Abstract
Purpose
The stage of unstable dysfunction, also defined as “active discopathy” by Nguyen in 2015 and configuring the first phase of the degenerative cascade described by Kirkaldy-Willis, has specific pathoanatomical and clinical characteristics (low back pain) in the interested vertebral segment, without the presence of spondylolisthesis in flexion–extension radiography. This clinical condition has been defined as “microinstability” (MI). The term has currently not been recognized by the scientific community and is subject of debate for its diagnostic challenge. MI indicates a clinical condition in which the patient has a degeneration of the lumbar spine, causing low back pain, and radiological examinations do not show a spondylolisthesis.
Methods
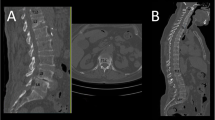
We elaborated a clinical score test based on preoperative radiological examinations (static and dynamic X-Rays, CT and MRI) to detect and assess MI. Then, we enrolled 74 patients, all the levels from L1 to S1 were analysed, for a total amount of 370 retrospectively analysed levels. We excluded patients with degenerative scoliosis, as it is related to an advanced stage of degeneration. The test has been developed with the aim of furnishing quantitative data on the basis of the aforementioned radiological examinations and of elaborating a diagnosis and a treatment for the degenerative pathology in dysfunctional phase, responsible for low back pain.
Results
We performed a statistical analysis on the results obtained from the test in terms of significativity and predictive value with a 1-year follow-up, calculating the p value and the χ 2 value.
Conclusions
In patients with low back pain and negative dynamic X-Rays, an accurate analysis of the radiological exams (CT, MRI, X-Rays) allows to formulate a diagnosis of suspect MI with a good predictive value. This situation opens many clinical and medicolegal scenarios. The preliminary results seem to validate the test with a good predictive value, especially towards ASD, but they need further studies. On the basis of the results obtained, the test seems to allow a good classification of the dysfunctional phase of the degenerative cascade, identifying and classifying MI as a pathologic entity, defining its pathoanatomical and clinical relevance and elaborating a treatment algorithm.


Similar content being viewed by others
References
Nguyen C, Poiraudeau S, Rannou F (2015) From Modic 1 vertebral-endplate subchondral bone signal changes detected by MRI to the concept of “active discopathy”. Ann Rheum Dis 74:1488–1494. doi:10.1136/annrheumdis-2015-207317
Kirkaldy-Willis WH, Farfan HF (1982) Instability of the lumbar spine. Clin Orthop Relat Res 165:110–123
Hancock MJ, Maher CM, Petocz P et al (2015) Risk factors for a recurrence of low back pain. Spine J. doi:10.1016/j.spinee.2015.07.007
Yochum TR, Rowe LJ (2004) Essentials of skeletal radiology. vol 1, 3rd edn. Lippincott editor
Griffith JF, Wang Y-XJ, Antonio GE et al (2007) Modified Pfirrmann grading system for lumbar intervertebral disc degeneration. Spine (Phila Pa 1976). doi:10.1097/BRS.0b013e31815a59a0
Yu LP, Qian WW, Yin GY et al (2012) MRI assessment of lumbar intervertebral disc degeneration with lumbar degenerative disease using the Pfirrmann grading systems. PLoS One 7:1–7. doi:10.1371/journal.pone.0048074
Bianchi M, Peterson CK, Pfirrmann CW et al (2015) Are the presence of MODIC changes on MRI scans related to “improvement” in low back pain patients treated with lumbar facet joint injections? BMC Musculoskelet Disord 16:234. doi:10.1186/s12891-015-0688-x
Rahme R, Moussa R (2008) The modic vertebral endplate and marrow changes: pathologic significance and relation to low back pain and segmental instability of the lumbar spine. Am J Neuroradiol 29:838–842. doi:10.3174/ajnr.A0925
Määttä JH, Karppinen JI, Luk KDK et al (2015) Phenotype profiling of Modic changes of the lumbar spine and its association with other MRI phenotypes: a large-scale population-based study. Spine J 15:1933–1942. doi:10.1016/j.spinee.2015.06.056
Chaput C, Padon D, Rush J et al (2007) The significance of increased fluid signal on magnetic resonance imaging in lumbar facets in relationship to degenerative spondylolisthesis. Spine (Phila Pa 1976) 32:1883–1887. doi:10.1097/BRS.0b013e318113271a
Mengiardi B, Schmid MR, Boos N et al (2006) Fat content of lumbar paraspinal muscles in patients with chronic low back pain and in asymptomatic volunteers: quantification with MR spectroscopy. Radiology 240:786–792. doi:10.1148/radiol.2403050820
Fujiwara A, Tamai K, Yamato M et al (1999) The relationship between facet joint osteoarthritis and disc degeneration of the lumbar spine: an MRI study. Eur Spine J 8:396–401 (90080396.586 [pii])
Fujiwara A, An HS, Lim TH, Haughton VM (2001) Morphologic changes in the lumbar intervertebral foramen due to flexion-extension, lateral bending, and axial rotation: an in vitro anatomic and biomechanical study. Spine (Phila Pa 1976) 26:876–882
Benneker LM, Heini PF, Anderson SE et al (2005) Correlation of radiographic and MRI parameters to morphological and biochemical assessment of intervertebral disc degeneration. Eur Spine J 14:27–35. doi:10.1007/s00586-004-0759-4
Djurasovic M, Carreon LY, Crawford CH et al (2012) The influence of preoperative MRI findings on lumbar fusion clinical outcomes. Eur Spine J 21:1616–1623. doi:10.1007/s00586-012-2244-9
Kanna RM, Shetty AP, Rajasekaran S (2014) Patterns of lumbar disc degeneration are different in degenerative disc disease and disc prolapse magnetic resonance imaging analysis of 224 patients. Spine J 14:300–307. doi:10.1016/j.spinee.2013.10.042
Shan Z, Li S, Liu J et al (2015) Correlation between biomechanical properties of the annulus fibrosus and magnetic resonance imaging (MRI) findings. Eur Spine J. doi:10.1007/s00586-015-4061-4
Dupuis PR, Yong-Hing K, Cassidy JD, Kirkaldy-Willis WH (1985) Radiologic diagnosis of degenerative lumbar spinal instability. Spine (Phila Pa 1976) 10:262–276
Landi A, Gregori F, Marotta N et al (2015) Hidden spondylolisthesis: unrecognized cause of low back pain? Prospective study about the use of dynamic projections in standing and recumbent position for the individuation of lumbar instability. Neuroradiology 57:583–588. doi:10.1007/s00234-015-1513-9
Landi A, Mancarella C, Delfini R (2014) What is the role of interspinous fusion devices (IFD) in the lumbar spine instability? J Spine Neurosurg S2 2–4. doi:10.4172/2325-9701.S2-e001
Landi A (2013) Elastic resistance of the spine: why does motion preservation surgery almost fail? World J Clin cases 1:134–139. doi:10.12998/wjcc.v1.i4.134
Landi A (2014) Interspinous posterior devices: what is the real surgical indication? World J Clin Cases 2:402. doi:10.12998/wjcc.v2.i9.402
Landi A, Delfini R (2014) Interspinous posterior devices IPD: a miracle cure for the lumbar spinal stenosis? Surg Curr Res. doi:10.4172/2161-1076.1000162
Landi A, Delfini R (2013) Soft stenosis of the lumbar spine: thickness vs hypertrophy of the ligamentum flavum. A pathogenetic and molecular point of view. J Spine. doi:10.4172/2165-7939.1000e111
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
N. Marotta is consultant for B-BRAUN.
Rights and permissions
About this article
Cite this article
Landi, A., Gregori, F., Mancarella, C. et al. Lumbar spinal degenerative “microinstability”: hype or hope? Proposal of a new classification to detect it and to assess surgical treatment. Eur Spine J 24 (Suppl 7), 872–878 (2015). https://doi.org/10.1007/s00586-015-4274-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-015-4274-6