Abstract
Purpose
We previously showed that external cooling decreases day 14 mortality in febrile septic shock. Because cooling may participate in heart rate control, we studied the respective impact of heart rate and temperature lowering on mortality.
Methods
Post hoc analysis of the Sepsiscool randomized controlled trial database (NCT00527007). Cooling was applied to maintain normothermia (36.5–37 °C) during 48 h. We assessed the time spent below different thresholds of temperature and heart rate on day 14 mortality. The best threshold was selected by AUC-ROC and tested as a potential mediator of mortality reduction. Mediation analysis was adjusted for severity and treatments influencing temperature and heart rate evolution. Sensitivity analysis was done using only patients with appropriate antimicrobial therapy.
Results
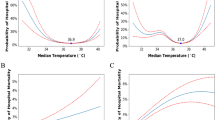
A total of 197/200 patients with adequate heart rate and temperature monitoring were analyzed. The best threshold differentiating survivors and nonsurvivors was 38.4 °C for temperature and 95 b/min for heart rate. During the 48 h of intervention, cooling significantly increased the time spent with a temperature below 38.4 °C, p = 0.001, and with a heart rate below 95 b/min, p < 0.01. The longer was the time spent with a temperature below 38.4 °C, the lower was the mortality [adjOR 0.17 (0.06–0.49), p = 0.001]. The time spent with a heart rate below 95 b/min was similar in survivors and nonsurvivors [adjOR 0.68 (0.27–1.72), p = 0.42]. Mediation analysis showed that the time spent with a temperature below 38.4 °C was a significant mediator of mortality.
Conclusion
The time spent with a temperature below 38.4 °C was independently associated with patient’s outcome and explained 73 % of the effect of the randomization on the day 14 mortality. Heart rate lowering was not a mediator of mortality.



Similar content being viewed by others
References
Barie PS, Hydo LJ, Eachempati SR (2004) Causes and consequences of fever complicating critical surgical illness. Surg Infect 5:145–159
Kiekkas P, Velissaris D, Karanikolas M, Aretha D, Samios A, Skartsani C, Baltopoulos GI, Filos KS (2009) Peak body temperature predicts mortality in critically ill patients without cerebral damage. Heart Lung 39:208–216
Selladurai S, Eastwood GM, Bailey M, Bellomo R (2011) Paracetamol therapy for septic critically ill patients: a retrospective observational study. Crit Care Resusc 13:181–186
Laupland KB, Zahar JR, Adrie C, Schwebel C, Goldgran-Toledano D, Azoulay E, Garrouste-Orgeas M, Cohen Y, Jamali S, Souweine B, Darmon M, Timsit JF (2012) Determinants of temperature abnormalities and influence on outcome of critical illness. Crit Care Med 40:145–151
Kushimoto S, Gando S, Saitoh D, Mayumi T, Ogura H, Fujishima S, Araki T, Ikeda H, Kotani J, Miki Y, Shiraishi SI, Suzuki K, Suzuki Y, Takeyama N, Takuma K, Tsuruta R, Yamaguchi Y, Yamashita N, Aikawa N (2013) The impact of body temperature abnormalities on the disease severity and outcome in patients with severe sepsis: an analysis from a multicenter, prospective survey of severe sepsis. Crit Care 17:R271
Fever and Antipyretic in Critically ill patients Evaluation (FACE) Study Group, Lee BH, Inui D, Suh GY, Kim JY, Kwon JY, Park J, Tada K, Tanaka K, Ietsugu K, Uehara K, Dote K, Tajimi K, Morita K, Matsuo K, Hoshino K, Hosokawa K, Lee KH, Lee KM, Takatori M, Nishimura M, Sanui M, Ito M, Egi M, Honda N, Okayama N, Shime N, Tsuruta R, Nogami S, Yoon SH, Fujitani S, Koh SO, Takeda S, Saito S, Hong SJ, Yamamoto T, Yokoyama T, Yamaguchi T, Nishiyama T, Igarashi T, Kakihana Y, Koh Y (2012) Association of body temperature and antipyretic treatments with mortality of critically ill patients with and without sepsis: multi-centered prospective observational study. Crit Care 16:R33
Young PJ, Saxena M, Beasley R, Bellomo R, Bailey M, Pilcher D, Finfer S, Harrison D, Myburgh J, Rowan K (2012) Early peak temperature and mortality in critically ill patients with or without infection. Intensive Care Med 38:437–444
Manthous CA, Hall JB, Olson D, Singh M, Chatila W, Pohlman A, Kushner R, Schmidt GA, Wood LD (1995) Effect of cooling on oxygen consumption in febrile critically ill patients. Am J Respir Crit Care Med 151:10–14
Bernard GR, Wheeler AP, Russell JA, Schein R, Summer WR, Steinberg KP, Fulkerson WJ, Wright PE, Christman BW, Dupont WD, Higgins SB, Swindell BB (1997) The effects of ibuprofen on the physiology and survival of patients with sepsis. The Ibuprofen in Sepsis Study Group. N Engl J Med 336:912–918
Gozzoli V, Treggiari MM, Kleger GR, Roux-Lombard P, Fathi M, Pichard C, Romand JA (2004) Randomized trial of the effect of antipyresis by metamizol, propacetamol or external cooling on metabolism, hemodynamics and inflammatory response. Intensive Care Med 30:401–407
Taccone FS, Saxena M, Schortgen F (2014) What’s new with fever control in the ICU. Intensive Care Med 40:1147–1150
Nakamura K (2011) Central circuitries for body temperature regulation and fever. Am J Physiol Regul Integr Comp Physiol 301:R1207–R1228
Russell JA (2012) Control of fever in septic shock: should we care or intervene? Am J Respir Crit Care Med 185:1040–1041
Dunser MW, Hasibeder WR (2009) Sympathetic overstimulation during critical illness: adverse effects of adrenergic stress. J Intensive Care Med 24:293–316
Nalivaiko E (2006) Tachycardia during fever: is it neural or humoral? Am J Physiol Regul Integr Comp Physiol 290:R1750
Takayama K, Yuhki K, Ono K, Fujino T, Hara A, Yamada T, Kuriyama S, Karibe H, Okada Y, Takahata O, Taniguchi T, Iijima T, Iwasaki H, Narumiya S, Ushikubi F (2005) Thromboxane A2 and prostaglandin F2alpha mediate inflammatory tachycardia. Nat Med 11:562–566
Magder SA (2012) The ups and downs of heart rate. Crit Care Med 40:239–245
Aboab J, Sebille V, Jourdain M, Mangalaboyi J, Gharbi M, Mansart A, Annane D (2011) Effects of esmolol on systemic and pulmonary hemodynamics and on oxygenation in pigs with hypodynamic endotoxin shock. Intensive Care Med 37:1344–1351
Morelli A, Ertmer C, Westphal M, Rehberg S, Kampmeier T, Ligges S, Orecchioni A, D’Egidio A, D’Ippoliti F, Raffone C, Venditti M, Guarracino F, Girardis M, Tritapepe L, Pietropaoli P, Mebazaa A, Singer M (2013) Effect of heart rate control with esmolol on hemodynamic and clinical outcomes in patients with septic shock: a randomized clinical trial. JAMA 310:1683–1691
Schortgen F, Clabault K, Katsahian S, Devaquet J, Mercat A, Deye N, Dellamonica J, Bouadma L, Cook F, Beji O, Brun-Buisson C, Lemaire F, Brochard L (2012) Fever control using external cooling in septic shock: a randomized controlled trial. Am J Respir Crit Care Med 185:1088–1095
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A, Bruining H, Reinhart CK, Suter PM, Thijs LG (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 22:707–710
Moreno RP, Metnitz PG, Almeida E, Jordan B, Bauer P, Campos RA, Iapichino G, Edbrooke D, Capuzzo M, Le Gall JR (2005) SAPS 3—from evaluation of the patient to evaluation of the intensive care unit. Part 2: development of a prognostic model for hospital mortality at ICU admission. Intensive Care Med 31:1345–1355
Poukkanen M, Wilkman E, Vaara ST, Pettila V, Kaukonen KM, Korhonen AM, Uusaro A, Hovilehto S, Inkinen O, Laru-Sompa R, Hautamaki R, Kuitunen A, Karlsson S (2013) Hemodynamic variables and progression of acute kidney injury in critically ill patients with severe sepsis: data from the prospective observational FINNAKI study. Crit Care 17:R295
Amato MB, Meade MO, Slutsky AS, Brochard L, Costa EL, Schoenfeld DA, Stewart TE, Briel M, Talmor D, Mercat A, Richard JC, Carvalho CR, Brower RG (2015) Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med 372:747–755
Imai K, Keele L, Tingley D (2010) A general approach to causal mediation analysis. Psychol Methods 15:309–334
Tingley D, Yamamoto T, Hirose K, Keele L, Imai K (2014) Mediation: R package for causal mediation analysis. J Stat Softw 59:1–38
Poblete B, Romand JA, Pichard C, Konig P, Suter PM (1997) Metabolic effects of i.v. propacetamol, metamizol or external cooling in critically ill febrile sedated patients. Br J Anaesth 78:123–127
Mohr NM, Fuller BM, Skrupky LP, Moy H, Alunday R, Micek ST, Fagley RE (2011) Clinical and demographic factors associated with antipyretic use in gram-negative severe sepsis and septic shock. Ann Pharmacother 45:1207–1216
Niven D, Laupland K, Tabah A, Vesin A, Rello J, Koulenti D, Dimopoulos G, de Waele J, Timsit JF (2013) Diagnosis and management of temperature abnormality in ICUs: a EUROBACT investigators survey. Crit Care 17:R289
O’Grady NP, Barie PS, Bartlett JG, Bleck T, Carroll K, Kalil AC, Linden P, Maki DG, Nierman D, Pasculle W, Masur H (2008) Guidelines for evaluation of new fever in critically ill adult patients: 2008 update from the American College of Critical Care Medicine and the Infectious Diseases Society of America. Crit Care Med 36:1330–1349
Schortgen F (2012) Fever in sepsis. Minerva Anestesiol 78:1254–1264
Seguin P, Roquilly A, Mimoz O, Maguet PL, Asehnoune K, Biederman S, Carise E, Malledant Y (2012) Risk factors and outcomes for prolonged versus brief fever: a prospective cohort study. Crit Care 16:R150
Parker MM, Shelhamer JH, Natanson C, Alling DW, Parrillo JE (1987) Serial cardiovascular variables in survivors and nonsurvivors of human septic shock: heart rate as an early predictor of prognosis. Crit Care Med 15:923–929
Raby KE, Brull SJ, Timimi F, Akhtar S, Rosenbaum S, Naimi C, Whittemore AD (1999) The effect of heart rate control on myocardial ischemia among high-risk patients after vascular surgery. Anesth Analg 88:477–482
Benchekroune S, Karpati PC, Berton C, Nathan C, Mateo J, Chaara M, Riche F, Laisne MJ, Payen D, Mebazaa A (2008) Diastolic arterial blood pressure: a reliable early predictor of survival in human septic shock. J Trauma 64:1188–1195
Leibovici L, Gafter-Gvili A, Paul M, Almanasreh N, Tacconelli E, Andreassen S, Nielsen AD, Frank U, Cauda R, Group TS (2007) Relative tachycardia in patients with sepsis: an independent risk factor for mortality. QJM 100:629–634
Azimi G, Vincent JL (1986) Ultimate survival from septic shock. Resuscitation 14:245–253
Groeneveld AB, Nauta JJ, Thijs LG (1988) Peripheral vascular resistance in septic shock: its relation to outcome. Intensive Care Med 14:141–147
Mourvillier B, Tubach F, van de Beek D, Garot D, Pichon N, Georges H, Lefevre LM, Bollaert PE, Boulain T, Luis D, Cariou A, Girardie P, Chelha R, Megarbane B, Delahaye A, Chalumeau-Lemoine L, Legriel S, Beuret P, Brivet F, Bruel C, Camou F, Chatellier D, Chillet P, Clair B, Constantin JM, Duguet A, Galliot R, Bayle F, Hyvernat H, Ouchenir K, Plantefeve G, Quenot JP, Richecoeur J, Schwebel C, Sirodot M, Esposito-Farese M, Le Tulzo Y, Wolff M (2013) Induced hypothermia in severe bacterial meningitis: a randomized clinical trial. JAMA 310:2174–2183
Saxena M, Young P, Pilcher D, Bailey M, Harrison D, Bellomo R, Finfer S, Beasley R, Hyam J, Menon D, Rowan K, Myburgh J (2015) Early temperature and mortality in critically ill patients with acute neurological diseases: trauma and stroke differ from infection. Intensive Care Med 41:823–832
Staer-Jensen H, Sunde K, Olasveengen TM, Jacobsen D, Draegni T, Nakstad ER, Eritsland J, Andersen GO (2014) Bradycardia during therapeutic hypothermia is associated with good neurologic outcome in comatose survivors of out-of-hospital cardiac arrest. Crit Care Med 42:2401–2408
Acknowledgment
This study was funded by The Assistance Publique-Hôpitaux de Paris, France. The sponsor participated in the study organization and monitoring but had no access to the data.
Sepsis Cool Investigators
Karine Clabault: Réanimation médicale CHU de Rouen, France.
Fabrice Cook: AP-HP, Groupe Hospitalier Henri Mondor, réanimation chirurgicale, Créteil, France.
Jean Dellamonica: Réanimation médicale CHU de Nice, France.
Jerome Devaquet: Réanimation polyvalente Hôpital Foch, Suresnes, France.
Nicolas Deye: APHP, Hôpital Lariboisière, réanimation médicale et toxicologique, Paris, France.
Alain Mercat: Réanimation médicale CHU Angers, France.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Dr. Brochard’s laboratory has received research grant from Dräger (SmartCare), Covidien (PAV), General Electric (lung volume), Fisher Paykel (high flow oxygen), and Vygon (CPAP), educational grant from General Electric, and personal fees from Covidien (PAV). St Michael’s Hospital in Toronto is receiving royalties from Maquet (NAVA). Dr. Katsahian consulted for La générale de santé. The remaining authors have no conflict of interest.
Additional information
For the Sepsis Cool Investigators. The remaining members of the Sepsis Cool Investigators are listed at the end of the article.
Rights and permissions
About this article
Cite this article
Schortgen, F., Charles-Nelson, A., Bouadma, L. et al. Respective impact of lowering body temperature and heart rate on mortality in septic shock: mediation analysis of a randomized trial. Intensive Care Med 41, 1800–1808 (2015). https://doi.org/10.1007/s00134-015-3987-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-015-3987-7