Abstract
Objectives
Aboriginal Canadians (i.e., First Nations, Inuit and Métis) are disproportionately affected by HIV/AIDS, and experience greater social and economic marginalization and poorer housing conditions. This study sought to understand the differences in the determinants of health and housing-related characteristics between samples of Aboriginal and Caucasian adults living with HIV/AIDS in Ontario.
Methods
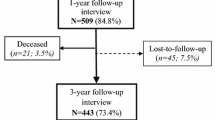
We analyzed baseline demographic, socio-economic, health, and housing-related data from 521 individuals (79 Aboriginal and 442 Caucasian) living with HIV/AIDS and enrolled in the Positive Spaces, Healthy Places study. We compared the characteristics of Aboriginal and Caucasian participants to identify determinants of health and housing-related characteristics independently associated with Aboriginal ethnicity.
Results
Compared to Caucausian participants living with HIV, Aboriginal participants were more likely to be younger, female or transgender women, less educated, unemployed, and homeless or unstably housed. They were also more likely to have low incomes and to have experienced housing-related discrimination. In a multivariate model, gender, income, and experiences of homelessness were independently associated with Aboriginal ethnicity.
Conclusion
Aboriginal individuals living with HIV/AIDS in our sample are coping with significantly worse social and economic conditions and are more likely to experience challenging housing situations than a comparison group of Caucasian individuals living with HIV/AIDS. To develop effective care, treatment and support strategies for Aboriginal peoples with HIV, it is critical to address and improve their socio-economic and housing conditions.
Résumé
Objectifs
Les Canadiens autochtones (Premières Nations, Inuits et Métis) sont démesurément touchés par le VIH et le sida; ils sont aussi plus marginalisés sur le plan socioéconomique et ont des conditions de logement inférieures. Nous avons cherché à comprendre les différences dans les déterminants de la santé et les caractéristiques de l’habitat d’échantillons d’adultes autochtones et blancs vivant avec le VIH ou le sida en Ontario.
Méthode
Nous avons analysé les données de base (démographiques, socioéconomiques, sanitaires et liées au logement) de 521 sujets (79 Autochtones, 442 Blancs) vivant avec le VIH ou le sida et participant à l’étude Positive Spaces, Healthy Places. Les caractéristiques des participants autochtones et blancs ont été comparées afin de cerner les déterminants de la santé et les caractéristiques de l’habitat présentant une association indépendante avec l’ethnicité autochtone.
Résultats
Comparativement aux participants blancs vivant avec le VIH, les participants autochtones étaient plus susceptibles d’être des jeunes, des femmes ou des femmes transgenre, d’être moins scolarisés, sans emploi, sans abri ou de vivre dans un logement précaire. Ils étaient aussi plus susceptibles d’avoir un faible revenu et d’avoir été victimes de discrimination liée au logement. Dans notre modèle multivarié, le sexe, le revenu et les expériences d’itinérance présentaient des associations indépendantes avec l’ethnicité autochtone.
Conclusion
Les sujets autochtones vivant avec le VIH ou le sida dans notre échantillon composent avec des conditions socioéconomiques beaucoup plus difficiles et sont plus susceptibles d’éprouver des problèmes à se loger que le groupe témoin de sujets blancs vivant avec le VIH et le sida. Pour élaborer des stratégies de soins, de traitement et de soutien efficaces pour les Autochtones atteints du VIH, il est essentiel d’aborder et d’améliorer leurs conditions socioéconomiques et de logement.
Similar content being viewed by others
References
Public Health Agency of Canada. HIV/AIDS among Aboriginal peoples in Canada: A continuing concern. Epi Update. Available at: https://doi.org/www.phacaspc.gc.ca/publicat/epiu-aepi/epi_update_may_04/9-eng.php (Accessed July 6, 2010).
Statistics Canada. Aboriginal identity population, by province and territory. 2006 Census. Available at: https://doi.org/www40.statcan.ca/101/cst01/demo60a-eng.htm (Accessed July 6, 2010).
Public Health Agency of Canada. Summary: Estimates of HIV Prevalence and Incidence in Canada, 2008. Available at: https://doi.org/www.phac-aspc.gc.ca/aids-sida/publication/survreport/estimat08-eng.php (Accessed July 16, 2010).
Liu J, Remis R. Race/Ethnicity Among Persons with HIV/AIDS in Ontario, 1981–2004. Ontario HIV Epidemiologic Monitoring Unit, 2007).
Wood E, Montaner JS, Li K, Zhang R, Barney L, Strathdee SA, et al. Burden of HIV infection among aboriginal injection drug users in Vancouver, British Columbia. Am J Public Health 2008;98(3):515–19.
Wood E, Kerr T, Palepu A, Zhang R, Strathdee SA, Tyndall MW, et al. Slower uptake of HIV antiretroviral therapy among Aboriginal injection drug users. J Infect 2006;52(4):233–36.
Miller CL, Spittal PM, Wood E, Chan K, Schechter MT, Montaner JS, et al. Inadequacies in antiretroviral therapy use among Aboriginal and other Canadian populations. AIDS Care 2006;18(8):968–76.
Wood E, Montaner JS, Chan K, Tyndall MW, Schechter MT, Bangsberg D, et al. Socioeconomic status, access to triple therapy, and survival from HIV-disease since 1996. AIDS 2002;16(15):2065–72.
Lima VD, Kretz P, Palepu A, Bonner S, Kerr T, Moore D, et al. Aboriginal status is a prognostic factor for mortality among antiretroviral naive HIV positive individuals first initiating HAART. AIDS Res Ther 2006;3:14.
Royal Commission on Aboriginal Peoples. Report of the Royal Commission on Aboriginal Peoples. Ottawa, ON: Supply and Services Canada, 1996).
National Aboriginal Housing Association. A Time for Action: A National Plan to Address Aboriginal Housing. Ottawa: NAHA, 2009).
Jakubec L, Engeland J, Prentice J. Research Highlight - Revised Aboriginal Households. 2004. Ottawa, Canadian Mortgage and Housing Corporation. 2001 Housing Series.
Joint United Nations Programme on HIV/AIDS (UNAIDS). From Principle to Practice: Greater Involvement of People Living With or Affected by HIV/AIDS (GIPA). Geneva, Switzerland: UNAIDS, 1999).
Tucker R, Rourke SB, Greene S, Bekele T, Bhuiyan S, Sobota M, et al. Housing and health-related quality of life among persons living with HIV/AIDS: Design and implementation of the Positive Spaces, Healthy Places Study. AIDS Behav J under review.
Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The Alcohol Use Disorders Identification Test (AUDIT): Guidelines for Use in Primary Health Care. Geneva: World Health Organization, 1992).
Skinner HA. The Drug Abuse Screening Test (DAST-20). Addict Behav 1982;7(4):363–71.
Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Measurement 1977;1(3):385.
Akaike H. A new look at the statistical model identification. IEEE Transactions on Automatic Control 1974;19(6):716–23.
Perusse D. Aboriginal People Living Off-Reserve and the Labour Market: Estimates from the Labour Force Survey, 2007. Ottawa: Statistics Canada, 2008).
Jackson R, Reimer G. Canadian Aboriginal People Living With HIV/AIDS: Care, Treatment and Support Issues. Ottawa: Canadian Aboriginal AIDS Network, 2005).
McCall J, Browne AJ, Reimer-Kirkham S. Struggling to survive: The difficult reality of Aboriginal women living with HIV/AIDS. Qual Health Res 2009;19(12):1769–82.
Palepu A, Yip B, Miller C, Strathdee SA, O’Shaughnessy MV, Montaner JS, et al. Factors associated with the response to antiretroviral therapy among HIV-infected patients with and without a history of injection drug use. AIDS 2001;15(3):423–24.
Mehrabadi A, Craib KJ, Patterson K, Adam W, Moniruzzaman A, Ward-Burkitt B, et al. The Cedar Project: A comparison of HIV-related vulnerabilities amongst young Aboriginal women surviving drug use and sex work in two Canadian cities. Int J Drug Policy 2008;19(2):159–68.
McKay-McNabb K. Life experiences of Aboriginal women living with HIV/AIDS. Can J Aboriginal Community-Based HIV/AIDS Res 2005;1:5–16.
Rourke SB, Sobota M, Tucker R, Bekele T, Gibson K, Greene S, et al. Social determinants of health in HIV/HCV co-infection compared to HIV infection only: Results from the “Positive Spaces, Healthy Places” Study. Open Medicine Journal in press.
Clarke JN, Friedman DB, Hoffman-Goetz L. Canadian Aboriginal people’s experiences with HIV/AIDS as portrayed in selected English language Aboriginal media (1996–2000). Soc Sci Med 2005;60(10):2169–80.
Smylie J, Anderson M. Understanding the health of Indigenous peoples in Canada: Key methodological and conceptual challenges. CMAJ 2006;175(6):602.
Author information
Authors and Affiliations
Consortia
Additional information
Dedication: This article is dedicated to the memory of LaVerne Monette, co-investigator with the CIHR-funded Positive Spaces, Healthy Places (PSHP) research project, who passed away December 1, 2010. Responsible for the Aboriginal arm of the study, she played a key role in developing the questionnaire, analyzing the data and presenting the findings. She brought to our team her life experiences as an Aboriginal woman and her passion to help Aboriginal people living with and at risk of HIV. She understood the critical role of housing in health and quality of life, and was a strong advocate for research to identify the housing needs of Aboriginal people in Ontario and for policy change that will lead to safe, stable housing for all.
Acknowledgements: This work was supported by grants from the Canadian Institutes of Health Research, the Ontario Ministry of Health and Long-Term Care, the Ontario AIDS Network, the Wellesley Institute, and the Ontario HIV Treatment Network.
Conflict of Interest: None to declare.
Rights and permissions
About this article
Cite this article
Monette, L.E., Rourke, S.B., Gibson, K. et al. Inequalities in Determinants of Health Among Aboriginal and Caucasian Persons Living With HIV/AIDS in Ontario: Results From the Positive Spaces, Healthy Places Study. Can J Public Health 102, 215–219 (2011). https://doi.org/10.1007/BF03404900
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03404900