Abstract
Providing neuroprotection to reduce secondary brain injury after neurological surgery and after an acute neurological insult is the primary goal of neuroanesthesia and neurocritical care. While several pharmacological and nonpharmacological agents have provided much promise in preclinical animal models of neurological injury, there is no single agent that has been unequivocally proven to provide neuroprotection in human patients. In this chapter, we review the recent clinical studies that demonstrate the evidence for and against several agents that have been investigated in the context of perioperative neuroprotection after neurological surgery and after acute neurological insults including stroke and traumatic brain injury (TBI). Several therapeutic agents have been shown to provide neuroprotection in specific injuries or patient populations, and the plethora of agents that have yielded promising results in preclinical studies justifies the enormous time and expense that is necessary to conduct large-scale clinical trials.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Badenes R, Gruenbaum SE, Bilotta F. Cerebral protection during neurosurgery and stroke. Curr Opin Anaesthesiol. 2015;28(5):532–6.
Bilotta F, Stazi E, Zlotnik A, Gruenbaum SE, Rosa G. Neuroprotective effects of intravenous anesthetics: a new critical perspective. Curr Pharm Des. 2014;20(34):5469–75.
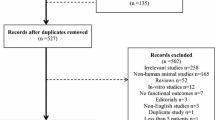
Gruenbaum SE, Zlotnik A, Gruenbaum BF, Hersey D, Bilotta F. Pharmacologic neuroprotection for functional outcomes after traumatic brain injury: a systematic review of the clinical literature. CNS Drugs. 2016;30(9):791–806.
Faden AI, Shirane R, Chang LH, James TL, Lemke M, Weinstein PR. Opiate-receptor antagonist improves metabolic recovery and limits neurochemical alterations associated with reperfusion after global brain ischemia in rats. J Pharmacol Exp Ther. 1990;255(2):451–8.
Zheng J, Li H, Guo R, Chen R, Lin S, Liu M, et al. Neuroprotection of nalmefene for postoperative patients with spontaneous intracerebral hemorrhage. Int J Neurosci. 2015;125(12):918–23.
Uchida K, Yasunaga H, Sumitani M, Horiguchi H, Fushimi K, Yamada Y. Effects of remifentanil on in-hospital mortality and length of stay following clipping of intracranial aneurysm: a propensity score-matched analysis. J Neurosurg Anesthesiol. 2014;26(4):291–8.
Roach GW, Newman MF, Murkin JM, Martzke J, Ruskin A, Li J, et al. Ineffectiveness of burst suppression therapy in mitigating perioperative cerebrovascular dysfunction. Multicenter Study of Perioperative Ischemia (McSPI) Research Group. Anesthesiology. 1999;90(5):1255–64.
Kanbak M, Saricaoglu F, Avci A, Ocal T, Koray Z, Aypar U. Propofol offers no advantage over isoflurane anesthesia for cerebral protection during cardiopulmonary bypass: a preliminary study of S-100beta protein levels. Canadian journal of anaesthesia =. Journal canadien d’anesthesie. 2004;51(7):712–7.
Abdelmalak BB, Knittel J, Abdelmalak JB, Dalton JE, Christiansen E, Foss J, et al. Preoperative blood glucose concentrations and postoperative outcomes after elective non-cardiac surgery: an observational study. Br J Anaesth. 2014;112(1):79–88.
Waxweiler RJ, Thurman D, Sniezek J, Sosin D, O’Neil J. Monitoring the impact of traumatic brain injury: a review and update. J Neurotrauma. 1995;12(4):509–16.
Gerber LM, Chiu YL, Carney N, Hartl R, Ghajar J. Marked reduction in mortality in patients with severe traumatic brain injury. J Neurosurg. 2013;119(6):1583–90.
Marmarou A, Lu J, Butcher I, McHugh GS, Mushkudiani NA, Murray GD, et al. IMPACT database of traumatic brain injury: design and description. J Neurotrauma. 2007;24(2):239–50.
Falleti MG, Maruff P, Burman P, Harris A. The effects of growth hormone (GH) deficiency and GH replacement on cognitive performance in adults: a meta-analysis of the current literature. Psychoneuroendocrinology. 2006;31(6):681–91.
Moreau OK, Cortet-Rudelli C, Yollin E, Merlen E, Daveluy W, Rousseaux M. Growth hormone replacement therapy in patients with traumatic brain injury. J Neurotrauma. 2013;30(11):998–1006.
Devesa J, Reimunde P, Devesa P, Barbera M, Arce V. Growth hormone (GH) and brain trauma. Horm Behav. 2013;63(2):331–44.
Gardner CJ, Mattsson AF, Daousi C, Korbonits M, Koltowska-Haggstrom M, Cuthbertson DJ. GH deficiency after traumatic brain injury: improvement in quality of life with GH therapy: analysis of the KIMS database. Eur J Endocrinol. 2015;172(4):371–81.
Agha A, Rogers B, Sherlock M, O’Kelly P, Tormey W, Phillips J, et al. Anterior pituitary dysfunction in survivors of traumatic brain injury. J Clin Endocrinol Metab. 2004;89(10):4929–36.
Mahmood A, Goussev A, Kazmi H, Qu C, Lu D, Chopp M. Long-term benefits after treatment of traumatic brain injury with simvastatin in rats. Neurosurgery. 2009;65(1):187–91; discussion 91–2.
Lu D, Goussev A, Chen J, Pannu P, Li Y, Mahmood A, et al. Atorvastatin reduces neurological deficit and increases synaptogenesis, angiogenesis, and neuronal survival in rats subjected to traumatic brain injury. J Neurotrauma. 2004;21(1):21–32.
Sanchez-Aguilar M, Tapia-Perez JH, Sanchez-Rodriguez JJ, Vinas-Rios JM, Martinez-Perez P, de la Cruz-Mendoza E, et al. Effect of rosuvastatin on cytokines after traumatic head injury. J Neurosurg. 2013;118(3):669–75.
Orlando A, Bar-Or D, Salottolo K, Levy AS, Mains CW, Slone DS, et al. Unintentional discontinuation of statins may increase mortality after traumatic brain injury in elderly patients: a preliminary observation. J Clin Med Res. 2013;5(3):168–73.
Yoles E, Belkin M, Schwartz M. HU-211, a nonpsychotropic cannabinoid, produces short- and long-term neuroprotection after optic nerve axotomy. J Neurotrauma. 1996;13(1):49–57.
Shohami E, Biegon A. Novel approach to the role of NMDA receptors in traumatic brain injury. CNS Neurol Disord Drug Targets. 2014;13(4):567–73.
Nguyen BM, Kim D, Bricker S, Bongard F, Neville A, Putnam B, et al. Effect of marijuana use on outcomes in traumatic brain injury. Am Surg. 2014;80(10):979–83.
Brewster ME, Pop E, Foltz RL, Reuschel S, Griffith W, Amselem S, et al. Clinical pharmacokinetics of escalating i.v. doses of dexanabinol (HU-211), a neuroprotectant agent, in normal volunteers. Int J Clin Pharmacol Ther. 1997;35(9):361–5.
Knoller N, Levi L, Shoshan I, Reichenthal E, Razon N, Rappaport ZH, et al. Dexanabinol (HU-211) in the treatment of severe closed head injury: a randomized, placebo-controlled, phase II clinical trial. Crit Care Med. 2002;30(3):548–54.
Maas AI, Murray G, Henney 3rd H, Kassem N, Legrand V, Mangelus M, et al. Efficacy and safety of dexanabinol in severe traumatic brain injury: results of a phase III randomised, placebo-controlled, clinical trial. Lancet Neurol. 2006;5(1):38–45.
Clifton GL, Ziegler MG, Grossman RG. Circulating catecholamines and sympathetic activity after head injury. Neurosurgery. 1981;8(1):10–4.
Mohseni S, Talving P, Wallin G, Ljungqvist O, Riddez L. Preinjury beta-blockade is protective in isolated severe traumatic brain injury. J Trauma Acute Care Surg. 2014;76(3):804–8.
Arbabi S, Campion EM, Hemmila MR, Barker M, Dimo M, Ahrns KS, et al. Beta-blocker use is associated with improved outcomes in adult trauma patients. J Trauma. 2007;62(1):56–61; discussion 60–2.
Sekhon B, Sekhon C, Khan M, Patel SJ, Singh I, Singh AK. N-Acetyl cysteine protects against injury in a rat model of focal cerebral ischemia. Brain Res. 2003;971(1):1–8.
Hicdonmez T, Kanter M, Tiryaki M, Parsak T, Cobanoglu S. Neuroprotective effects of N-acetylcysteine on experimental closed head trauma in rats. Neurochem Res. 2006;31(4):473–81.
Hoffer ME, Balaban C, Slade MD, Tsao JW, Hoffer B. Amelioration of acute sequelae of blast induced mild trauamatic brain injury by N-acetyl cysteine: a double-blind, placebo controlled study. PloS one. 2013;8(1):e54163.
Shand B, Strey C, Scott R, Morrison Z, Gieseg S. Pilot study on the clinical effects of dietary supplementation with Enzogenol, a flavonoid extract of pine bark and vitamin C. Phytotherapy Res. 2003;17(5):490–4.
Theadom A, Mahon S, Barker-Collo S, McPherson K, Rush E, Vandal AC, et al. Enzogenol for cognitive functioning in traumatic brain injury: a pilot placebo-controlled RCT. Eur J Neurol Off J Eur Fed Neurol Soc. 2013;20(8):1135–44.
Masliah E, Diez-Tejedor E. The pharmacology of neurotrophic treatment with Cerebrolysin: brain protection and repair to counteract pathologies of acute and chronic neurological disorders. Drugs Today (Barc). 2012;48 Suppl A:3–24.
Chen CC, Wei ST, Tsaia SC, Chen XX, Cho DY. Cerebrolysin enhances cognitive recovery of mild traumatic brain injury patients: double-blind, placebo-controlled, randomized study. Br J Neurosurg. 2013;27(6):803–7.
Guzik TJ, West NE, Pillai R, Taggart DP, Channon KM. Nitric oxide modulates superoxide release and peroxynitrite formation in human blood vessels. Hypertension. 2002;39(6):1088–94.
Terpolilli NA, Zweckberger K, Trabold R, Schilling L, Schinzel R, Tegtmeier F, et al. The novel nitric oxide synthase inhibitor 4-amino-tetrahydro-L-biopterine prevents brain edema formation and intracranial hypertension following traumatic brain injury in mice. J Neurotrauma. 2009;26(11):1963–75.
Stover JF, Belli A, Boret H, Bulters D, Sahuquillo J, Schmutzhard E, et al. Nitric oxide synthase inhibition with the antipterin VAS203 improves outcome in moderate and severe traumatic brain injury: a placebo-controlled randomized Phase IIa trial (NOSTRA). J Neurotrauma. 2014;31(19):1599–606.
Deutsch ER, Espinoza TR, Atif F, Woodall E, Kaylor J, Wright DW. Progesterone’s role in neuroprotection, a review of the evidence. Brain Res. 2013;1530:82–105.
Wei J, Xiao GM. The neuroprotective effects of progesterone on traumatic brain injury: current status and future prospects. Acta Pharmacol Sin. 2013;34(12):1485–90.
Shakeri M, Boustani MR, Pak N, Panahi F, Salehpour F, Lotfinia I, et al. Effect of progesterone administration on prognosis of patients with diffuse axonal injury due to severe head trauma. Clin Neurol Neurosurg. 2013;115(10):2019–22.
Xiao G, Wei J, Yan W, Wang W, Lu Z. Improved outcomes from the administration of progesterone for patients with acute severe traumatic brain injury: a randomized controlled trial. Critical care (London, England). 2008;12(2):R61.
Wright DW, Kellermann AL, Hertzberg VS, Clark PL, Frankel M, Goldstein FC, et al. ProTECT: a randomized clinical trial of progesterone for acute traumatic brain injury. Ann Emerg Med. 2007;49(4):391–402, e1–2.
Skolnick BE, Maas AI, Narayan RK, van der Hoop RG, MacAllister T, Ward JD, et al. A clinical trial of progesterone for severe traumatic brain injury. N Engl J Med. 2014;371(26):2467–76.
Kelly DF. Alcohol and head injury: an issue revisited. J Neurotrauma. 1995;12(5):883–90.
Raj R, Skrifvars MB, Kivisaari R, Hernesniemi J, Lappalainen J, Siironen J. Acute alcohol intoxication and long-term outcome in patients with traumatic brain injury. J Neurotrauma. 2015;32(2):95–100.
Pandit V, Patel N, Rhee P, Kulvatunyou N, Aziz H, Green DJ, et al. Effect of alcohol in traumatic brain injury: is it really protective? J Surg Res. 2014;190(2):634–9.
Scheyerer MJ, Dutschler J, Billeter A, Zimmermann SM, Sprengel K, Werner CM, et al. Effect of elevated serum alcohol level on the outcome of severely injured patients. Emerg Med J. 2014;31(10):813–7.
Cormio M, Gopinath SP, Valadka A, Robertson CS. Cerebral hemodynamic effects of pentobarbital coma in head-injured patients. J Neurotrauma. 1999;16(10):927–36.
Levin AB, Duff TA, Javid MJ. Treatment of increased intracranial pressure: a comparison of different hyperosmotic agents and the use of thiopental. Neurosurgery. 1979;5(5):570–5.
Chen HI, Malhotra NR, Oddo M, Heuer GG, Levine JM, LeRoux PD. Barbiturate infusion for intractable intracranial hypertension and its effect on brain oxygenation. Neurosurgery. 2008;63(5):880–6; discussion 6–7.
Schwartz ML, Tator CH, Rowed DW, Reid SR, Meguro K, Andrews DF. The University of Toronto head injury treatment study: a prospective, randomized comparison of pentobarbital and mannitol. Can J Neurol Sci. 1984;11(4):434–40.
Ward JD, Becker DP, Miller JD, Choi SC, Marmarou A, Wood C, et al. Failure of prophylactic barbiturate coma in the treatment of severe head injury. J Neurosurg. 1985;62(3):383–8.
Majdan M, Mauritz W, Wilbacher I, Brazinova A, Rusnak M, Leitgeb J. Barbiturates use and its effects in patients with severe traumatic brain injury in five European countries. J Neurotrauma. 2013;30(1):23–9.
Mellion SA, Bennett KS, Ellsworth GL, Moore K, Riva-Cambrin J, Metzger RR, et al. High-dose barbiturates for refractory intracranial hypertension in children with severe traumatic brain injury. Pediatr Crit Care Med J Soc Crit Care Med World Fed Pediatr Intensive Crit Care Soc. 2013;14(3):239–47.
Siren AL, Fratelli M, Brines M, Goemans C, Casagrande S, Lewczuk P, et al. Erythropoietin prevents neuronal apoptosis after cerebral ischemia and metabolic stress. Proc Natl Acad Sci U S A. 2001;98(7):4044–9.
Aloizos S, Evodia E, Gourgiotis S, Isaia EC, Seretis C, Baltopoulos GJ. Neuroprotective effects of erythropoietin in patients with severe closed brain injury. Turk Neurosurg. 2015;25(4):552–8.
Robertson CS, Hannay HJ, Yamal JM, Gopinath S, Goodman JC, Tilley BC, et al. Effect of erythropoietin and transfusion threshold on neurological recovery after traumatic brain injury: a randomized clinical trial. JAMA. 2014;312(1):36–47.
Nichol A, French C, Little L, Haddad S, Presneill J, Arabi Y, et al. Erythropoietin in traumatic brain injury (EPO-TBI): a double-blind randomised controlled trial. Lancet. 2015;386(10012):2499–506.
Talke PO, Sharma D, Heyer EJ, Bergese SD, Blackham KA, Stevens RD. Republished: Society for Neuroscience in Anesthesiology and Critical Care expert consensus statement: anesthetic management of endovascular treatment for acute ischemic stroke. Stroke J Cereb Circ. 2014;45(8):e138–50.
Huang Z, Filipovic Z, Mp N, Ung C, Troy EL, Colburn RW, et al. AC105 increases extracellular magnesium delivery and reduces excitotoxic glutamate exposure within injured spinal cords in rats. J Neurotrauma. 2016.
Saver JL, Starkman S, Eckstein M, Stratton SJ, Pratt FD, Hamilton S, et al. Prehospital use of magnesium sulfate as neuroprotection in acute stroke. N Engl J Med. 2015;372(6):528–36.
Gibson CL, Bath PM. Feasibility of progesterone treatment for ischaemic stroke. J Cereb Blood Flow Metab Off J Int Soc Cereb Blood Flow Metab. 2016;36(3):487–91.
van den Berg LA, Koelman DL, Berkhemer OA, Rozeman AD, Fransen PS, Beumer D, et al. Type of anesthesia and differences in clinical outcome after intra-arterial treatment for ischemic stroke. Stroke J Cereb Circ. 2015;46(5):1257–62.
van den Berg LA, Roos YB. Response to letter regarding article, “type of anesthesia and differences in clinical outcome after intra-arterial treatment for ischemic stroke”. Stroke J Cereb Circ. 2015;46(9):e218.
Boyko M, Gruenbaum SE, Gruenbaum BF, Shapira Y, Zlotnik A. Brain to blood glutamate scavenging as a novel therapeutic modality: a review. J Neural Transm (Vienna, Austria : 1996). 2014;121(8):971–9.
Boyko M, Zlotnik A, Gruenbaum BF, Gruenbaum SE, Ohayon S, Kuts R, et al. Pyruvate’s blood glutamate scavenging activity contributes to the spectrum of its neuroprotective mechanisms in a rat model of stroke. Eur J Neurosci. 2011;34(9):1432–41.
Zhumadilov A, Boyko M, Gruenbaum SE, Brotfain E, Bilotta F, Zlotnik A. Extracorporeal methods of blood glutamate scavenging: a novel therapeutic modality. Expert Rev Neurother. 2015;15(5):501–8.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Gruenbaum, S.E., Bilotta, F. (2017). Neuroprotection in Neuroanesthesia and Neurocritical Care. In: Khan, Z. (eds) Challenging Topics in Neuroanesthesia and Neurocritical Care. Springer, Cham. https://doi.org/10.1007/978-3-319-41445-4_26
Download citation
DOI: https://doi.org/10.1007/978-3-319-41445-4_26
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-41443-0
Online ISBN: 978-3-319-41445-4
eBook Packages: MedicineMedicine (R0)