Abstract
Purpose
To compare survival, oxygenation, ventilation, and hemodynamic variables achieved with chest compressions or ventilation plus chest compressions.
Methods
This randomized experimental study was conducted in the experimental department of a university hospital. Thirty infant pigs with asphyxial cardiac arrest were randomized into two groups of cardiopulmonary resuscitation (CPR): group 1, continuous chest compressions plus non-coordinated ventilation with a mask and mechanical ventilator (inspired oxygen fraction 0.21) (VC); group 2, chest compressions only (CC). Nine minutes of basic resuscitation was performed initially in both groups, followed by advanced resuscitation. CPR was terminated on achieving return of spontaneous circulation (ROSC) or after 30 min of total resuscitation time without ROSC.
Results
Three animals (18.8%) in the VC group and 1 (7.1%) in the CC group achieved ROSC (P = 0.351). Oxygenation and ventilation during basic CPR were insufficient in both groups, though they were significantly better in the VC group than in the CC group after 9 min (PaO2, 26 vs. 19 mmHg, P = 0.008; PaCO2, 84 vs. 101 mmHg, P = 0.05). Cerebral saturation was higher in the VC group (61%) than in the CC group (30%) (P = 0.06). There were no significant differences in mean arterial pressure.
Conclusions
Neither of the basic CPR protocols achieved adequate oxygenation and ventilation in this model of asphyxial pediatric cardiac arrest. Chest compressions plus ventilation produced better oxygenation, ventilation, and cerebral oxygenation with no negative hemodynamic effects. Survival was higher in the VC group, though the difference was not statistically significant.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years, several clinical studies have found that compression-only cardiopulmonary resuscitation (CPR) can achieve better survival and neurological outcome than compression plus ventilation in adult cardiac arrest (CA) of cardiac origin, particularly in ventricular fibrillation, and in out-of-hospital CA [1–5]. Moreover, some experimental studies of CA secondary to ventricular fibrillation have found a similar rate of recovery and a better neurological prognosis in animals that received chest compressions only (CC) in comparison with those that were resuscitated with the standard technique of ventilation plus chest compressions (VC) [6–11]. With CC resuscitation, the absence of interruptions of chest compressions would optimize the perfusion of vital organs and hyperventilation would be avoided.
These findings, together with the fact that some citizens are unwilling to perform mouth-to-mouth ventilation on adults [5] and that learning compression-only CPR is easier than compression plus ventilation, have led to a proposal to change the international guidelines for bystander-initiated CPR.
However, some studies have reported a higher survival with VC than with CC CPR in out-of-hospital CA of noncardiac origin in adults [12] and children [13].
In pediatric patients, CA is very often of asphyxial origin and, in contrast to the situation with ventricular fibrillation, the blood flow is maintained for a certain time before cardiac activity ceases, reducing the arterial and venous oxygen tension and increasing the CO2 tension. For this reason the importance of ventilation in pediatric CA may differ from that in adult CA [5].
The aim of our study was to compare survival and the oxygenation and ventilation parameters with CC and VC resuscitation in an infant animal model of asphyxial CA. Our hypothesis was that CPR by continuous chest compressions plus non-coordinated ventilation (VC) achieves better oxygenation and ventilation than compression-only CPR (CC) with no hemodynamic repercussions; a higher percentage of return of spontaneous circulation (ROSC) would therefore be achieved with VC resuscitation than with CC resuscitation.
Methods
A randomized study was performed on 30 2-month-old Maryland pigs with a mean (SD) weight of 9.5 (2.4) kg. The experimental protocol was approved by the local institutional ethical animal investigation committee. International guidelines for the care of experimental animals were applied. The animals were intubated and connected to a mechanical ventilator (Drager SA2, Lubeck, Germany) with a respiratory rate of 20 breaths/min (bpm), tidal volume of 10 ml/kg, fraction of inspired oxygen (FiO2) of 50%, and positive end-expiratory pressure of 3 cm H2O. Sedation and relaxation (propofol 10 mg/kg/h, fentanyl 10 mg/kg/h, and atracurium 2 mg/kg/h as a continuous infusion) were maintained throughout the procedure, inhibiting the presence of agonal breathing. Continuous monitoring was performed of the electrocardiogram (ECG), peripheral oxygen saturation (Visconnet® monitor, KGB Madrid, Spain), cerebral and renal saturation (INVOS® Cerebral Oximeter monitor, Somanetics, Troy, Mi, USA), and the respiratory volumes and pressures, FiO2, and end-tidal carbon dioxide (EtCO2) via a spirometer connected to the endotracheal tube and an S5® monitor (Datex Ohmeda, Madison, USA) with a volume detection capacity of 7 ml. A 4-F PiCCO® catheter was inserted into the femoral artery to measure the blood pressure and cardiac output by means of a femoral arterial thermodilution system (PiCCO®, Pulsion Medical Systems, Munich, Germany). A 5.5-F catheter was inserted through the femoral vein to measure the central venous pressure (CVP). Blood gases were analyzed using the GEM Premier 3000® blood gas analyzer (Instrumentation Laboratory, Lexington, USA).
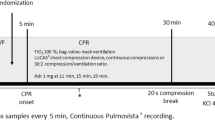
Figure 1 shows the experimental protocol. Cardiac arrest was induced by disconnection from the ventilator and extubation for at least 10 min. Basic resuscitation was started after confirming the absence of signs of spontaneous circulation [absent pulse and mean arterial pressure (MAP) less than 25 mmHg].
The animals were randomly distributed into two groups: in group 1, resuscitation was started with manual chest compressions (100 compressions/min) and ventilation via a face mask (20 bpm, tidal volume 10 ml/kg, FiO2 0.21, using the respirator and without interruption of chest compressions) (VC); in group 2, only chest compressions (CC) were performed. The number of chest compressions was controlled continuously using the arterial blood pressure and ECG monitor.
After 9 min of basic resuscitation, advanced resuscitation with intubation and mechanical ventilation with an FiO2 of 1 and the administration of 0.02 mg/kg of epinephrine every 3 min were started in both groups. Advanced CPR was terminated if ROSC was achieved or after 30 min of total resuscitation time without ROSC.
After ROSC, mechanical ventilation was continued for 20 min with 100% oxygen and adjusted to obtain a PaCO2 between 35 and 45 mmHg (4.7–6 kPa). On completion of the experiment, all successfully resuscitated animals were killed by the administration of sedative overdose and the intravenous injection of potassium chloride.
The following parameters were recorded at baseline and every 3 min during the experiment: ECG rhythm, heart rate (HR), mean arterial pressure, CVP, cardiac index (CI), inspiratory tidal volume (TV), EtCO2, and peripheral, cerebral, and renal oxygen saturations. Arterial and venous blood gases and lactate measurements were recorded at baseline and every 6 min. Cardiac index was determined before cardiac arrest, during resuscitation, and when ROSC was achieved. During chest compressions it was not possible to calibrate the thermodilution PICCO method and CI was only measured by analysis of the pulse contour curve.
The statistical analysis was performed using the SPSS statistical package, version 16.0. Variables with a normal distribution were compared using the t test, the χ 2 test, and the Fisher test; the Friedman and Mann–Whitney U tests were used when nonparametric tests were required. A P value of less than 0.05 was considered statistically significant.
Results
Sixteen pigs were randomized to group 1, VCs, and 14 to group 2, CCs only. There were no significant differences between the two groups regarding arrest rhythms, hemodynamic, respiratory, and perfusion parameters, or blood gas profiles at the time of disconnection from the respirator or 10 min after disconnection (Table 1).
There were no significant differences in the hemodynamic parameters MAP, CVP, and CI between the two techniques during basic and advanced life support (Fig. 2).
During basic CPR the animals in the VC group presented lower PaCO2 figures that the CC group (Fig. 3). However, adequate ventilation was not achieved in any of the animals. During advanced resuscitation, after intubation, there was a progressive improvement in the ventilation in both groups, although normal ventilation was not achieved despite a tidal volume of 10 ml/kg and a respiratory rate of 20 rpm. During advanced resuscitation, the PaCO2 remained lower in the VC group, though the difference was not statistically significant (Fig. 3).
During basic CPR, the PaO2 and arterial saturation were higher in the VC group than in the CC group despite ventilation with an FiO2 of 0.21 (Figs. 4, 5). During advanced CPR after endotracheal intubation, both groups showed a progressive improvement in oxygenation, without reaching normal values; the difference between the two groups was not significant.
The animals in the VC group presented greater cerebral oxygenation during basic resuscitation although the differences did not reach statistical significance (Fig. 6). Cerebral oxygenation improved in both groups during advanced resuscitation, though normal values were not reached.
There were no differences in central venous saturation, arterial pH, or lactic acid concentration between the two groups at any time in the course of the experiment. Table 2 shows the comparison of parameters between the two groups at the end of basic resuscitation and at the end of advanced resuscitation.
Recovery of spontaneous circulation was only achieved in 4 of the 30 animals (13.3%): 3 (18.8%) in the VC group and 1 (7.1%) in the CC group. This difference did not reach statistical significance (P = 0.351). There were no differences in baseline parameters at the start of resuscitation between the animals that achieved ROSC and those that did not. The four animals that achieved ROSC remained stable in the subsequent 20-min observation period.
Discussion
A number of observational studies in adults [1–4] and in children [13] have compared the clinical course of patients resuscitated using cardiac compressions only to that of those who received compressions and ventilation. Some studies in adults showed that the exclusive use of compressions during basic CPR was associated with a survival equal to or greater than CPR with compressions and ventilation and was easier to perform [1–4, 14]. For this reason, the 2010 American Heart Association guidelines recommend that, following initial assessment, rescuers of adult patients start CPR with chest compressions before opening the airway and delivering rescue breaths, and chest compressions alone are recommended for untrained lay persons responding to victims of cardiac arrest. Performing chest compressions alone is reasonable for trained lay persons if they are unable to perform airway and breathing maneuvers [15].
On the other hand, a recent study in children showed that survival among patients over 1 year of age who suffered cardiac arrest of probable noncardiac origin was greater in those who received compressions plus ventilation compared to compression-only CPR [13]. However, there are no randomized clinical trials in adults or children that have compared the two techniques, and there are only observational studies and reviews [16–18].
Our study compares the effect of CPR with compressions and ventilation versus compressions alone on oxygenation, ventilation, and survival in an infant animal model of hypoxic cardiac arrest. We avoided gasping by administration of a paralyzing agent and permitted passive ventilation in compression-only CPR. Other studies have produced cardiac arrest by endotracheal tube clamping simulating an obstructed airway [19, 20] that does not permit passive ventilation in compression-only CPR or by inducing ventricular fibrillation [6, 7, 21, 22].
In our study the survival was higher in the group with chest compressions plus ventilation. However, the difference was not significant due, at least in part, to the small sample size. The low overall rate of resuscitation was probably due to the prolonged hypoxic time without gasping before resuscitation, and similar rates have been reported in out-of-hospital cardiac arrest in children [5, 13] and in previous studies with the same animal model of cardiac arrest, in which ROSC was achieved in 20% of animals treated with standard doses of epinephrine [23].
Our model simulates out-of-hospital CA in children, producing cardiorespiratory arrest due to hypoxia. In our study, we inhibited gasping to simulate the situation of CA secondary to apnea, in which a bystander calls the emergency team and performs basic resuscitation after a prolonged period of hypoxia; the emergency team arrives 9 min later and begins advanced resuscitation with intubation, ventilation with an FiO2 of 1, and the administration of epinephrine. Our results show that, in cases of prolonged hypoxia, the rate of ROSC is very low despite correct basic and advanced CPR. This fact underlines the importance of prevention and early resuscitation.
We found in a previous randomized crossover animal study of asphyxial cardiac arrest that ventilation combined with chest compressions achieved better ventilation than compressions alone, without causing deterioration in hemodynamic parameters. The tidal volume achieved with CC was practically undetectable and the ventilation produced was insufficient to achieve adequate gas exchange [23]. However, due to the different design of that study, it was not possible to analyze how the changes in the parameters affected survival.
Our study has produced a number of important results. First, neither of the basic CPR protocols achieved adequate oxygenation and ventilation in this model of asphyxial CA. However, better arterial oxygenation and ventilation were observed with chest compressions plus ventilation. Furthermore, cerebral saturation was higher in the VC group, although the difference did not reach statistical significance. In addition, both the PaCO2 and cerebral oxygenation remained somewhat better in the VC group during advanced resuscitation, when the same protocol was used in both groups.
Several studies have shown that the interruption of chest compressions in order to perform ventilation can be a major prognostic factor, as it alters the hemodynamic situation and decreases coronary, myocardial, and tissue perfusion [24–26]. In our study, there were no differences in the hemodynamic variables (blood pressure, cardiac index, and central venous pressure) between the two groups during resuscitation. These results support the idea that ventilation does not interfere with hemodynamic parameters when it is not coordinated with compressions and no pauses in compressions are required, whether during basic or advanced CPR. In our study, chest compressions achieved an adequate systolic blood pressure but a low MAP, with a normal or high cardiac index. However, measurement of the cardiac output using the PiCCO method can be unreliable during CPR due to the movements produced by the chest compressions and to the inability to recalibrate the system; the cardiac output was therefore only estimated from an analysis of the arterial curve.
Several authors have emphasized the risk of hyperventilation during resuscitation and after ROSC [1, 3, 6]. Ventilation during CPR can give rise to hypocapnia, with a secondary reduction in cerebral blood flow and increased mortality and/or neurological sequelae [1, 3, 6, 20].
The 2005 international recommendations for CPR changed the compression/ventilation ratio in pediatric patients from 5:1 to 30:2 for lay or single rescuers and 15:2 for two healthcare professionals in basic resuscitation and to reduce minute ventilation to less than baseline for age in advanced resuscitation [27]. Although the ideal ratio between ventilation and chest compressions in CA in children is still under discussion, the new recommendations are based on the pathophysiological basis that the cardiac output and pulmonary blood flow during CPR fall to 10–25% compared to normal values, and the ventilation necessary to achieve adequate gas exchange would therefore also be lower than under normal conditions [1–4, 24–28]. Our results show that when using a normal tidal volume of 10 ml/kg with a respiratory rate of 20 rpm, which is a higher rate than recommended, there is no risk of hyperventilation in either basic or advanced resuscitation. On the contrary, most animals were hypoventilated throughout the period of resuscitation (Fig. 3). Hypoventilation could cause lung collapse, which increases pulmonary vascular resistance and reduces left preload, leading to a fall in cardiac output. In our study, non-coordinated ventilation plus cardiac compressions was used to reduce the interruptions in compressions. Further studies are needed to determine whether coordinated ventilations and compressions could improve ventilation and oxygenation and to establish the effect on hemodynamic parameters.
Several recent articles have shown the risk of hyperoxia during neonatal resuscitation and after ROSC in adults [29, 30]. In our study, animals were hypoxic both during basic resuscitation with an FiO2 of 0.21 and during advanced resuscitation with an FiO2 of 1. These data suggest that the use of a high FiO2 during resuscitation in non-neonatal pediatric CA is not associated with a risk of hyperoxia.
There are a number of limitations to our study. As we indicated above, the sample size was small and survival in the two groups was low, thus making it difficult to establish statistically significant differences. A further limitation of our study is that no evaluation was performed of the subsequent course of the animals after ROSC, as all were killed after 20 min.
Chest compressions were not interrupted during ventilation. This improved the efficacy of chest compressions but did not simulate the current recommendations for initial bystander resuscitation. In addition, although ventilation was controlled by mechanical ventilation, the quality of the chest compressions could have been suboptimal. We performed manual cardiac massage as is done in clinical practice, measuring and controlling the frequency of compressions to adjust to 100/min. However, we did not control depth of compression or coronary blood flow, which are factors directly associated with ROSC. On the other hand, manual chest compressions could be different between the groups and it could introduce a bias in the results. However the experimental team was the same throughout the experiment, and chest compressors rotated out every 3 min.
Basic resuscitation is actually performed by synchronized mouth to mouth ventilation and chest compression in humans. It is not possible to give mouth to mouth ventilation in this animal model, and it is also very difficult to synchronize mechanical ventilation with manual chest compressions. We decided to use mask ventilation using a ventilator instead of manual ventilation so as to ensure delivery of a consistent tidal volume, which is very important if one wants to compare ventilation parameters between groups. The specific mask used in our study allows for its application to the snout of the pig, and assures that any leak is minimal.
As found in other studies, our results provide evidence of the important role of ventilations in basic CPR for infants and children [5, 13, 15–17, 23].
We conclude that non-coordinated VC achieved a nonsignificantly higher survival than cardiac compressions alone in this model of asphyxial pediatric cardiac arrest. Neither cardiac compressions alone nor non-coordinated ventilation and compressions achieved adequate oxygenation and ventilation. Chest compressions plus ventilation produced a better general and cerebral oxygenation and ventilation with no negative hemodynamic effects.
References
SOS-KANTO study group (2007) Cardiopulmonary resuscitation by bystanders with chest compression only (SOS-KANTO): an observational study. Lancet 369:920–926
Iwami T, Kawamura T, Hiraide A, Berg RA, Hayashi Y, Nishiuchi T, Kajino K, Yonemoto N, Yukioka H, Sugimoto H, Kakuchi H, Sase K, Yokoyama H, Nonogi H (2007) Effectiveness of bystander-initiated cardiac-only resuscitation for patients with out-of-hospital cardiac arrest. Circulation 116:2900–2907
Ong ME, Ng FS, Anushia P, Tham LP, Leong BS, Ong VY, Tiah L, Lim SH, Anantharaman V (2008) Comparison of chest compression only and standard cardiopulmonary resuscitation for out-of-hospital cardiac arrest in Singapore. Resuscitation 78:119–126
Kellum MJ, Kennedy KW, Barney R, Keilhauer Fa, Bellino M, Zuercher M, Ewy GA (2008) Cardiocerebral resuscitation improves neurologically intact survival of patients with out-of-hospital cardiac arrest. Ann Emerg Med 52:244–252
López-Herce J, Carrillo A (2010) Bystander CPR for paediatric out-of-hospital cardiac arrest. Lancet 375:1321–1322
Ewy GA, Zuercher M, Hilwig RW, Sanders AB, Berg RA, Otto CW, Hayes MM, Kern KB (2007) Improved neurological outcome with continuous chest compressions compared with 30:2 compressions-to-ventilations cardiopulmonary resuscitation in a realistic swine model of out-of-hospital cardiac arrest. Circulation 116:2525–2530
Berg RA, Kern KB, Hilwig RW, Berg MD, Sanders AB, Otto CW, Ewy GA (1997) Assisted ventilation does not improve outcome in a porcine model of single-rescuer bystander cardiopulmonary resuscitation. Circulation 95:1635–1641
Berg RA, Kern KB, Sanders AB, Otto CW, Hilwig RW, Ewy GA (1993) Bystander cardiopulmonary resuscitation. Is ventilation necessary? Circulation 88:1907–1915
Noc M, Weil MH, Tang W, Turner T, Fukui M (1995) Mechanical ventilation may not be essential for initial cardiopulmonary resuscitation. Chest 108:821–827
Kern KB, Hilwig RW, Berg RA, Ewy GA (1998) Efficacy of chest compression-only BLS CPR in the presence of an occluded airway. Resuscitation 39:179–188
Chandra NC, Gruben KG, Tsitlik JE, Brower R, Guerci AD, Halperin HH, Weisfeldt ML, Permutt S (1994) Observations of ventilation during resuscitation in a canine model. Circulation 90:3070–3075
Kitamura T, Iwami T, Kawamura T, Nagao K, Tanaka H, Hiraide A, Implementation Working Group for all Japan Utstein Registry of the Fire and Disaster Management Agency (2010) Bystander-initiated rescue breathing for out-of-hospital cardiac arrests of noncardiac origin. Circulation 122:293–299
Kitamura T, Iwami T, Kawamura T, Nagao K, Tanaka H, Nadkarni VM, Berg RA, Hiraide A, Implementation Working Group for all Japan Utstein Registry of the Fire and Disaster Management Agency (2010) Conventional and chest-compression-only cardiopulmonary resuscitation by bystanders for children who have out-of-hospital cardiac arrests: a prospective, nationwide, population-based cohort study. Lancet 375:1347–1354
Kitamura T, Iwami T, Kawamura T, Nagao K, Tanaka H, Berg RA, Hiraide A (2011) Time-dependent effectiveness of chest compression-only and conventional cardiopulmonary resuscitation for out-of-hospital cardiac arrest of cardiac origin. Resuscitation 82:3–9
Berg RA, Hemphill R, Abella BS, Aufderheide TP, Cave DM, Hazinski MF, Lerner EB, Rea TD, Sayre MR, Swor RA (2010) Part 5: adult basic life support: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 122(18 Suppl 3):S685–S705
Bobrow BJ, Spaite DW, Berg RA, Stolz U, Sanders AB, Kern KB, Vadeboncoeur TF, Clark LL, Gallagher JV, Stapczynski JS, LoVecchio F, Mullins TJ, Humble WO, Ewy GA (2010) Chest compression-only CPR by lay rescuers and survival from out-of-hospital cardiac arrest. JAMA 304:1447–1454
Sherman M (2007) The new American Heart Association cardiopulmonary resuscitation guidelines: should children and adults have to share? Curr Opin Pediatr 19:253–257
Topjian AA, Berg RA, Nadkarni VM (2008) Pediatric cardiopulmonary resuscitation: advances in science, techniques, and outcomes. Pediatrics 122:1086–1098
Berg RA, Hilwig RW, Kern KB, Babar I, Ewy GA (1999) Simulated mouth-to-mouth ventilation and chest compressions (bystander cardiopulmonary resuscitation) improves outcome in a swine model of prehospital pediatric asphyxial cardiac arrest. Crit Care Med 27:1893–1899
Berg RA, Hilwig RW, Kern KB, Ewy GA (2000) Bystander “chest compressions and assisted ventilation independently improve outcome from piglet asphyxial pulseless” cardiac arrest. Circulation 101:1743–1748
Lurie KG, Yannopoulos D, McKnite SH, Herman ML, Idris AH, Nadkarni VM, Tang W, Gabrielli A, Barnes TA, Metzger AK (2008) Comparison of a 10-breaths-per-minute versus a 2-breaths-per-minute strategy during cardiopulmonary resuscitation in a porcine model of cardiac arrest. Respir Care 53:862–870
Dorph E, Wik L, Stromme TA, Eriksen M, Steen PA (2004) Oxygen delivery and return of spontaneous circulation with ventilation:compression ratio 2:30 versus chest compressions only CPR in pigs. Resuscitation 60:309–318
Iglesias JM, López-Herce J, Urbano J, Solana MJ, Mencía S, Del Castillo J (2010) Chest compressions versus ventilation plus chest compressions in a pediatric asphyxial cardiac arrest animal model. Intensive Care Med 36:712–716
Idris AH, Banner MJ, Wenzel V, Fuerst RS, Becker LB, Melker RJ (1994) Ventilation caused by external chest compression is unable to sustain effective gas exchange during CPR: a comparison with mechanical ventilation. Resuscitation 28:143–150
Deakin CD, O’Neill JF, Tabor T (2007) Does compression-only cardiopulmonary resuscitation generate adequate passive ventilation during cardiac arrest? Resuscitation 75:53–59
Bobrow BJ, Ewy GA (2009) Ventilation during resuscitation efforts for out-of-hospital primary cardiac arrest. Curr Opin Crit Care 15:228–233
Kleinman ME, de Caen AR, Chameides L, Atkins DL, Berg RA, Bhanji F, Biarent D, Bingham R, Coovadia AH, Hazinski MF, Hickey RW, Nadkarni VM, Reis AG, Rodríguez-Nunez A, Tibballs J, Zaritsky AL, Zideman D, Pediatric Basic and Advanced Life Support Chapter Collaborators (2010) Part 10: pediatric basic and advanced life support: 2010 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation 122:S466–S515
Nagao K (2009) Chest compression-only cardiocerebral resuscitation. Curr Opin Crit Care 15:189–197
Kilgannon JH, Jones AE, Shapiro NI, Angelos MG, Milcarek B, Hunter K, Parrillo JE, Trzeciak S, Emergency Medicine Shock Research Network (EMShockNet) Investigators (2010) Association between arterial hyperoxia following resuscitation from cardiac arrest and in-hospital mortality. JAMA 303:2165–2171
Saugstad OD, Ramji S, Soll RF, Vento M (2008) Resuscitation of newborn infants with 21% or 100% oxygen: an updated systematic review and meta-analysis. Neonatology 94:176–182
Acknowledgments
We thank Mercedes Adrados and Natalia Sánchez of the Department of Experimental Medicine and Surgery of the Hospital General Universitario Gregorio Marañón for their collaboration in performing the experiments. This study was financed by grants PS09/00545 and N. RD08/0072: Maternal, Child Health and Development Network) within the framework of the VI National I+D+i Research Program (2008–2011)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Botran, M., Lopez-Herce, J., Urbano, J. et al. Chest compressions versus ventilation plus chest compressions: a randomized trial in a pediatric asphyxial cardiac arrest animal model. Intensive Care Med 37, 1873–1880 (2011). https://doi.org/10.1007/s00134-011-2338-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-011-2338-6