Abstract
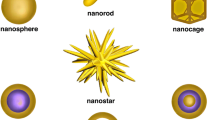
The problem of occupational exposure to nanoparticles (NP) has raised many questions which remain unanswered today: When airborne NPs, either dissociated or more commonly in the form of aggregates, are inhaled by humans, will they produce a biological and/or tissular response where they are deposited, i.e., in the respiratory tract, or at some distance from the deposition area, i.e., an indirect effect secondary to the inflammatory response of the respiratory tract or a direct effect due to translocation of nanoparticles through the biological membranes?
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Comité de la prévention et de la précaution (CPP): Nanotechnologies, nanoparticules: quels dangers, quels risques? Ministère de l’Ecologie et du Développement durable, 1–64, www.ecologie.gouv.fr (2006)
W.G. Kreyling, M. Semmler-Behnke, J. Seitz, W. Scymczak, A. Wenk, P. Mayer, S. Takenaka, G. Oberdorster: Size dependence of the translocation of inhaled iridium and carbon nanoparticle aggregates from the lung of rats to the blood and secondary target organs. Inhal. Toxicol. 21 (S1), 55–60 (2009)
T. Xia, N. Li, A.E. Nel: Potential health impact of nanoparticles. Annu. Rev. Public Health 30, 137–150 (2009)
A. Nel, T. Xia, L. Mädler, N. Li: Toxic potential of materials at the nano level. Science 311, 622–627 (2006)
K. Donaldson, P.J. Borm, G. Oberdorster, K.E. Pinkerton, V. Stone, C.L. Tran: Concordance between in vitro and in vivo dosimetry in the proinflammatory effects of low-toxicity, low-solubility particles: The key role of the proximal alveolar region. Inhal. Toxicol. 20, 53–62 (2008)
G. Oberdorster, E. Oberdorster, J. Oberdorster: Nanotoxicology: An emerging discipline evolving from studies of ultrafine particles. Environ. Health Perspect. 113, 823–839 (2005)
M.F. Stanton, C. Wrench: Mechanisms of mesothelioma induction with asbestos and fibrous glass. J. Natl. Cancer Inst. 48, 797–821 (1972)
M.W. Frampton: Systemic and cardiovascular effects of airway injury and inflammation: Ultrafine particle exposure in humans. Environ. Health Perspect. 109 (Suppl. 4), 529–532 (2001)
A. Nemmar, P.H. Hoet, B. Vanquickenborne, D. Dinsdale, M. Thomeer, M.F. Hoylaerts, H. Vanbilloen, L. Mortelmans, B. Nemery: Passage of inhaled particles into the blood circulation in humans. Circulation 105, 411–414 (2002)
C.C. Daigle, D.C. Chalupa, F.R. Gibb, P.E. Morrow, G. Oberdorster, M.J. Utell, M.W. Frampton: Ultrafine particle deposition in humans during rest and exercise. Inhal. Toxicol. 15, 539–552 (2003)
A.P. Pietropaoli, M.W. Frampton, R.W. Hyde, P.E. Morrow, G. Oberdorster, C. Cox, D.M. Speers, L.M. Frasier, D.C. Chalupa, L.S. Huang, M.J. Utell: Pulmonary function, diffusing capacity, and inflammation in healthy and asthmatic subjects exposed to ultrafine particles. Inhal. Toxicol. 16 (Suppl. 1), 59–72 (2004)
D.C. Chalupa, P.E. Morrow, G. Oberdorster, M.J. Utell, M.W. Frampton: Ultrafine particle deposition in subjects with asthma. Environ. Health Perspect. 112, 879–882 (2004)
M.W. Frampton, M.J. Utell, W. Zareba, G. Oberdorster, C. Cox, L.S. Huang, P.E. Morrow, F.E. Lee, D. Chalupa, L.M. Frasier, D.M. Speers, J. Stewart: Effects of exposure to ultrafine carbon particles in healthy subjects and subjects with asthma. Res. Respir. Health Eff. Inst. 126, 1–47 (2004)
W.S. Beckett, D.F. Chalupa, A. Pauly-Brown, D.M. Speers, J.C. Stewart, M.W. Frampton, M.J. Utell, L.S. Huang, C. Cox, W. Zareba, G. Oberdorster: Comparing inhaled ultrafine versus fine zinc oxide particles in healthy adults: A human inhalation study. Am. J. Respir. Crit. Care Med. 171, 1129–1135 (2005)
M.W. Frampton: Inflammation and airborne particles. Clin. Occup. Environ. Med. 5, 797–815 (2006)
H.C. Routledge, S. Manney, R.M. Harrison, J.G. Ayres, J.N. Townend: Effect of inhaled sulphur dioxide and carbon particles on heart rate variability and markers of inflammation and coagulation in human subjects. Heart 92, 220–227 (2006)
P. Wiebert, A. Sanchez-Crespo, R. Falk, K. Philipson, A. Lundin, S. Larsson, W. Moller, W.G. Kreyling, M. Svartengren: No significant translocation of inhaled 35-nm carbon particles to the circulation in humans. Inhal. Toxicol. 18, 741–747 (2006)
N.L. Mills, N. Amin, S.D. Robinson, A. Anand, J. Davies, D. Patel, J.M. de la Fuente, F.R. Cassee, N.A. Boon, W. Macnee, A.M. Millar, K. Donaldson, D.E. Newby: Do inhaled carbon nanoparticles translocate directly into the circulation in humans? Am. J. Respir. Crit. Care Med. 173, 426–431 (2006)
J. Londahl, A. Massling, J. Pagels, E. Swietlicki, E. Vaclavik, S. Loft: Size-resolved respiratory-tract deposition of fine and ultrafine hydrophobic and hygroscopic aerosol particles during rest and exercise. Inhal. Toxicol. 19, 109–116 (2007)
W. Moller, K. Felten, K. Sommerer, G. Scheuch, G. Meyer, P. Meyer, K. Haussinger, W.G. Kreyling: Deposition, retention, and translocation of ultrafine particles from the central airways and lung periphery. Am. J. Respir. Crit. Care Med. 177, 426–432 (2008)
A.P. Shah, A.P. Pietropaoli, L.M. Frasier, D.M. Speers, D.C. Chalupa, J.M. Delehanty, L.S. Huang, M.J. Utell, M.W. Frampton: Effect of inhaled carbon ultrafine particles on reactive hyperemia in healthy human subjects. Environ. Health Perspect. 116, 375–380 (2008)
W. Zareba, J.P. Couderc, G. Oberdorster, D. Chalupa, C. Cox, L.S. Huang, A. Peters, M.J. Utell, M.W. Frampton: ECG parameters and exposure to carbon ultrafine particles in young healthy subjects. Inhal. Toxicol. 21, 223–233 (2009)
IARC 2006: http://monographs.iarc.fr/ENG/Meetings/93-carbonblack.pdf, http://monographs.iarc.fr/ENG/Meetings/93-titaniumdioxide.pdf
K. Gardiner, M. van Tongeren, M. Harrington: Respiratory health effects from exposure to carbon black: Results of the phase 2 and 3 cross-sectional studies in the European carbon black manufacturing industry. Occup. Environ. Med. 58, 496–503 (2001)
M.J. Van Tongeren, K. Gardiner, C.E. Rossiter, J. Beach, P. Harber, M.J. Harrington: Longitudinal analyses of chest radiographs from the European Carbon Black Respiratory Morbidity Study. Eur. Respir. J. 20, 417–425 (2002)
K. Gardiner, N.W. Trethowan, J.M. Harrington, C.E. Rossiter, I.A. Calvert: Respiratory health effects of carbon black: A survey of European carbon black workers. Br. J. Ind. Med. 50, 1082–1096 (1993)
J.T. Hodgson, R.D. Jones: A mortality study of carbon black workers employed at five United Kingdom factories between 1947 and 1980. Arch. Environ. Health 40, 261–268 (1985)
T. Sorahan, L. Hamilton, M. van Tongeren, K. Gardiner, J.M. Harrington: A cohort mortality study of UK carbon black workers, 1951–1996. Am. J. Ind. Med. 39, 158–170 (2001)
NIOSH Evaluation of Health Hazard and Recommendations for Occupational Exposure to Titanium Dioxide 2005: www.cdc.gov/niosh/review/public/TIo2/pdfs/TIO2Draft.pdf
J.L. Chen, W.E. Fayerweather: Epidemiologic study of workers exposed to titanium dioxide. J. Occup. Med. 30, 937–942 (1988)
J.P. Fryzek, B. Chadda, D. Marano, K. White, S. Schweitzer, J.K. McLaughlin, W.J. Blot: A cohort mortality study among titanium dioxide manufacturing workers in the United States. J. Occup. Environ. Med./Am. Coll. Occup. Environ. Med. 45, 400–409 (2003)
J.J. Beaumont, M.S. Sandy, C.D. Sherman: Titanium dioxide and lung cancer. J. Occup. Environ. Med. 46, 759 (2004); erratum: 1189
P. Boffetta, V. Gaborieau, L. Nadon, M.F. Parent, E. Weiderpass, J. Siemiatycki: Exposure to titanium dioxide and risk of lung cancer in a population-based study from Montreal. Scand. J. Work. Environ. Health. 27, 227–232 (2001)
P. Boffetta, A. Soutar, J.W. Cherrie, F. Granath, A. Andersen, A. Anttila, M. Blettner, V. Gaborieau, S.J. Klug, S. Langard, D. Luce, F. Merletti, B. Miller, D. Mirabelli, E. Pukkala, H.O. Adami, E. Weiderpass: Mortality among workers employed in the titanium dioxide production industry in Europe. Cancer Causes Control 15, 697–706 (2004)
Y. Song, X. Li, X. Du: Exposure to nanoparticles is related to pleural effusion, pulmonary fibrosis and granuloma. Eur. Respir. J. 34, 559–567 (2009)
C.A. Pope, R.T. Burnett, G.D. Thurston, M.J. Thun, E.E. Calle, D. Krewski, J.J. Godleski: Cardiovascular mortality and long-term exposure to particulate air pollution: Epidemiological evidence of general pathophysiological pathways of disease. Circulation 109, 71–77 (2004)
J.M. Antonini, A.B. Lewis, J.R. Roberts, D.A. Whaley: Pulmonary effects of welding fumes: Review of worker and experimental animal studies. Am. J. Ind. Med. 43, 350–360 (2003)
A. Peretz, J.H. Sullivan, D.F. Leotta, C.A. Trenga, F.N. Sands, J. Allen, C. Carlsten, C.W. Wilkinson, E.A. Gill, J.D. Kaufman: Diesel exhaust inhalation elicits acute vasoconstriction in vivo. Environ. Health Perspect. 116, 937–942 (2008)
E.V. Brauner, L. Forchhammer, P. Moller, J. Simonsen, M. Glasius, P. Wahlin, O. Raaschou-Nielsen, S. Loft: Exposure to ultrafine particles from ambient air and oxidative stress-induced DNA damage. Environ. Health Perspect. 115, 1177–1182 (2007)
J.M. Samet, A. Rappold, D. Graff, W.E. Cascio, J.H. Berntsen, Y.C. Huang, M. Herbst, M. Bassett, T. Montilla, M.J. Hazucha, P.A. Bromberg, R.B. Devlin: Concentrated ambient ultrafine particle exposure induces cardiac changes in young healthy volunteers. Am. J. Respir. Crit. Care Med. 179, 1034–1042 (2009)
S.A. Kharitonov, P.J. Barnes: Exhaled biomarkers. Chest 130, 1541–1546 (2006)
B. Balbi, P. Pignatti, M. Corradi, P. Baiardi, L. Bianchi, G. Brunetti, A. Radaeli, G. Moscato, A. Mutti, A. Spanevello, M. Malerba: Bronchoalveolar lavage, sputum and exhaled clinically relevant inflammatory markers: Values in healthy adults. Eur. Respir. J. 30, 769–781 (2007)
M.C. Levesque, D.W. Hauswirth, S. Mervin-Blake, C.A. Fernandez, K.B. Patch, K.M. Alexander, S. Allgood, P.D. McNair, A.S. Allen, J.S. Sundy: Determinants of exhaled nitric oxide levels in healthy, nonsmoking African American adults. J. Allergy Clin. Immunol. 121, 396–402, e3 (2008)
I. Horvath, J. Hunt, P.J. Barnes, K. Alving, A. Antczak, E. Baraldi, G. Becher, W.J. van Beurden, M. Corradi, R. Dekhuijzen, R.A. Dweik, T. Dwyer, R. Effros, S. Erzurum, B. Gaston, C. Gessner, A. Greening, L.P. Ho, J. Hohlfeld, Q. Jobsis, D. Laskowski, S. Loukides, D. Marlin, P. Montuschi, A.C. Olin, A.E. Redington, P. Reinhold, E.L. van Rensen, I. Rubinstein, P. Silkoff, K. Toren, G. Vass, C. Vogelberg, H. Wirtz: Exhaled breath condensate: Methodological recommendations and unresolved questions. Eur. Respir. J. 26, 523–548 (2005)
P.P. Rosias, C.M. Robroeks, A. Kester, G. Jden Hartog, W.K. Wodzig, G.T. Rijkers, L.J.V. Zimmermann, C.P. van Schayck, Q. Jobsis, E. Dompeling: Biomarker reproducibility in exhaled breath condensate collected with different condensers. Eur. Respir. J. 31, 934–942 (2008)
H. Knobloch, G. Becher, M. Decker, P. Reinhold: Evaluation of H2O2 and pH in exhaled breath condensate samples: Methodical and physiological aspects. Biomarkers 13, 319–341 (2008)
D.W. Hauswirth, J.S. Sundy, S. Mervin-Blake, C.A. Fernandez, K.B. Patch, K.M. Alexander, S. Allgood, P.D. McNair, M.C. Levesque: Normative values for exhaled breath condensate pH and its relationship to exhaled nitric oxide in healthy African Americans. J. Allergy Clin. Immunol. 122, 101–106 (2008)
M.J. Cruz, S. Sanchez-Vidaurre, P.V. Romero, F. Morell, X. Munoz: Impact of age on pH, 8-isoprostane, and nitrogen oxides in exhaled breath condensate. Chest 135, 462–467 (2009)
M. Malerba, B. Ragnoli, M. Corradi: Non-invasive methods to assess biomarkers of exposure and early stage of pulmonary disease in smoking subjects. Monaldi Arch. Chest Dis. 69, 128–133 (2008)
K. Hildebrandt, R. Ruckerl, W. Koenig, A. Schneider, M. Pitz, J. Heinrich, V. Marder, M. Frampton, G. Oberdorster, H.E. Wichmann, A. Peters: Short-term effects of air pollution: A panel study of blood markers in patients with chronic pulmonary disease. Part. Fibre Toxicol. 6, 25 (2009)
M. Gulumian, P.J. Borm, V. Vallyathan, V. Castranova, K. Donaldson, G. Nelson, J. Murray: Mechanistically identified suitable biomarkers of exposure, effect, and susceptibility for silicosis and coal-worker’s pneumoconiosis: A comprehensive review. J. Toxicol. Environ. Health B Crit. Rev. 9, 357–395 (2006)
D.M. Mannino, D. Thorn, A. Swensen, F. Holguin: Prevalence and outcomes of diabetes, hypertension and cardiovascular disease in COPD. Eur. Respir. J. 32, 962–969 (2008)
F.L. Fimognari, S. Scarlata, M.E. Conte, R.A. Incalzi: Mechanisms of atherothrombosis in chronic obstructive pulmonary disease. Int. J. Chron. Obstruct. Pulmon. Dis. 3, 89–96 (2008)
R.D. Brook, B. Franklin, W. Cascio, Y. Hong, G. Howard, M. Lipsett, R. Luepker, M. Mittleman, J. Samet, S.C. Smith, I. Tager: Air pollution and cardiovascular disease: A statement for healthcare professionals from the Expert Panel on Population and Prevention Science of the American Heart Association. Circulation 109, 2655–2671 (2004)
A. Peretz, E.C. Peck, T.K. Bammler, R.P. Beyer, J.H. Sullivan, C.A. Trenga, S. Srinouanprachnah, F.M. Farin, J.D. Kaufman: Diesel exhaust inhalation and assessment of peripheral blood mononuclear cell gene transcription effects: An exploratory study of healthy human volunteers. Inhal. Toxicol. 19, 1107–1119 (2007)
A.J. Lucking, M. Lundback, N.L. Mills, D. Faratian, S.L. Barath, J. Pourazar, F.R. Cassee, K. Donaldson, N.A. Boon, J.J. Badimon, T. Sandstrom, A. Blomberg, D.E. Newby: Diesel exhaust inhalation increases thrombus formation in man. Eur. Heart J. 29, 3043–3051 (2008)
H. Tornqvist, N.L. Mills, M. Gonzalez, M.R. Miller, S.D. Robinson, I.L. Megson, W. Macnee, K. Donaldson, S. Soderberg, D.E. Newby, T. Sandstrom, A. Blomberg: Persistent endothelial dysfunction in humans after diesel exhaust inhalation. Am. J. Respir. Crit. Care Med. 176, 395–400 (2007)
N. Mills, N. Amin, S. Robinson, et al.: Do inhaled carbon nanoparticles translocate directly into the circulation in humans? Am. J. Respir. Crit. Care Med. 173, 426–431 (2006)
N.L. Mills, S.D. Robinson, P.H. Fokkens, D.L. Leseman, M.R. Miller, D. Anderson, E.J. Freney, M.R. Heal, R.J. Donovan, A. Blomberg, T. Sandstrom, W. MacNee, N.A. Boon, K. Donaldson, D.E. Newby, F.R. Cassee: Exposure to concentrated ambient particles does not affect vascular function in patients with coronary heart disease. Environ. Health Perspect. 116, 709–715 (2008)
A.J. Ghio, Y.C. Huang: Exposure to concentrated ambient particles (CAPs): A review. Inhal. Toxicol. 16, 53–59 (2004)
M.W. Frampton, J.C. Stewart, G. Oberdorster, P.E. Morrow, D. Chalupa, A.P. Pietropaoli, L.M. Frasier, D.M. Speers, C. Cox, L.S. Huang, M.J. Utell: Inhalation of ultrafine particles alters blood leukocyte expression of adhesion molecules in humans. Environ. Health Perspect. 114, 51–58 (2006)
P.P. Simeonova, A. Erdely: Engineered nanoparticle respiratory exposure and potential risks for cardiovascular toxicity: Predictive tests and biomarkers. Inhal. Toxicol. 21 (S1), 68–73 (2009)
A. Erdely, T. Hulderman, R. Salmen, A. Liston, P.C. Zeidler-Erdely, D. Schwegler-Berry, V. Castranova, S. Koyama, Y.A. Kim, M. Endo, P.P. Simeonova: Cross-talk between lung and systemic circulation during carbon nanotube respiratory exposure. Potential biomarkers. Nano Lett. 9, 36–43 (2009)
M. Semmler, J. Seitz, F. Erbe, P. Mayer, J. Heyder, G. Oberdorster, W.G. Kreyling: Long-term clearance kinetics of inhaled ultrafine insoluble iridium particles from the rat lung, including transient translocation into secondary organs. Inhal. Toxicol. 16, 453–459 (2004)
P. Wiebert, A. Sanchez-Crespo, J. Seitz, R. Falk, K. Philipson, W.G. Kreyling, W. Moller, K. Sommerer, S. Larsson, M. Svartengren: Negligible clearance of ultrafine particles retained in healthy and affected human lungs. Eur. Respir. J. 28, 286–290 (2006)
Z. Chen, H. Chen, H. Meng, G. Xing, X. Gao, B. Sun, X. Shi, H. Yuan, C. Zhang, R. Liu, F. Zhao, Y. Zhao, X. Fang: Bio-distribution and metabolic paths of silica coated CdSeS quantum dots. Toxicol. Appl. Pharmacol. 230, 364–371 (2008)
X. He, H. Nie, K. Wang, W. Tan, X. Wu, P. Zhang: In vivo study of biodistribution and urinary excretion of surface-modified silica nanoparticles. Anal. Chem. 80, 9597–9603 (2008)
M.T. Zhu, W.Y. Feng, Y. Wang, B. Wang, M. Wang, H. Ouyang, Y.L. Zhao, Z.F. Chai: Particokinetics and extrapulmonary translocation of intratracheally instilled ferric oxide nanoparticles in rats and the potential health risk assessment. Toxicol. Sci. 107, 342–351 (2009)
A.A. Burns, J. Vider, H. Ow, E. Herz, O. Penate-Medina, M. Baumgart, S.M. Larson, U. Wiesner, M. Bradbury: Fluorescent silica nanoparticles with efficient urinary excretion for nanomedicine. Nano Lett. 9, 442–448 (2009)
W.S. Cho, M. Cho, S.R. Kim, M. Choi, J.Y. Lee, B.S. Han, S.N. Park, M.K. Yu, S. Jon, J. Jeong: Pulmonary toxicity and kinetic study of Cy5.5-conjugated superparamagnetic iron oxide nanoparticles by optical imaging. Toxicol. Appl. Pharmacol 239, 106–115 (2009)
K. Sarlo, K.L. Blackburn, E.D. Clark, J. Grothaus, J. Chaney, S. Neu, J. Flood, D. Abbott, C. Bohne, K. Casey, C. Fryer, M. Kuhn: Tissue distribution of 20 nm, 100 nm and 1000 nm fluorescent polystyrene latex nanospheres following acute systemic or acute and repeat airway exposure in the rat. Toxicology 263, 117–126 (2009)
A. Seaton: Nanotechnology and the occupational physician. Occup. Med. 56, 312–316 (2006)
A. Seaton, L. Tran, R. Aitken, K. Donaldson: Nanoparticles, human health hazard and regulation. J. Roy. Soc. Interface 7 (Suppl. 1), S119–S129 (2010)
M. Nasterlack, A. Zober, C. Oberlinner: Considerations on occupational medical surveillance in employees handling nanoparticles. Int. Arch. Occup. Environ. Health 81, 721–726 (2008)
NIOSH: Interim guidance for medical screening and hazard surveillance for workers potentially exposed to engineered nanoparticles. Current Intelligence Bulletin 60. National Institute for Occupational Safety and Health. Department of Health and Human Services, February 2009. Publication No. 2009-116 (2009)
W.E. Halperin, J. Ratcliffe, T.M. Frazier, L. Wilson, S.P. Becker, P.A. Schulte: Medical screening in the workplace: Proposed principles. J. Occup. Med. 28, 547–552 (1986)
P.A. Schulte, M.K. Schubauer-Berigan, C. Mayweather, C.L. Geraci, R. Zumwalde, J.L. McKernan: Issues in the development of epidemiologic studies of workers exposed to engineered nanoparticles. J. Occup. Environ. Med. 51, 323–335 (2009)
M. Saunders: Transplacental transport of nanomaterials. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 1, 671–684 (2009)
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2011 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Brochard, P., Bloch, D., Pairon, JC. (2011). Occupational Exposure to Nanoparticles and Medical Safety. In: Houdy, P., Lahmani, M., Marano, F. (eds) Nanoethics and Nanotoxicology. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-20177-6_11
Download citation
DOI: https://doi.org/10.1007/978-3-642-20177-6_11
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-20176-9
Online ISBN: 978-3-642-20177-6
eBook Packages: Physics and AstronomyPhysics and Astronomy (R0)