Abstract
Surgery presents an infectious risk that varies depending on several factors. First of all, emergency interventions present a greater risk of infection than elective interventions, while other risk factors are related to the type of surgery, the organ concerned, the length of surgery, and the type of subject undergoing the surgical procedure.
Other risk factors are related to the kind of patient one is dealing with, and frail patients are at the highest infectious risk.
Frailty has always been considered linked to disability, comorbidity, and other characteristics, but it may actually have a biological basis and be a distinct clinical syndrome.
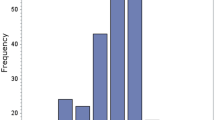
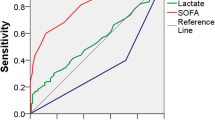
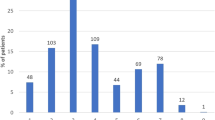
Regardless of the subject’s risk factors, early diagnosis of sepsis is essential, starting with the stratification of patients which can be carried out through classification methods. The SOFA (Sequential Organ Failure Assessment) score, which has been updated very recently by a Consensus on the definition of Sepsis and Septic Shock, takes into consideration some parameters that evaluate the severity of the clinical and metabolic structure.
Among the scores used, in addition to C-reactive protein and procalcitonin, recently, other biomarkers have been studied.
In the treatment of sepsis, the goal is to use the correct antibiotic as soon as possible.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Krislyn M, Mueck L, Kao S. Patients at high-risk for surgical site infection. Surg Infect (Larchmt). 2017;18(4):440–6.
Vogel TR, Dombrovskiy VY, et al. Impact of infectious complications after elective surgery on hospital readmission and late deaths in the U.S. Medicare population. Surg Infect (Larchmt). 2012;13(5):307–11.
Winograd CH. Targeting strategies: an overview of criteria and outcomes. J Am Geriatr Soc. 1991;39S:25S–35S.
McMillan GJ, Hubbard RE. Frailty in older inpatients: what physicians need to know. Q J Med. 2012;105:1059–65.
Ling ML, Apisarnthanarak A, Azlina Abbas A, et al. APSIC guidelines for the prevention of surgical site infections. Antimicrob Resist Infect Control. 2019;8:174.
Shao J, Zhang H, Yin B, et al. Risk factors for surgical site infection following operative treatment of ankle fractures: a systematic review and meta-analysis. Int J Surg. 2018;56:124–32.
Levy MM, FinkMP MJC, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Crit Care Med. 2003;31:1250–6.
Nasa P, Juneja D, Singh O. Severe sepsis and septic shock in elderly. World J Crit Care Med. 2012;1(1):23–30.
Dombrovskiy VY, Martin AA, Sunderram J, et al. Rapid increase in hospitalization and mortality rates for severe sepsis in the United States: a trend analysis from 1993 to 2003. Crit Care Med. 2007;35:1244–50.
Martin GS, Mannino DM, Moss M. The effect of age on the development and outcome of adult sepsis. Crit Care Med. 2006;34:15–21.
Girard TD, Opal SM, Ely EW. Insights into severe sepsis in older patients: from epidemiology to evidence-based management. Clin Infect Dis. 2003;40:719–27.
Walter LC, Brand RJ, Counsell SR, et al. Development and validation of a prognostic index for 1-year mortality in older adults after hospitalization. JAMA. 2001;285:2987–94.
Valenti WM, Trudell RG, Bentley DW. Factors predisposing to oropharyngeal colonization with gram-negative bacilli in the aged. N Engl J Med. 1978;298:1108–11.
Tomsic I, Chaberny IF, Krauth C, et al. Implementation interventions in preventing surgical site infections in abdominal surgery: a systematic review. BMC Health Serv Res. 2020;20(1):236.
Sartelli M, Chichom-Mefire A, Labricciosa FM, et al. The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg. 2017;12:29.
Sartelli M. A focus on intra-abdominal infections. World J Emerg Surg. 2010;5:9.
Xiaodong Y, Bin S, Xing Z, et al. Incomplete immune reconstitution in HIV/AIDS patients on antiretroviral therapy: challenges of immunological non-responders. J Leukoc Biol. 2020;107(4):597–612.
Singer M, Deutschman CS, et al. The third international consensus definition for sepsis and septic shock (sepsis-3). JAMA. 2016;315:801–10.
Faix JD. Biomarkers of sepsis. Crit Rev Clin Lab Sci. 2013;50(1):23–6.
Ghezzi P, Cerami A. Tumor necrosis factor as a pharmacological target. Methods Mol Med. 2004;98:1–8.
Petilla V, Hynninen M, Takkunen O, et al. Predictive value of procalcitonin and interleukin 6 in critically ill patients with suspected sepsis. Intensive Care Med. 2002;28:1220–5.
Eliasson M, Egesten A. Antibacterial chemokines: actors in both innate and adaptive immunity. In: Herwald H, Egesten A, editors. Contributions to microbiology: trends in innate immunity, vol. 15. Basel: Karger; 2008. p. 101–17.
Geven C, Kox M, Pikkers P. Adrenomedullin and Adrenomedullin-targeted therapy as treatment strategies relevant for sepsis. Front Immunol. 2018;9:292.
Chen YX, Li CS. Prognostic value of adrenomedullin in septic patients in the ED. Am J Emerg Med. 2013;31(7):1017–21.
Mierzchala-Pasierb M, Lipinska-Gediga M. Sepsis diagnosis and monitoring-procalcitonin as standard, but what next? Anaesthesiol Intensive Ther. 2019;51(4):299–305.
CZhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054.
Gallo Marin B, Aghagoli G, Lavine K. Predictors of Covid-19 severity: a literature review. Rev Med Virol. 2021;31(1):1–10.
Zaninotto M, Mion MM, Marchioro L. Endothelial dysfunction and mid-regional proAdrenomedullin: what role in SARS-CoV-2 infected patients? Clin Chim Acta. 2021;523:185–90.
Lelubre C, Anselin S, Zouaoui Boudjeltia K, et al. Interpretation of C-reactive protein concentration in critically ill patients. Biomed Res Int. 2013;2013:124021.
Song M, Kellum JA. Interleukin-6. Crit Care Med. 2005;33(12 Suppl):S463–5.
Mahroum N, Mahagna H, Amital H. Diagnosis and classification of adult still’s disease. J Autoimmun. 2014;48:34–7.
Alexandre, Mendonça Helena, Santos Ricardo, Franco-Duarte Paula, Sampaio. Fungal infections diagnosis – Past present and future. Res Microbiol. 2022;173(3) 103915-S0923250821001297 103915 https://doi.org/10.1016/j.resmic.2021.103915.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Beltrame, A., Anselmo, M. (2023). Recognition and Early Management of Sepsis in Frail Patients. In: Aseni, P., Grande, A.M., Leppäniemi, A., Chiara, O. (eds) The High-risk Surgical Patient. Springer, Cham. https://doi.org/10.1007/978-3-031-17273-1_13
Download citation
DOI: https://doi.org/10.1007/978-3-031-17273-1_13
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-17272-4
Online ISBN: 978-3-031-17273-1
eBook Packages: MedicineMedicine (R0)