Abstract
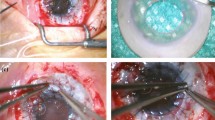
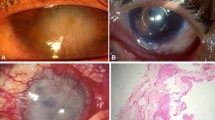
• Background: Severe stem cell deficiencies uniformly lead to superficial conjunctivalization of corneal grafts with subsequent functional failure. We sought better long-term results by transplanting central corneolimbal grafts and simultaneously protecting the graft and its stem cells from immunological destruction by means of systemic administration of ciclosporin A. • Patients and methods: In an ongoing pilot study, up to April 1995 20 eyes with stem cell dysfunctions of various etiology (e.g. chemical burn, ocular pseudopemphigoid, congenital aniridia) received eccentrically trephined fresh corneal grafts of 7.7–10.0 mm diameter. About one third of the circumference of the grafts contained limbal area. The mean age of the patients was 46.2 years (range 9–84 years). All patients received systemic ciclosporin A for at least 12 months. At present, the mean follow-up period is 9.6 months (mean 1–20.6 months). • Results: Fourteen of 20 grafts (70%) have remained clear so far. Reasons for six graft failures were surface disorders in four eyes, immune reactions in one eye and surface disorders in combination with immune reactions in another eye. Ten of 20 grafts (50%) experienced severe surface disorders. In six eyes surface disorders were coincident with endothelial immune reactions, in four eyes they were not. In four of 20 grafts (20%) conjunctivalization was observed in front of the transplanted limbal area; in seven of 20 grafts (35%) conjunctivalization occurred only distant from the transplanted limbal stem cells. • Conclusions: Our method of central corneolimbal transplantation with simultaneous protection of the transplanted stem cell population from immunological destruction by means of systemic ciclosporin A has been successful for 14 eyes with severe stem cell deficiencies up to 20.6 months postoperatively. This new treatment principle promises — for the first time — long-term rehabilitation for a majority of eyes with severe limbal stem cell deficiencies.
Similar content being viewed by others
References
Chen JY, Tseng SCG (1990) Corneal epithelial wound healing in partial limbal deficiency. Invest Ophthalmol Vis Sci 31:1301–1314
Duke-Elder S, Leigh A (1965) Diseases of the outer eye. Corneal grafts. In: Duke-Elder S (ed) System of ophthalmology, vol 8. Kimpton, London, pp 648–66
Herman WK, Doughman, DJ, Lindstrom, RL (1983) Conjunctival autograft transplantation for unilateral ocular surface diseases. Ophthalmology 90:1121–1126
Hoppeler T, Balogh T, Kalman A, Gloor B (1993) Autologe Limbustransplantation nach Verätzung. In: Gloor B, Hartmann C, Rochels R (eds) Kongreßband DGII. Springer, Berlin Heidelberg New York, pp 429–433
Huang AJW, Tseng SCG (1991) Corneal epithelial wound healing in the absence of limbal epithelium. Invest Ophthalmot Vis Sci 32:96–105
Kenyon KR, Tseng SCG (1989) Limbal autograft transplantation for ocular surface disorders. Ophthalmology 96:709–723
Kuckelkorn R, Redbrake C, Schrage NF, Reim M (1993) Keratoplastik mit 11–12 mm Durchmesser zur Versorgung von schwerstverätzten Augen. Ophthalmologe 90:683–687
Mytilineos J, Scherer S, Opeltz G (1990) Comparison of RFLP DR beta and serological HLA-DR typing in 1500 individuals. Transplantation 50:870–873
Pets E, Gaag R van der (1984/1985) HLA-A, B, C, and HLA-DR antigens and dendritic cells in fresh and organ culture preserved corneas. Cornea 3:231–239
Redbrake C, Tympnert J, Reim M (1993) Komplikationen nach Keratoplastik. Ophthalmologe 90 [Suppl 1]:147
Reinhard T, Sundmacher R, Heering P (1995) Systemic ciclosporin A in high-risk keratoplasty. Graefe's Arch Clin Exp Ophthalmol
Sundmacher R (1977) Immunreaktionen nach Keratoplastik. Klin Monatsbl Augenheilkd 171:705–722
Sundmacher R, Stefansson A, Mackensen G (1983) Verlaufsbeobachtungen nach Keratoplastik. Fortschr Ophthalmol 80:224–227
Sundmacher R, Reinhard T, Heering P (1992) Six years' experience with systemic cyclosporin A prophylaxis in high-risk perforating keratoplasty patients. Ger J Ophthalmol 1:432–436
Tan DTH, Ficker LA, Buckley RJ (1994) Limbal transplantation. Invest Ophthalmol Vis Sci 35:1913
Thoft RA (1977) Conjunctival transplantation. Arch Ophthalmol 95:1425–1427
Tsai RJ, Sun T, Tseng SCG (1990) Comparison of limbal and conjunctival autograft transplantation in corneal surface reconstruction in rabbits. Ophthalmology 97:446–455
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Sundmacher, R., Reinhard, T. Central corneolimbal transplantation under systemic ciclosporin A cover for severe limbal stem cell insufficiency. Graefe's Arch Clin Exp Ophthalmol 234 (Suppl 1), S122–S125 (1996). https://doi.org/10.1007/BF02343060
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF02343060