Summary
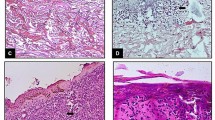
A total of 77 human skin wounds with a post-infliction interval between 3 h and 7 months were investigated and the proliferation marker antigen Ki 67 was visualized in paraffin sections using a specific monoclonal antibody (MIB). The re-built epidermal layer covering the former lesional area showed only a few basal cells positively staining for Ki 67 antigen. No enhanced reactivity was found when compared to uninjured skin. In basal cells of the epidermis adjacent to the wound area, however, varying numbers of positive cells occurred, but no information useful for a reliable time estimation of skin wounds could be obtained due to the considerable variability in the number of Ki 67 positive epidermal basal cells found in non-damaged skin. Fibroblastic cells in the wound area revealed an increased number of Ki 67-positive sites which could first be detected in a 1.5-day-old skin lesion. Positive results could be obtained in every specimen investigated after a post-infliction interval of 6 days up to 1.5 months. Only the scar tissue of the oldest wound examined (wound age 7 months) revealed no increase in the number of positively staining fibroblasts. Therefore, positive results indicate a wound age of at least approximately 1.5 days and the lack of an increased number of positive fibroblastic cells in a sufficient number of specimens indicates at a wound age of less than 6 days, but cannot totally exclude longer post-infliction intervals.
Zusammenfassung
In Paraffinschnitten von 77 menschlichen Hautwunden mit einer Überlebenszeit zwischen 3 Std und 7 Monaten wurde das Ki 67-Antigen mit einem monoklonalen Antikörper (MIB) immunhistochemisch dargestellt. Die neugebildete Epidermis zeigte lediglich einzelne, positiv reagierende Keratinozyten, eine verstärkte Reaktivität im Vergleich zu unverletzten Hautarealen war nicht feststellbar. Die epidermalen Basalzellschichten, die dem ursprünglichen Epitheldefekt benachbart waren, wiesen jedoch eine unterschiedlich ausgeprägte Anfärbbarkeit auf. Eine Aussage zum Wundalter war anhand der Zahl positiv reagierender Basalzellen wegen der beträchtlichen intra- wie auch inter-individuellen Streubreite der Befunde nicht möglich. Eine relevant erhöhte Zahl positiv reagierender fibroblastärer Zellen im Wundgebiet verglichen mit unverletzter Dermis trat erstmals in einer 1,5 Tage überlebten Wunde auf und war in allen untersuchten Wunden ab 6 Tagen Überlebenszeit bis zu einem Wundalter von 1,5 Monaten zu beobachten. Lediglich die älteste untersuchte Läsion (Wundalter 7 Monate) zeigte keine relevante Zahl Ki 67-exprimierender Fibroblasten im Narbengewebe. Positive Befunde belegen somit eine Überlebenszeit von mindestens 1,5 Tagen. Das Fehlen einer erhöhten Zahl positiv anfärbbarer fibroblastärer Zellen in einer ausreichenden Anzahl von Präparaten weist auf ein Wundalter unter ca. 6 Tagen hin, kann ein solches allerdings nicht mit letzter Sicherheit beweisen.
Similar content being viewed by others
References
Betz P, Nerlich A, Wilske J, Tübel J, Penning R, Eisenmenger W (1992) Time-dependent appearance of myofibroblasts in granulation tissue of human skin wounds. Int J Leg Med 105:99–103
Betz P, Nerlich A, Tübel J, Penning R, Eisenmenger W (1993) The time-dependent expression of keratins 5 and 13 during the reepithelization of human skin wounds. Int J Leg Med 105:229–232
Betz P, Nerlich A, Wilske J, Tübel J, Wiest I, Penning R, Eisenmenger W (1992) Time-dependent pericellular expression of collagen type IV, laminin, and heparan sulfate proteoglycan in myofibroblasts. Int J Leg Med 105:169–172
Block P, Seiter I, Oehlert W (1963) Autoradiographic studies of the initial cellular response to injury. Exp Cell Res 30:311–321
Brown DC, Gatter KC (1990) Monoclonal antibody Ki67: its use in histopathology. Histopathology 17:489–503
Cordell JL, Falini B, Erber WN, Ghosh AK, Abdulaziz Z, MacDonald S, Pulford AF, Stein H, Mason DY (1984) Immunoenzymatic labeling of monoclonal antibodies using immune complexes of alkaline phosphatase and monoclonal antialkaline phosphatase (APAAP-complex). J Histochem Cytochem 32:219–229
Cottier H, Dreher R, Keller HU, Roos B, Hess MW (1976) Cytokinetic aspects of wound healing. In: Longacre JJ (ed) The ultrastructure of collagen. Thomas, Springfield/Ill, pp 108–131
Cottier H (ed) (1980) Pathogenese. Handbuch für die ärztliche Fortbildung. Springer, Berlin Heidelberg New York
De Vito RV (1965) Healing of wounds. Surg Clin North Am 45:441–459
Gerdes J, Schwab U, Lemke H, Stein H (1983) Production of a mouse monoclonal antibody reactive with a nuclear antigen associated with cell proliferation. Int J Cancer 31:13–20
Gerdes J, Lemke U, Baisch H, Wacker H-H, Schwab U, Stein H (1984) Cell cycle analysis of a cell proliferation human nuclear antigen defined by the monoclonal antibody Ki 67. J Immunol 133:1710–1715
Gerdes J, Becker M, Key G, Cattoretti G (1992) Immunohistologic detection of tumor growth factor (Ki 67-antigen) in formalin fixed and routinely processed tissue. J Pathol (in press)
Hell EA, Cruickshank CND (1963) The effect of injury upon uptake of3H-thymidine by guinea pig epidermis. Exp Cell Res 31:128–139
McMinn RMM (1969) Tissue repair. Academic Press, New York London
Oehmichen M, Schmidt V (1988) DNS-Synthese epidermaler Basalzellen als Indikator des Wundalters. Beitr Gerichtl Med XLVI:271–276
Oehmichen M, Lagodka T (1991) Time-dependent RNA synthesis in different skin layers after wounding. Experimental investigations in vital and postmortem biopsies. Int J Leg Med 104:153–159
Ortonne J-P, Löning T, Schmitt D, Thivolet J (1981) Immunomorphological and ultrastructural aspects of keratinocyte migration in epidermal wound healing. Virchows Arch [A] 392:217–230
Ralfkiaer E, Stein H, Bosq J, Gatter KC, Ralfkiaer N, Lange Wantzin G, Mason DY (1986) Expression of a cell-cycle-associated nuclear antigen (Ki 67) in cutaneous lymphoid infiltrates. Am J Dermatopathol 8:37–43
Ross R, Benditt EP (1961) Wound healing and collagen formation. J Cell Biol 15:99–108
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Betz, P., Nerlich, A., Wilske, J. et al. The time-dependent localization of Ki 67 antigen-positive cells in human skin wounds. Int J Leg Med 106, 35–40 (1993). https://doi.org/10.1007/BF01225022
Received:
Revised:
Issue Date:
DOI: https://doi.org/10.1007/BF01225022