H, Escorsell A, Hafer C, Schreiner O, Galle PR, Mancini E, Caraceni P, Karvellas CJ, Salmhofer H, Knotek M, Gines P, Kozik-Jaromin J, Rifai K (2012) Effects of fractionated plasma separation and adsorption on survival in patients with acute-on-chronic liver failure. Gastroenterology 142(782–789):e783
Wong F, Raina N, Richardson R (2010) Molecular adsorbent recirculating system is ineffective in the management of type 1 hepatorenal syndrome in patients with cirrhosis with ascites who have failed vasoconstrictor treatment. Gut 59:381–386
Moreau R, Jalan R, Gines P, Pavesi M, Angeli P, Cordoba J, Durand F, Gustot T, Saliba F, Domenicali M, Gerbes A, Wendon J, Alessandria C, Laleman W, Zeuzem S, Trebicka J, Bernardi M, Arroyo V (2013) Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis. Gastroenterology 144(1426–1437):1437.e1421–1429
European Association for the Study of the Liver (2017) EASL Clinical Practice Guidelines: the diagnosis and management of patients with primary biliary cholangitis. J Hepatol 67:145–172
Lindor KD, Bowlus CL, Boyer J, Levy C, Mayo M (2019) Primary biliary cholangitis: 2018 practice guidance from the American Association for the Study of Liver Diseases. Hepatology 69:394–419
Bachs L, Parés A, Elena M, Piera C, Rodés J (1992) Effects of long-term rifampicin administration in primary biliary cirrhosis. Gastroenterology 102:2077–2080
Wolfhagen FH, Sternieri E, Hop WC, Vitale G, Bertolotti M, Van Buuren HR (1997) Oral naltrexone treatment for cholestatic pruritus: a double-blind, placebo-controlled study. Gastroenterology 113:1264–1269
Mayo MJ, Handem I, Saldana S, Jacobe H, Getachew Y, Rush AJ (2007) Sertraline as a first-line treatment for cholestatic pruritus. Hepatology 45:666–674
Reig A, Sesé P, Parés A (2018) Effects of bezafibrate on outcome and pruritus in primary biliary cholangitis with suboptimal ursodeoxycholic acid response. Am J Gastroenterol 113:49–55
Hegade VS, Kendrick SF, Dobbins RL, Miller SR, Thompson D, Richards D, Storey J, Dukes GE, Corrigan M, Oude Elferink RP, Beuers U, Hirschfield GM, Jones DE (2017) Effect of ileal bile acid transporter inhibitor GSK2330672 on pruritus in primary biliary cholangitis: a double-blind, randomised, placebo-controlled, crossover, phase 2a study. Lancet 389:1114–1123
Kremer AE, Oude Elferink RP, Beuers U (2011) Pathophysiology and current management of pruritus in liver disease. Clin Res Hepatol Gastroenterol 35:89–97
Parés A, Herrera M, Avilés J, Sanz M, Mas A (2010) Treatment of resistant pruritus from cholestasis with albumin dialysis: combined analysis of patients from three centers. J Hepatol 53:307–312
Leckie P, Tritto G, Mookerjee R, Davies N, Jones D, Jalan R (2012) ‘Out-patient’ albumin dialysis for cholestatic patients with intractable pruritus. Aliment Pharmacol Ther 35:696–704
Macia M, Avilés J, Navarro J, Morales S, García J (2003) Efficacy of molecular adsorbent recirculating system for the treatment of intractable pruritus in cholestasis. Am J Med 114:62–64
Parés A, Cisneros L, Salmerón JM, Caballería L, Mas A, Torras A, Rodés J (2004) Extracorporeal albumin dialysis: a procedure for prolonged relief of intractable pruritus in patients with primary biliary cirrhosis. Am J Gastroenterol 99:1105–1110
Bellmann R, Graziadei IW, Feistritzer C, Schwaighofer H, Stellaard F, Sturm E, Wiedermann CJ, Joannidis M (2004) Treatment of refractory cholestatic pruritus after liver transplantation with albumin dialysis. Liver Transpl Off Publ Am Assoc Study Liver Dis Int Liver Transpl Soc 10:107–114
Lemoine M, Revaux A, Francoz C, Ducarme G, Brechignac S, Jacquemin E, Uzan M, Ganne-Carrie N (2008) Albumin liver dialysis as pregnancy-saving procedure in cholestatic liver disease and intractable pruritus. World J Gastroenterol 14:6572–6574
Javouhey E, Ranchin B, Lachaux A, Boillot O, Martin X, Floret D, Cochat P (2009) Long-lasting extracorporeal albumin dialysis in a child with end-stage renal disease and severe cholestasis. Pediatr Transplant 13:235–239
Schaefer B, Schaefer F, Wittmer D, Engelmann G, Wenning D, Schmitt CP (2012) Molecular Adsorbents Recirculating System dialysis in children with cholestatic pruritus. Pediatr Nephrol 27:829–834
Horvatits T, Drolz A, Trauner M, Fuhrmann V (2019) Liver injury and failure in critical illness. Hepatology 70:2204–2215
Drolz A, Horvatits T, Roedl K, Rutter K, Staufer K, Haider DG, Zauner C, Heinz G, Schellongowski P, Kluge S, Trauner M, Fuhrmann V (2016) Outcome and features of acute kidney injury complicating hypoxic hepatitis at the medical intensive care unit. Ann Intensive Care 6:61
Drolz A, Saxa R, Scherzer T, Fuhrmann V (2011) Extracorporeal artificial liver support in hypoxic liver injury. Liver Int Off J Int Assoc Study Liver 31(Suppl 3):19–23
El Banayosy A, Kizner L, Schueler V, Bergmeier S, Cobaugh D, Koerfer R (2004) First use of the Molecular Adsorbent Recirculating System technique on patients with hypoxic liver failure after cardiogenic shock. ASAIO J 50:332–337
Fuhrmann V, Herkner H, Roedl K, Drolz A, Horvatits T, Horvatits K, Jarczak D, Zauner C, Schellongowski P, Heinz G, Trauner M, Kluge S (2019) Behandlung von sekundärem Leberversagen mit dem MARS®-System - eine randomisiert-kontrollierte Studie. In: Editor (ed)^(eds) Book Behandlung von sekundärem Leberversagen mit dem MARS®-System - eine randomisiert-kontrollierte Studie. City, pp 11–12
van Mierlo KM, Schaap FG, Dejong CH, Olde Damink SW (2016) Liver resection for cancer: new developments in prediction, prevention and management of postresectional liver failure. J Hepatol 65:1217–1231
Catalina MV, Barrio J, Anaya F, Salcedo M, Rincon D, Clemente G, Banares R (2003) Hepatic and systemic haemodynamic changes after MARS in patients with acute on chronic liver failure. Liver Int Off J Int Assoc Study Liver 23(Suppl 3):39–43
Sen S, Mookerjee RP, Cheshire LM, Davies NA, Williams R, Jalan R (2005) Albumin dialysis reduces portal pressure acutely in patients with severe alcoholic hepatitis. J Hepatol 43:142–148
Stadlbauer V, Krisper P, Aigner R, Haditsch B, Jung A, Lackner C, Stauber RE (2006) Effect of extracorporeal liver support by MARS and Prometheus on serum cytokines in acute-on-chronic liver failure. Crit Care 10:R169
Gilg (2016) Albumin dialysis with mars in post-hepatectomy liver failure (PHLF): experiences from two HPB centers. Surg Curr Res 6: 252:1–6
Gilg S, Sparrelid E, Saraste L, Nowak G, Wahlin S, Strömberg C, Lundell L, Isaksson B (2018) The molecular adsorbent recirculating system in posthepatectomy liver failure: results from a prospective phase I study. Hepatol Commun 2:445–454
Balzan S, Belghiti J, Farges O, Ogata S, Sauvanet A, Delefosse D, Durand F (2005) The “50-50 criteria” on postoperative day 5: an accurate predictor of liver failure and death after hepatectomy. Ann Surg 242:824–828
Sparrelid E, Gilg S, van Gulik TM (2020) Systematic review of MARS treatment in post-hepatectomy liver failure. HPB (Oxf) 22:950–960
Beyls C, Malaquin S, Huette P, Mary A, Besserve P, Roger PA, Bernasinski M, Guilbart M, Abou-Arab O, Dupont H, Mahjoub Y (2021) Hemodynamic impact of molecular adsorbent recirculating system in refractory vasoplegic shock due to calcium channel blocker poisoning. Int J Artif Organs 44(12):944–951
Pichon N, Dugard A, Clavel M, Amiel JB, François B, Vignon P (2012) Extracorporeal albumin dialysis in three cases of acute calcium channel blocker poisoning with life-threatening refractory cardiogenic shock. Ann Emerg Med 59:540–544
Hassoun J, Hammer N, Magini G, Ponte B, Ongaro M, Rougemont AL, Goossens N, Frossard JL, Spahr L (2021) Management of acute Wilsonian hepatitis with severe hemolysis: a successful combination of chelation and MARS dialysis. Case Rep Hepatol 2021:5583654
Faybik P, Hetz H, Baker A, Bittermann C, Berlakovich G, Werba A, Krenn CG, Steltzer H (2003) Extracorporeal albumin dialysis in patients with Amanita phalloides poisoning. Liver Int Off J Int Assoc Study Liver 23(Suppl 3):28–33
De Bruyn T, Meijers B, Evenepoel P, Laub R, Willems L, Augustijns P, Annaert P (2012) Stability of therapeutic albumin solutions used for molecular adsorbent recirculating system-based liver dialysis. Artif Organs 36:29–41
Krisper P, Tiran B, Fliser D, Haditsch B, Stadlbauer V, Otto R, Ernst T, Kretschmer U, Stauber RE, Haller H, Holzer H, Manns MP, Rifai K (2010) Efficacy and safety of anticoagulation with heparin versus heparin plus epoprostenol in patients undergoing extracorporeal liver support with Prometheus. Artif Organs 34:84–88
Tan HK, Yang WS, Chow P, Lui HF, Choong HL, Wong KS (2007) Anticoagulation minimization is safe and effective in albumin liver dialysis using the molecular adsorbent recirculating system. Artif Organs 31:193–199
Faybik P, Hetz H, Mitterer G, Krenn CG, Schiefer J, Funk GC, Bacher A (2011) Regional citrate anticoagulation in patients with liver failure supported by a molecular adsorbent recirculating system. Crit Care Med 39:273–279
Meijers B, Laleman W, Vermeersch P, Nevens F, Wilmer A, Evenepoel P (2012) A prospective randomized open-label crossover trial of regional citrate anticoagulation vs. anticoagulation free liver dialysis by the Molecular Adsorbents Recirculating System. Crit Care (Lond, Engl) 16:R20
Tan HK (2004) Molecular adsorbent recirculating system (MARS). Ann Acad Med Singap 33:329–335
Sponholz C, Matthes K, Rupp D, Backaus W, Klammt S, Karailieva D, Bauschke A, Settmacher U, Kohl M, Clemens MG, Mitzner S, Bauer M, Kortgen A (2016) Molecular adsorbent recirculating system and single-pass albumin dialysis in liver failure—a prospective, randomised crossover study. Crit Care (Lond, Engl) 20:2
Dyla A, Mielnicki W, Bartczak J, Zawada T, Garba P (2017) Effectiveness and safety assessment of citrate anticoagulation during albumin dialysis in comparison to other methods of anticoagulation. Artif Organs 41:818–826
Thai C, Oben C, Wagener G (2020) Coagulation, hemostasis, and transfusion during liver transplantation. Best Pract Res Clin Anaesthesiol 34:79–87
Evenepoel P, Laleman W, Wilmer A, Claes K, Kuypers D, Bammens B, Nevens F, Vanrenterghem Y (2006) Prometheus versus molecular adsorbents recirculating system: comparison of efficiency in two different liver detoxification devices. Artif Organs 30:276–284
Schneider AG, Journois D, Rimmelé T (2017) Complications of regional citrate anticoagulation: accumulation or overload? Crit Care (Lond, Engl) 21:281
Weiler S, Vogelsinger H, Joannidis M, Dunzendorfer S, Bellmann R (2011) Influence of albumin dialysis on pharmacokinetics of amphotericin B colloidal dispersion and amphotericin B lipid complex. Artif Organs 35:667–671
Aguilar G, Azanza JR, Sádaba B, Badenes R, Ferrando C, Delgado C, Hernández J, Parra MA, Puig J, Carbonell JA, Navarro D, Belda FJ (2014) Pharmacokinetics of anidulafungin during albumin dialysis. Crit Care (Lond, Engl) 18:422
Personett HA, Larson SL, Frazee EN, Nyberg SL, El-Zoghby ZM (2015) Extracorporeal elimination of piperacillin/tazobactam during molecular adsorbent recirculating system therapy. Pharmacotherapy 35:e136-139
Ruggero MA, Argento AC, Heavner MS, Topal JE (2013) Molecular Adsorbent Recirculating System (MARS(®)) removal of piperacillin/tazobactam in a patient with acetaminophen-induced acute liver failure. Transpl Infect Dis Off J Transplant Soc 15:214–218
Personett HA, Larson SL, Frazee EN, Nyberg SL, Leung N, El-Zoghby ZM (2014) Impact of molecular adsorbent recirculating system therapy on tacrolimus elimination: a case report. Transplant Proc 46:2440–2442
Falkensteiner C, Kortgen A, Leonhardt J, Bauer M, Sponholz C (2021) Comparison of albumin dialysis devices molecular adsorbent recirculating system and ADVanced Organ Support system in critically ill patients with liver failure—a retrospective analysis. Ther Apher Dial Off Peer-Rev J Int Soc Apher Jpn Soc Apher Jpn Soc Dial Ther 25:225–236
Fuhrmann V, Weber T, Roedl K, Motaabbed J, Tariparast A, Jarczak D, de Garibay APR, Kluwe J, Boenisch O, Herkner H, Kellum JA, Kluge S (2020) Advanced organ support (ADVOS) in the critically ill: first clinical experience in patients with multiple organ failure. Ann Intensive Care 10:96
Tan EX, Wang MX, Pang J, Lee GH (2020) Plasma exchange in patients with acute and acute-on-chronic liver failure: a systematic review. World J Gastroenterol 26:219–245
Schmidt LE, Wang LP, Hansen BA, Larsen FS (2003) Systemic hemodynamic effects of treatment with the molecular adsorbents recirculating system in patients with hyperacute liver failure: a prospective controlled trial. Liver Transpl Off Publ Am Assoc Study Liver Dis Int Liver Transpl Soc 9:290–297
Novelli G, Rossi M, Pretagostini M, Pugliese F, Ruberto F, Novelli L, Nudo F, Bussotti A, Corradini S, Martelli S, Berloco PB (2005) One hundred sixteen cases of acute liver failure treated with MARS. Transplant Proc 37:2557–2559
El Banayosy A, Cobaugh D, Pauly A, Kizner L, Korfer R (2007) Albumindialyse bei patienten mit sekundärem leberversagen nach kariogenem schock. Intensivemed 44:149–157
Gerth HU, Pohlen M, Thölking G, Pavenstädt H, Brand M, Hüsing-Kabar A, Wilms C, Maschmeier M, Kabar I, Torner J, Pavesi M, Arroyo V, Banares R, Schmidt HHJ (2017) Molecular adsorbent recirculating system can reduce short-term mortality among patients with acute-on-chronic liver failure—a retrospective analysis. Crit Care Med 45:1616–1624
Acknowledgements
The authors are grateful to Bruno Trumbic, MD (Paris, France) for assistance in assembling the manuscript. A special dedication to Roger Williams CBE, for his great devotion to liver research and his contribution and inspiration to the development of devices for liver support therapy.
Funding
The study was part of an Investigator-Initiated Research (IIR) Grant Program from Baxter International Inc. Baxter® was not involved in the conception of the study, the expert’s selection and drafting of the manuscript.
Author information
Authors and Affiliations
Contributions
FS, SJ and JT appointed the expert panel, organized the meetings and coordinated the panel group, drafted and wrote the final version of the manuscript. All authors participated individually to the draft writing, the consensus and approved the statements and final version of the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
FS has received speaker’s honoraria and/or research grants from Novartis, Astellas, Chiesi, Gilead, Merck Sharp and Dohme, Neovie, Biotest and Baxter. RB has received speaker’s honoraria and/or research grants from Gilead, abbvie, Janssen, Gore Baxter. FL has nothing to declare. AW has no conflict of interest. AP has received grant funding, personal fees, and advisory board fees from Intercept Pharmaceuticals and Genfit; advisory board fees and fees for teaching from Novartis; and personal fees from CymaBay Therapeutics and Inova Diagnostics. SM has received speaker`s honoraria and/or research grants from Amgen, Astellas, Baxter, BMS/Pfizer, CytoSorbents, Pentracor, Vifor. JS is chairman of the board of Albutec GmbH. VF declare presentations for Fresenius, Baxter, ADVITOS, CSL-Behring, Merz, Advisory board. SG declare no conflict of interest. TH is consultant for DIALIVE. On advisory committee and received consultancy from AbbVie, Bristol-Myers Squibb, Gilead, Malinckrodt, Merck, and Organovo. Received research grants from AbbVie, Allergan, Amarex/Cytodyn, Astra Zeneca, Boehringer-Ingelheim, Bristol-Myers Squibb, CARA, DURECT Corporation, Enanta, Galectin, Gilead, Grifols, Intercept, Merck, Mirum, Novartis, Novo Nordisk, Pfizer, Salix Pharmaceuticals, Sonic Incytes, and Terns Pharmaceuticals. DS received research grants Astellas and honoraria from Goliver and Biotest. JT, declare no conflict of interest. JT declares no conflict of interest. SJ declares consulting fees from Drager, Fresenius-Xenios, Medtronic, Mindray and Fisher & Paykel.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
134_2022_6802_MOESM1_ESM.pdf
Supplemental figure 1. Molecular structure of human serum albumin and binding sites (adapted from Bernardi M. et al [9]). (PDF 2047 kb)
Rights and permissions
About this article
Cite this article
Saliba, F., Bañares, R., Larsen, F.S. et al. Artificial liver support in patients with liver failure: a modified DELPHI consensus of international experts. Intensive Care Med 48, 1352–1367 (2022). https://doi.org/10.1007/s00134-022-06802-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-022-06802-1