Abstract
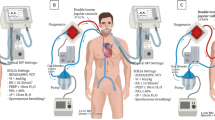
Extracorporeal systems are increasingly used in severe hypoxemic and/or hypercapnic respiratory failure [1]. Although recent data have shown an advantage of high-flow veno-venous extracorporeal membrane oxygenation (VV-ECMO) in severe acute respiratory distress syndrome (ARDS) [2, 3], there is a paucity of evidence regarding the utility of extracorporeal CO2 removal (ECCO2R, often similarly used: low-flow ECMO) in patients with respiratory failure. Despite this fact, the number of available systems is dramatically increasing. In this chapter, we therefore provide an overview of the currently used technologies with advantages and disadvantages in the light of physiology.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Karagiannidis C, Brodie D, Strassmann S, et al. Extracorporeal membrane oxygenation: evolving epidemiology and mortality. Intensive Care Med. 2016;42:889–96.
Combes A, Hajage D, Capellier G, et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. N Engl J Med. 2018;378:1965–75.
Peek GJ, Mugford M, Tiruvoipati R, et al. Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicentre randomised controlled trial. Lancet. 2009;374:1351–63.
Zanella A, Castagna L, Salerno D, et al. Respiratory electrodialysis. A novel, highly efficient extracorporeal CO2 removal technique. Am J Respir Crit Care Med. 2015;192:719–26.
Karagiannidis C, Strassmann S, Philipp A, Muller T, Windisch W. Veno-venous extracorporeal CO2 removal improves pulmonary hypertension in acute exacerbation of severe COPD. Intensive Care Med. 2015;41:1509–10.
Schaefer KE. Respiratory pattern and respiratory response to CO2. J Appl Physiol. 1958;13:1–14.
Karagiannidis C, Lubnow M, Philipp A, et al. Autoregulation of ventilation with neurally adjusted ventilatory assist on extracorporeal lung support. Intensive Care Med. 2010;36:2038–44.
Brochard L, Slutsky A, Pesenti A. Mechanical ventilation to minimize progression of lung injury in acute respiratory failure. Am J Respir Crit Care Med. 2017;195:438–42.
Biscotti M, Gannon WD, Agerstrand C, et al. Awake extracorporeal membrane oxygenation as bridge to lung transplantation: a 9-year experience. Ann Thorac Surg. 2017;104:412–9.
Crotti S, Bottino N, Ruggeri GM, et al. Spontaneous breathing during extracorporeal membrane oxygenation in acute respiratory failure. Anesthesiology. 2017;126:678–87.
Crotti S, Bottino N, Spinelli E. Spontaneous breathing during veno-venous extracorporeal membrane oxygenation. J Thorac Dis. 2018;10:S661–9.
Jeffries RG, Lund L, Frankowski B, Federspiel WJ. An extracorporeal carbon dioxide removal (ECCO2R) device operating at hemodialysis blood flow rates. Intensive Care Med Exp. 2017;5:41.
Karagiannidis C, Kampe KA, Sipmann FS, et al. Veno-venous extracorporeal CO2 removal for the treatment of severe respiratory acidosis: pathophysiological and technical considerations. Crit Care. 2014;18:R124.
Liu GM, Jin DH, Jiang XH, et al. Numerical and in vitro experimental investigation of the hemolytic performance at the off-design point of an axial ventricular assist pump. ASAIO J. 2016;62:657–65.
Giersiepen M, Wurzinger LJ, Opitz R, Reul H. Estimation of shear stress-related blood damage in heart valve prostheses—in vitro comparison of 25 aortic valves. Int J Artif Organs. 1990;13:300–6.
Fraser KH, Zhang T, Taskin ME, Griffith BP, Wu ZJ. A quantitative comparison of mechanical blood damage parameters in rotary ventricular assist devices: shear stress, exposure time and hemolysis index. J Biomech Eng. 2012;134:081002.
Del Sorbo L, Pisani L, Filippini C, et al. Extracorporeal CO2 removal in hypercapnic patients at risk of noninvasive ventilation failure: a matched cohort study with historical control. Crit Care Med. 2015;43:120–7.
Karagiannidis C, Strassmann S, Brodie D, et al. Impact of membrane lung surface area and blood flow on extracorporeal CO2 removal during severe respiratory acidosis. Intensive Care Med Exp. 2017;5:34.
Zhang J, Chen X, Ding J, et al. Computational study of the blood flow in three types of 3D hollow fiber membrane bundles. J Biomech Eng. 2013;135:121009.
Lubnow M, Philipp A, Foltan M, et al. Technical complications during veno-venous extracorporeal membrane oxygenation and their relevance predicting a system-exchange—retrospective analysis of 265 cases. PLoS One. 2014;9:e112316.
Gartner MJ, Wilhelm CR, Gage KL, Fabrizio MC, Wagner WR. Modeling flow effects on thrombotic deposition in a membrane oxygenator. Artif Organs. 2000;24:29–36.
Funakubo A, Taga I, McGillicuddy JW, Fukui Y, Hirschl RB, Bartlett RH. Flow vectorial analysis in an artificial implantable lung. ASAIO J. 2003;49:383–7.
Kaesler A, Rosen M, Schmitz-Rode T, Steinseifer U, Arens J. Computational modeling of oxygen transfer in artificial lungs. Artif Organs. 2018;42:786–99.
Eash HJ, Jones HM, Hattler BG, Federspiel WJ. Evaluation of plasma resistant hollow fiber membranes for artificial lungs. ASAIO J. 2004;50:491–7.
Svitek RG, Frankowski BJ, Federspiel WJ. Evaluation of a pumping assist lung that uses a rotating fiber bundle. ASAIO J. 2005;51:773–80.
Fernando UP, Thompson AJ, Potkay J, et al. A membrane lung design based on circular blood flow paths. ASAIO J. 2017;63:637–43.
Schmidt M, Jaber S, Zogheib E, Godet T, Capellier G, Combes A. Feasibility and safety of low-flow extracorporeal CO2 removal managed with a renal replacement platform to enhance lung-protective ventilation of patients with mild-to-moderate ARDS. Crit Care. 2018;22:122.
de Villiers Hugo J, Sharma AS, Ahmed U, Weerwind PW. Quantification of carbon dioxide removal at low sweep gas and blood flows. J Extra Corpor Technol. 2017;49:257–61.
Peperstraete H, Eloot S, Depuydt P, De Somer F, Roosens C, Hoste E. Low flow extracorporeal CO2 removal in ARDS patients: a prospective short-term crossover pilot study. BMC Anesthesiol. 2017;17:155.
Batchinsky AI, Jordan BS, Regn D, et al. Respiratory dialysis: reduction in dependence on mechanical ventilation by venovenous extracorporeal CO2 removal. Crit Care Med. 2011;39:1382–7.
Allardet-Servent J, Castanier M, Signouret T, Soundaravelou R, Lepidi A, Seghboyan JM. Safety and efficacy of combined extracorporeal CO2 removal and renal replacement therapy in patients with acute respiratory distress syndrome and acute kidney injury: The Pulmonary and Renal Support in Acute Respiratory Distress Syndrome Study. Crit Care Med. 2015;43:2570–81.
Burki NK, Mani RK, Herth FJF, et al. A novel extracorporeal CO(2) removal system: results of a pilot study of hypercapnic respiratory failure in patients with COPD. Chest. 2013;143:678–86.
Acknowledgements
We are grateful to Sascha Groß-Hardt, Institute of Applied Medical Engineering, Helmholtz Institute Aachen, RWTH Aachen University, Germany for his contribution to the current work. The current work was supported by the German Federal Ministry of Education and Research (13GW0219B; Verbundprojekt tragbare Langzeitunterstützung der Lunge zur Behandlung der schweren COPD [p-ECCO2R]).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Karagiannidis, C., Hesselmann, F., Fan, E. (2019). Physiological and Technical Considerations of Extracorporeal CO2 Removal. In: Vincent, JL. (eds) Annual Update in Intensive Care and Emergency Medicine 2019. Annual Update in Intensive Care and Emergency Medicine. Springer, Cham. https://doi.org/10.1007/978-3-030-06067-1_8
Download citation
DOI: https://doi.org/10.1007/978-3-030-06067-1_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-06066-4
Online ISBN: 978-3-030-06067-1
eBook Packages: MedicineMedicine (R0)