Abstract
Interferon-gamma (IFNγ) has previously been associated with immuno-mediated inflammation in diet-induced obesity and type 1 diabetes. This study sought to define the role of IFNγ-induced adipose tissue inflammation in endothelial dysfunction in type 2 diabetes. We examined mesenteric adipose tissue (MAT) inflammation, and endothelial function of small mesenteric artery (SMA) in control mice (m Leprdb), diabetic mice (Leprdb), m Leprdb treated with IFNγ, and Leprdb treated with anti-IFNγ or anti-monocyte chemoattractant protein-1 (anti-MCP-1). mRNA and protein expression of IFNγ and MCP-1 were increased in MAT of Leprdb, accompanied by increased T-lymphocyte and macrophage infiltration. Anti-IFNγ reduced MAT inflammatory cell infiltration and inflammatory cytokine expression in Leprdb, while IFNγ treatment showed the opposite effects in m Leprdb. Acetylcholine (ACh)-induced vasorelaxation of SMA was impaired in Leprdb versus m Leprdb, but sodium nitroprusside (SNP)-induced vasorelaxation was comparable. Both anti-IFNγ and anti-MCP-1 improved endothelial function of Leprdb, while IFNγ treatment impaired endothelial function of m Leprdb. Superoxide production was higher in both MAT and SMA of Leprdb mice, and anti-IFNγ reduced MAT and SMA superoxide production. Macrophage accumulation in the adventitia of SMA, and mRNA expression of MCP-1 in SMA were increased in Leprdb and IFNγ-treated m Leprdb, but reduced in anti-IFNγ treated Leprdb. These findings suggest IFNγ has a key role in the regulation of visceral adipose tissue inflammatory response and endothelial dysfunction in type 2 diabetes.
Similar content being viewed by others
Introduction
The onset of an obesity and type 2 diabetes pandemic has gained wide recognition [21]. Increased adiposity, especially abdominal adiposity, is associated with an increase in cardiovascular risk factors [39], although the mechanisms underlying these associations are not well understood. Accumulating evidence suggests that adipose tissue plays a critical role in the regulation of vascular function by releasing relaxing and contracting factors, pro-inflammatory cytokines/chemokines, hormones, and superoxide [7, 12, 14, 15, 25]. The pathogenic role of adipose tissue in type 2 diabetes is supported by clinical evidence that weight loss leads to improvement in glycemic control [11]. Thus, characterization of the biological and pathological functions of various adipose-derived factors will expand our understanding of the communication between the peri-vascular adipose and blood vessels and how adipose tissue affects vascular function through endocrine/paracrine actions in obese and type 2 diabetic patients [7, 52].
Obesity and type 2 diabetes are characterized by low-grade systemic inflammation, which is caused, at least in part, by inflamed adipose tissue [52]. Adipocytes are intrinsically capable of producing various pro-inflammatory cytokines/chemokines. Furthermore, adipose tissue inflammation may also be due to macrophage that has been shown to infiltrate adipose tissue [18]. Increased macrophage infiltration into adipose tissue is associated with insulin resistance and endothelial dysfunction in obese subjects [1, 17]. T lymphocyte infiltration in visceral adipose tissue occurs prior to the infiltration of macrophage and the development of insulin resistance in high-fat diet treated mice [22]. Together, this suggests that T lymphocyte infiltration may be a primary event that orchestrates the inflammation of adipose tissue [4]. Both T cells and natural killer (NK) cells express interferon-gamma (IFNγ) on activation [6, 30]. Obese IFNγ-deficient animals showed significantly reduced densities of inflammatory cells in adipose tissue, and better glucose tolerance than control animals when fed with the same diet [37]. Despite the established role of IFNγ in mediating the immune response in type 1 diabetes and diet-induced obesity [6, 37], the role of IFNγ in inducing adipose tissue inflammation in type 2 diabetes and the mechanisms of the crosstalk between IFNγ-induced adipose tissue inflammation/oxidative stress and vascular dysfunction have not been studied. Thus, the objective of this study is to test the hypothesis that IFNγ-induced adipose tissue inflammation/oxidative stress is linked to endothelial dysfunction in type 2 diabetes. We examined the role of IFNγ in adipose tissue inflammation/oxidative stress and its vascular pro-oxidant mechanisms putatively involved in the increased oxidative stress/reduced generation of NO in type 2 diabetic mice.
Methods
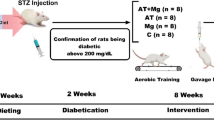
Animal models and treatment
The procedures followed were in accordance with approved guidelines set by the Animal Care Committee at the University of Missouri. Heterozygote control mice (m Leprdb) (Background Strain: C57BLKS/J), and homozygote type 2 diabetic mice (Leprdb) (Background Strain: C57BLKS/J) were purchased from Jackson Laboratory (Bar Harbor, Maine) and maintained on a normal rodent chow diet. 12–16 week-old, male, 20–35 g m Leprdb, and 40–60 g Leprdb mice were used in this study. m Leprdb was treated with murine recombinant IFNγ (R&D, Cat# 485-MI-100/CF, 330 μg/kg/day, i.p. injection, 5 days) [20]. Leprdb was treated with neutralizing antibody to IFNγ (anti-IFNγ, R&D, Cat#AF-485-NA, 250 μg/kg/day, i.p. injection, 4 days) or neutralizing antibody to MCP-1 (anti-MCP-1, Biovision, Cat#5225-100, 200 μg/kg/day, i.p. injection, 3 days) [35].
mRNA expression by real time polymerase chain reaction
Total RNA was extracted from mesenteric adipose tissue (MAT) or small mesenteric artery (SMA) samples using RNeasy Lipid Tissue Mini Kit (Qiagen) or RNeasy Plus Micro Kit (Qiagen), respectively. cDNA was amplified with the use of qRT-PCR Kit with SYBR® Green (Invitrogen). The primer sets were designed by Primer3 software [37, 41, 50]. Quantification was performed using the 2−∆∆CT method (∆∆CT = CT. target − CT. β-actin) [34]. Results were presented as fold change of transcripts for target normalized to internal control (β-actin), compared with m Leprdb (defined as 1.0 fold).
Protein expression by western blot analyses
Protein expression in MAT or SMA samples was detected using IFNγ primary antibody (Millipore, Cat#MAB1152, 1:500), MCP-1 primary antibody (Abcam, Cat#ab8101, 1:100), or nitrotyrosine primary antibody (Abcam, Cat#ab7048, 1:500). Signals were visualized by enhanced chemiluminescence (ECL, Santa Cruz), scanned densitometrically using Fuji LAS3000 and quantified with Multigauge software (Fujifilm).
Immunohistochemistry
MAT was fixed in 10% Z-fix, and embedded in paraffin. 5 μm sections were stained for rabbit anti-mouse CD3 (Abcam, Cat#ab16669, 1:200), rat anti-mouse F4/80 (Abcam, Cat#ab6640, 1:200), or rat anti-mouse Mac-3 (BD Bioscience, Cat#550292, 1:800), then incubated with appropriate biotinylated secondary antibodies followed by incubation with avidin–biotin complex (Vector). The reaction was visualized with 3-amino-9 ethyl carbazole (DAKO). Sections were counterstained with Gill’s hematoxylin solution (Sigma) [44].
Quantification of immunohistochemical staining data
The microscope (Leica CME) was set to 10× magnification and positive staining of macrophages accumulated in the adventitia of SMA was observed in consecutive fields of the entire section. The percentage of macrophage-positive SMA over the total number of SMA being counted for each sample was calculated and statistically analyzed.
Functional assessment of small mesenteric arteries
Mesenteric arteries (first order branches) with internal diameter of 200–250 μm were cut into 2 mm long rings and mounted on Myograph 610 M (A & D Instrument). The passive tension-internal circumference was determined by stretching to achieve an internal circumference equivalent to 60–70% of that of the blood vessel under a transmural pressure of 100 mmHg. A cumulative dose–response curve was obtained by adding acetylcholine (ACh, 1 nmol/L–10 μmol/L) and sodium nitroprusside (SNP, 1 nmol/L–10 μmol/L). Relaxation at each concentration was measured and expressed as the percentage of force generated in response to 1 μmol/L phenylephrine (PE) [32, 40]. NO availability and ROS production were evaluated by ACh concentration–response curve repeated after incubation with the NO synthase inhibitor N-Nitro-l-arginine methyl ester (L-NAME, 100 μmol/L, 20 min) and the anti-oxidant and superoxide dismutase mimetic TEMPOL (3 mmol/L, 60 min), respectively.
Measurement of superoxide using electron paramagnetic resonance spectroscopy
Measurement of superoxide using electron paramagnetic resonance spectroscopy (EPR) was performed as previously described [13, 49]. In brief, a 10% MAT or SMA tissue homogenate containing 2 mmol/L CPH (1-hydrox-3-carboxypyrrolidine) was prepared in a 50 mmol/L phosphate buffer with 0.01 mmol/L EDTA and were incubated for 30 min at 37°C and frozen quickly in liquid nitrogen for measurement.
Data analysis
All data were presented as mean ± SEM except as specifically stated. Statistical comparisons were performed with 2-way ANOVA for vasomotor responses under various treatments, and with one-way ANOVA for other data. Intergroup differences were tested with Fisher’s least significant difference test. Significance was accepted at P < 0.05. Expanded materials and methods are provided in the Online Supplement.
Results
Role of IFNγ in affecting body weight, visceral adiposity, glucose level and insulin sensitivity
Leprdb showed significantly higher body weight than m Leprdb. Abdominal girth, mesenteric bed weight and MAT adiposite size were increased in Leprdb versus m Leprdb. Fasting glucose level, insulin level and homeostasis model assessment of insulin resistance (HOMA-IR) were elevated in Leprdb mice compared with control mice. Insulin tolerance tests show impaired insulin sensitivity in diabetic mice versus control mice. Anti-IFNγ and IFNγ treatment exerted no effects on the above parameters (Supplementary Table 1 and Supplementary Fig. 1).
Role of IFNγ in adipose tissue inflammation in type 2 diabetic mice
IFNγ mRNA and protein expression were higher in MAT of Leprdb versus m Leprdb. Anti-IFNγ reduced mRNA and protein expression of IFNγ in Leprdb. IFNγ treatment to m Leprdb increased mRNA expression of IFNγ, but did not significantly affect protein expression of IFNγ in MAT. MCP-1 mRNA and protein expression were also higher in MAT of diabetic mice versus control mice. Anti-MCP-1 treatment reduced both mRNA and protein expression of MCP-1 in Leprdb. Although anti-IFNγ treatment ameliorated MCP-1 expression, anti-MCP-1 did not significantly affect mRNA and protein expression of IFNγ (Fig. 1). In addition to IFNγ and MCP-1, we also examined the mRNA expression of other adipose-derived factors in MAT of control and diabetic mice. The results indicate there were no differences in MAT mRNA expression of adiponectin, interleukin-10 (IL-10), RANTES, IL-6, and monokine induced by gamma-interferon (MIG) between control and diabetic mice (Supplemental Fig. 2).
The mRNA and Protein Expression of IFNγ and MCP-1 in MAT by qRT-PCR and western blot mRNA and protein expression of IFNγ (a, b) and MCP-1 (c, d) were increased in mesenteric adipose tissue (MAT) of Leprdb versus m Leprdb. Treatment of anti-IFNγ reduced IFNγ and MCP-1 expression in Leprdb, but treatment by recombinant IFNγ show opposite effects in control mice. Anti-MCP-1 reduced the expression of MCP-1, but not IFNγ in MAT of Leprdb mice. Results in various groups were normalized to those of the corresponding m Leprdb control, which were set to a value of 1.0. Data were shown as mean ± SEM. n = 4 separate experiments. *p < 0.05 versus m Leprdb mice, # p < 0.05 versus Leprdb mice
We examined the infiltration of CD3 positive T lymphocytes, F4/80 and Mac-3 positive macrophages in MAT of m Leprdb, Leprdb, Leprdb treated with anti-IFNγ or anti-MCP-1, and m Leprdb treated with IFNγ using immunohistochemical staining. Multiple macrophages and lymphocytes fused around dead adipocytes to form crown-like structures (CLS), which were prevalent in MAT of Leprdb (Fig. 2a). mRNA expression of CD3, CD4, CD8, and CD68 was increased in MAT of Leprdb versus control mice. Anti-IFNγ reduced mRNA expression of T lymphocyte and macrophage markers, while IFNγ increased the mRNA levels of CD3, CD4, CD8, and CD68 in m Leprdb mice. Anti-MCP-1 reduced macrophage infiltration, but did not significantly affect MAT T lymphocyte infiltration in Leprdb mice (Fig. 2b–e).
Inflammatory cell infiltration in adipose tissue. a Immunohistochemical staining of T-lymphocyte marker CD3, macrophage marker F4/80 and Mac-3 in MAT. T-lymphocyte and macrophage accumulation was increased in the MAT of diabetic mice. Anti-IFNγ reduced T-lymphocyte/macrophage infiltration, and treatment of m Leprdb mice with IFNγ increased MAT T-lymphocyte/macrophage infiltration. n = 4 separate experiments. mRNA expression of T cell markers, CD3 (b), CD4 (c), CD8 (d), and macrophage marker CD68 (e) were higher in MAT of Leprdb mice. Anti-IFNγ reduced the mRNA expression of T cell and macrophage markers in diabetic mice, while IFNγ treatment increased their levels in control mice. Anti-MCP-1 reduced CD68 mRNA expression without significantly affecting the level of T cell markers. n = 4 separate experiments. Data were shown as mean ± SEM. *p < 0.05 versus m Leprdb; # p < 0.05 versus Leprdb. f mRNA expression of CD68 in periaortic adipose tissue (PAT), interscapular brown adipose tissue (BAT), epididymal white adipose tissue (EWAT), and inguinal subcutaneous adipose tissue (SCAT) was examined by quantitative RT-PCR and was normalized to the CD68 level in MAT of m Leprdb control mice. n = 4–8 separate experiments. Data were shown as mean ± SEM. CD68 expression in each adipose tissue depot expressed as: *p < 0.05 versus m Leprdb; # p < 0.05 versus Leprdb
The expression of macrophage marker CD68 in peri-aortic adipose tissue (PAT) and interscapular brown adipose tissue (BAT) was relatively lower compared with that in MAT in all groups, and there were no statistical differences in PAT and BAT CD68 expression between control and diabetic mice. However, CD68 expression in epididymal white adipose tissue (EWAT) and inguinal subcutaneous adipose tissue (SCAT) was significantly higher in diabetic mice and IFNγ-treated control mice, but anti-IFNγ treatment to diabetic mice only minimally reduced the CD68 expression in EWAT and SCAT (Fig. 2f).
Role of IFNγ in endothelial dysfunction in type 2 diabetic mice
Endothelium-dependent vasorelaxation of SMA to ACh was impaired in Leprdb versus m Leprdb (Fig. 3). Anti-IFNγ and anti-MCP-1 improved endothelial function of Leprdb, but IFNγ impaired ACh-induced vasorelaxation of control mice (Fig. 3a, c). The endothelium-independent vasorelaxation to sodium nitroprusside (SNP) and vasoconstriction to PE were identical among all groups (Fig. 3b, d and Supplemental Fig. 3).
Endothelium-dependent and Endothelium-independent vasorelaxation of SMA. a, c ACh-induced endothelium-dependent vasorelaxation of SMA was impaired in Leprdb. Anti-IFNγ and anti-MCP-1 improved endothelial function, but treatment of control mice with IFNγ impaired endothelial function. b, d SNP-induced endothelium-independent vasorelaxation was not different among groups. Data were shown as mean ± SEM. n = 6–13 rings from 6–8 mice. *p < 0.05 versus m Leprdb mice, # p < 0.05 versus Leprdb mice
TEMPOL incubation restored the endothelial function of Leprdb back to the level of control mice (Fig. 4a). L-NAME incubation abolished the difference in endothelium-dependent vasorelaxation between control and diabetic mice (Fig. 4b).
The role of superoxide anion and nitric oxide (NO) in the regulation of endothelial function of SMA. a TEMPOL incubation (3 mmol/L, 60 min) restored impaired endothelial function in Leprdb. n = 8 rings from 6 mice. b Endothelium-dependent vasorelaxation was identical between control and diabetic mice after L-NAME incubation (100 μmol/L, 20 min). n = 11–16 rings from 7–10 mice. Data were shown as mean ± SEM. *p < 0.05 versus m Leprdb mice, # p < 0.05 versus Leprdb mice
The link between adipose tissue inflammation/oxidative stress and endothelial dysfunction in type 2 diabetic mice
The accumulation of Mac-3 positive macrophages in the adventitia of SMA vascular wall was higher in diabetic mice versus control mice. Anti-IFNγ reduced macrophage accumulation in SMA of Leprdb mice, but IFNγ showed opposite effects in control mice (Fig. 5a, b). Moreover, the mRNA expression of MCP-1 was higher in the SMA of diabetic mice. Anti-IFNγ reduced mRNA expression of MCP-1 in SMA of Leprdb mice, but IFNγ treatment to control mice increased SMA MCP-1 expression (Fig. 5c). However, the mRNA expression of VCAM-1, ICAM-1 and E-selectin in SMA was not different between control and diabetic mice (Supplements Fig. 4). Serum level of MCP-1 was comparable in diabetic and control mice (Fig. 5d). Serum level of inflammatory cytokine tumor necrosis factor-alpha (TNFα) was elevated in diabetic mice and control mice treated with IFNγ (Fig. 5e).
The Accumulation of Macrophages and the mRNA Expression of MCP-1 in the Vascular Wall of SMA, and the Serum Level of MCP-1 and TNFα a Mac-3 positive macrophage accumulation in the vascular wall of SMA was increased in Leprdb and m Leprdb treated with IFNγ. Anti-IFNγ reduced macrophage accumulation in SMA vascular wall. b The percentage of SMA with Mac-3 positive macrophage accumulation was quantified. n = 4 separate experiments. c mRNA expression of MCP-1 in SMA was higher in diabetic mice versus control mice. Anti-IFNγ reduced MCP-1 expression in SMA of diabetic mice. n = 8 separate experiments. d Serum level of MCP-1 was not different among m Leprdb, Leprdb, and m Leprdb + IFNγ. e Serum level of TNFα was higher in Leprdb and m Leprdb + IFNγ versus m Leprdb. n = 4–6 mice. Data were shown as mean ± SEM. *p < 0.05 versus m Leprdb mice, # p < 0.05 versus Leprdb mice
Superoxide production was elevated in both MAT and SMA of diabetic mice. Anti-IFNγ and anti-MCP-1 ameliorated both MAT and SMA superoxide production, while IFNγ increased MAT/SMA superoxide levels (Fig. 6a, b). Moreover, nitrotyrosine protein expression was higher in SMA of diabetic mice. Both anti-IFNγ and anti-MCP-1 decreased nitrotyrosine levels in SMA of Leprdb, but IFNγ treatment to m Leprdb increased SMA nitrotyrosine protein expression (Fig. 6c).
Oxidative stress in MAT and SMA a, b Superoxide levels measured by EPR were increased in MAT and SMA of Leprdb compared with m Leprdb control mice. Anti-IFNγ reduced MAT/SMA superoxide level in Leprdb, but IFNγ treatment increased MAT/SMA superoxide production in m Leprdb. Data represent mean ± SEM. n = 6–12 mice. *p < 0.05 versus m Leprdb mice, # p < 0.05 versus Leprdb mice. c Nitrotyrosine (N-Tyr) expression measured by Western Blotting was higher in SMA of diabetic mice. Anti-IFNγ and anti-MCP-1 reduced SMA expression of N-Tyr, while IFNγ showed the opposite effects in control mice SMA. Data represent blots from three separate experiments
Discussion
Endothelial dysfunction is an important factor in the pathogenesis of cardiovascular disorders and has gained increasing attention in the study of obesity and diabetes-associated vascular complications [3, 16, 31]. Central adiposity, particularly a greater amount of intra-abdominal or visceral fat, contributes to chronic sub-clinical inflammation, which is linked to endothelial dysfunction and atherosclerosis [43]. The study of the paracrine/endocrine effects of inflamed adipose tissue on the regulation of vascular function will further enhance our understanding of the mechanisms involved in diabetes-associated vascular complications. The major findings in this study are: (1) IFNγ expression is increased in MAT of type 2 diabetic mice; (2) IFNγ induces visceral adipose tissue inflammation/oxidative stress in control mice; (3) IFNγ increases macrophage accumulation and MCP-1 expression in the vascular wall and impairs endothelial function of SMA; (4) Anti-IFNγ ameliorates MAT inflammation/oxidative stress and improves SMA endothelial function in type 2 diabetic mice. We posit that IFNγ is a mechanism for the generation of inflammation and oxidative stress derived from adipose tissue and plays an important role in the regulation of endothelial function.
T lymphocyte/macrophage infiltration and adipose tissue inflammation in type 2 diabetic mice
Obesity is associated with inflammatory cell accumulation in the adipose tissue [46]. Diet-induced increases in adiposity promote macrophage infiltration into white adipose tissue and the extent of macrophage accumulation correlates with the degree of adiposity [8]. In addition to macrophages, T lymphocytes have recently been identified as a key player in adipose tissue inflammation by orchestrating the evolution of the inflammatory cascade [29]. In patients with type 2 diabetes, lymphocyte content in adipose tissue biopsies is significantly correlated with waist circumference, a marker of central adiposity, and insulin resistance [22]. Our results suggest that the increased IFNγ expression in MAT in Leprdb was accompanied by enhanced T lymphocyte/macrophage infiltration. Immunohistochemical staining generally showed T lymphocytes in clusters with macrophages, which formed CLS around adipocytes. Anti-IFNγ reduced MAT IFNγ and MCP-1 expression, as well as the T lymphocyte and macrophage infiltration. Anti-MCP-1 reduced macrophage infiltration, but did not significantly affect IFNγ expression and T lymphocyte infiltration (Figs. 1, 2). Thus, although T lymphocytes are quantitatively less prominent than macrophages [37], T cells may decisively affect the infiltration of macrophages, and the expression of macrophage-derived chemokines, in the visceral adipose tissue of type 2 diabetic mice.
Adipose tissue inflammation and endothelial dysfunction in type 2 diabetic mice
Growing evidence suggests a link between adipose tissue inflammation and endothelial dysfunction [1, 26]. The production of inflammatory cytokines and hormones by adipose tissue is of particular interest, since their local secretion by peri-vascular adipose deposits may provide a novel mechanistic link between obesity and diabetes-associated vascular complications [5, 7, 19]. The secretory products from human adipocytes stimulated pro-inflammatory cytokine secretion by human umbilical venous endothelial cells (HUVECs), suggesting that endothelial cell secretion was significantly tilted towards a pro-inflammatory pattern by adipocyte-derived factors [9, 38]. Moreover, macrophages stimulated with IFNγ activate nuclear factor-kappa B (NF-Kb) and induce MCP-1 gene expression in HUVECs, which posits to a possible interaction between adipose inflammatory cells and vascular cells [36]. Mesenteric vasculature regulates total blood flow to the gut and mediates transport of nutrients in the circulation [24]. The mesenteric bed is surrounded by a variable volume of peri-vascular mesenteric adipose tissue, which plays an important role in sustaining an inflammation cascade in obesity and type 2 diabetes [14]. Changes in the fat may have consequences for the regulation of mesenteric artery tone and mesenteric endothelial function [12]. Thus, SMA is an ideal model to study the possible local effects of MAT inflammation on vascular function.
Oxidative stress and inflammation are known to be the key mechanisms in the pathogenesis of vascular dysfunction in atherosclerosis, myocardial ischemia/reperfusion, and diabetes [2, 42, 45, 48]. Many adipose-derived cytokines, such as IL-6, TNFα, and MCP-1 profoundly stimulate ROS production and reduce NO bioavailability [23, 33, 52, 53]. Our results show that ACh-induced vasorelaxation was impaired in SMA of Leprdb. This impairment was completely restored by SOD mimetic, TEMPOL, incubation (Fig. 4a). L-NAME incubation abolished the difference in endothelium-dependent vasorelaxation between control and diabetic mice (Fig. 4b), supporting the view that the impairment of endothelial function in Leprdb was mediated by ROS and NO bioavailability. Furthermore, SMA superoxide production and nitrotyrosine protein expression were higher in Leprdb versus m Leprdb. Anti-IFNγ and anti-MCP-1 reduced SMA superoxide and nitrotyrosine expression, while IFNγ showed the opposite effects in m Leprdb (Fig. 6).
The profound MAT oxidative stress and macrophage accumulation in the vascular wall of SMA may serve as link between MAT inflammation and SMA endothelial dysfunction. In Leprdb mice, the superoxide production is elevated in both MAT and SMA. By normalizing the superoxide level of MAT/SMA to the protein content, the superoxide production is quantitatively more prominent in MAT than in SMA (Fig. 6a, b). Anti-IFNγ reduced MAT superoxide production in Leprdb, but IFNγ increased MAT oxidative stress in m Leprdb mice (Fig. 6a). Moreover, macrophage accumulation in the adventitia of mesenteric vessels was significantly higher in Leprdb and m Leprdb treated with IFNγ. Leprdb treated with anti-IFNγ showed reduced macrophage accumulation in SMA. mRNA expression of MCP-1 was also elevated in the SMA of diabetic mice and anti-IFNγ treatment attenuated the MCP-1 expression in SMA (Fig. 5c). Importantly, compared with the remarkable impairment of SMA endothelial function following IFNγ systemic in vivo administration, in vitro incubation of the adipose-free vessel with a pathological concentration of murine recombinant IFNγ (1.6 or 16 ng/ml for 1 h, or 16 ng/ml for 4 h) did not significantly affect ACh-dependent SMA vasorelaxation (Supplemental Fig. 5). This suggests that the role of IFNγ in the impairment of vascular function occurs indirectly following IFNγ-induced adipose tissue inflammation.
Separating the local versus systemic effects of adipose tissue on the regulation of vascular function is also important. Although adipose tissue is considered as a potential systemic source of inflammation, only a limited number of adipose-derived cytokines are released into the circulation in sufficient amounts to account for obesity-associated increased systemic levels [28]. The trivial contribution of adipose-derived MCP-1 [10], TNFα [27], and PAI-1 [47] to the circulating concentrations has been demonstrated by measuring the arteriovenous difference over the inferior epigastric vein [28]. In fact, although MCP-1 expression was increased in Leprdb MAT, the serum level of MCP-1 was not statistically different between control and diabetic mice (Fig. 5d). The serum level of TNFα was higher in diabetic mice and IFNγ-treated control mice (Fig. 5e). However, as a chronic disease model, the circulating concentration of TNFα in the pg/ml range is unlikely to cause endothelial dysfunction in type 2 diabetic mice [51]. Therefore, mesenteric adipose tissue exhibiting a pro-inflammatory phenotype may primarily exert local effects by promoting inflammatory cell accumulation and the release of inflammatory cytokines, thereby enhancing vascular inflammation/oxidative stress and attenuating endothelial function.
In conclusion, our study suggests that IFNγ-induced adipose tissue inflammation and oxidative stress is linked to endothelial dysfunction in type 2 diabetes. These findings help define the linkage between adipose tissue inflammation and vascular dysfunction and highlight the therapeutic potential of anti-IFNγ for alleviating diabetes-related vascular complications, which may result in better remediation strategies in the longer term.
References
Apovian CM, Bigornia S, Mott M, Meyers MR, Ulloor J, Gagua M, McDonnell M, Hess D, Joseph L, Gokce N (2008) Adipose macrophage infiltration is associated with insulin resistance and vascular endothelial dysfunction in obese subjects. Arterioscler Thromb Vasc Biol 28:1654–1659. doi:10.1161/ATVBAHA.108.170316
Becker BF, Chappell D, Jacob M (2010) Endothelial glycocalyx and coronary vascular permeability: the fringe benefit. Basic Res Cardiol 105:687–701. doi:10.1007/s00395-010-0118-z
Belin de Chantemele EJ, Ali MI, Mintz J, Stepp DW (2009) Obesity induced-insulin resistance causes endothelial dysfunction without reducing the vascular response to hind limb ischemia. Basic Res Cardiol 104:707–717. doi:10.1007/s00395-009-0042-2
Bouloumie A, Casteilla L, Lafontan M (2008) Adipose tissue lymphocytes and macrophages in obesity and insulin resistance: makers or markers, and which comes first? Arterioscler Thromb Vasc Biol 28:1211–1213. doi:10.1161/ATVBAHA.108.168229
Calabro P, Limongelli G, Pacileo G, Di Salvo G, Golino P, Calabro R (2008) The role of adiposity as a determinant of an inflammatory milieu. J Cardiovasc Med (Hagerstown) 9:450–460. doi:10.2459/JCM.0b013e3282eee9a8
Calderon B, Suri A, Pan XO, Mills JC, Unanue ER (2008) IFN-gamma-dependent regulatory circuits in immune inflammation highlighted in diabetes. J Immunol 181:6964–6974
Chatterjee TK, Stoll LL, Denning GM, Harrelson A, Blomkalns AL, Idelman G, Rothenberg FG, Neltner B, Romig-Martin SA, Dickson EW, Rudich S, Weintraub NL (2009) Proinflammatory phenotype of perivascular adipocytes: influence of high-fat feeding. Circ Res 104:541–549. doi:10.1161/CIRCRESAHA.108.182998
Coenen KR, Gruen ML, Chait A, Hasty AH (2007) Diet-induced increases in adiposity, but not plasma lipids, promote macrophage infiltration into white adipose tissue. Diabetes 56:564–573. doi:10.2337/db06-1375
Curat CA, Miranville A, Sengenes C, Diehl M, Tonus C, Busse R, Bouloumie A (2004) From blood monocytes to adipose tissue-resident macrophages: induction of diapedesis by human mature adipocytes. Diabetes 53:1285–1292
Dahlman I, Kaaman M, Olsson T, Tan GD, Bickerton AS, Wahlen K, Andersson J, Nordstrom EA, Blomqvist L, Sjogren A, Forsgren M, Attersand A, Arner P (2005) A unique role of monocyte chemoattractant protein 1 among chemokines in adipose tissue of obese subjects. J Clin Endocrinol Metab 90:5834–5840. doi:10.1210/jc.2005-0369
Feldstein AC, Nichols GA, Smith DH, Stevens VJ, Bachman K, Rosales AG, Perrin N (2008) Weight change in diabetes and glycemic and blood pressure control. Diabetes Care 31:1960–1965. doi:10.2337/dc08-0426
Galvez B, de Castro J, Herold D, Dubrovska G, Arribas S, Gonzalez MC, Aranguez I, Luft FC, Ramos MP, Gollasch M, Fernandez Alfonso MS (2006) Perivascular adipose tissue and mesenteric vascular function in spontaneously hypertensive rats. Arterioscler Thromb Vasc Biol 26:1297–1302. doi:10.1161/01.ATV.0000220381.40739.dd
Gao X, Belmadani S, Picchi A, Xu X, Potter BJ, Tewari-Singh N, Capobianco S, Chilian WM, Zhang C (2007) Tumor necrosis factor-alpha induces endothelial dysfunction in Leprdb mice. Circulation 115:245–254. doi:10.1161/CIRCULATIONAHA.106.650671
Gao YJ (2007) Dual modulation of vascular function by perivascular adipose tissue and its potential correlation with adiposity/lipoatrophy-related vascular dysfunction. Curr Pharm Des 13:2185–2192
Gao YJ, Takemori K, Su LY, An WS, Lu C, Sharma AM, Lee RM (2006) Perivascular adipose tissue promotes vasoconstriction: the role of superoxide anion. Cardiovasc Res 71:363–373. doi:10.1016/j.cardiores.2006.03.013
Ghaboura N, Tamareille S, Ducluzeau PH, Grimaud L, Loufrani L, Croue A, Tourmen Y, Henrion D, Furber A, Prunier F (2011) Diabetes mellitus abrogates erythropoietin-induced cardioprotection against ischemic-reperfusion injury by alteration of the RISK/GSK-3beta signaling. Basic Res Cardiol 106:147–162. doi:10.1007/s00395-010-0130-3
Hansen T, Ahlstrom H, Soderberg S, Hulthe J, Wikstrom J, Lind L, Johansson L (2009) Visceral adipose tissue, adiponectin levels and insulin resistance are related to atherosclerosis as assessed by whole-body magnetic resonance angiography in an elderly population. Atherosclerosis 205:163–167. doi:10.1016/j.atherosclerosis.2008.11.007
Heilbronn LK, Campbell LV (2008) Adipose tissue macrophages, low grade inflammation and insulin resistance in human obesity. Curr Pharm Des 14:1225–1230
Heusch G (2006) Obesity–a risk factor or a RISK factor for myocardial infarction? Br J Pharmacol 149:1–3. doi:10.1038/sj.bjp.0706833
Jackson SH, Miller GF, Segal BH, Mardiney M 3rd, Domachowske JB, Gallin JI, Holland SM (2001) IFN-gamma is effective in reducing infections in the mouse model of chronic granulomatous disease (CGD). J Interferon Cytokine Res 21:567–573. doi:10.1089/10799900152547821
Karam JG, McFarlane SI (2008) Prevention of type 2 DM: implications for adolescents and young adults. Pediatr Endocrinol Rev 5(Suppl 4):980–988
Kintscher U, Hartge M, Hess K, Foryst-Ludwig A, Clemenz M, Wabitsch M, Fischer-Posovszky P, Barth TF, Dragun D, Skurk T, Hauner H, Bluher M, Unger T, Wolf AM, Knippschild U, Hombach V, Marx N (2008) T-lymphocyte infiltration in visceral adipose tissue: a primary event in adipose tissue inflammation and the development of obesity-mediated insulin resistance. Arterioscler Thromb Vasc Biol 28:1304–1310. doi:10.1161/ATVBAHA.108.165100
Kleinbongard P, Heusch G, Schulz R (2010) TNFalpha in atherosclerosis, myocardial ischemia/reperfusion and heart failure. Pharmacol Ther 127:295–314. doi:10.1016/j.pharmthera.2010.05.002
Lanciault G, Jacobson ED (1976) The gastrointestinal circulation. Gastroenterology 71:851–873
Marchesi C, Ebrahimian T, Angulo O, Paradis P, Schiffrin EL (2009) Endothelial nitric oxide synthase uncoupling and perivascular adipose oxidative stress and inflammation contribute to vascular dysfunction in a rodent model of metabolic syndrome. Hypertension 54:1384–1392. doi:10.1161/HYPERTENSIONAHA.109.138305
Marchesi S, Vaudo G, Lupattelli G, Lombardini R, Roscini AR, Brozzetti M, Siepi D, Mannarino E (2007) Fat distribution and endothelial function in normal-overweight menopausal women. J Clin Pharm Ther 32:477–482. doi:10.1111/j.1365-2710.2007.00856.x
Mohamed-Ali V, Goodrick S, Rawesh A, Katz DR, Miles JM, Yudkin JS, Klein S, Coppack SW (1997) Subcutaneous adipose tissue releases interleukin-6, but not tumor necrosis factor-alpha, in vivo. J Clin Endocrinol Metab 82:4196–4200
Murdolo G, Hammarstedt A, Sandqvist M, Schmelz M, Herder C, Smith U, Jansson PA (2007) Monocyte chemoattractant protein-1 in subcutaneous abdominal adipose tissue: characterization of interstitial concentration and regulation of gene expression by insulin. J Clin Endocrinol Metab 92:2688–2695. doi:10.1210/jc.2006-2814
Nishimura S, Manabe I, Nagasaki M, Eto K, Yamashita H, Ohsugi M, Otsu M, Hara K, Ueki K, Sugiura S, Yoshimura K, Kadowaki T, Nagai R (2009) CD8 + effector T cells contribute to macrophage recruitment and adipose tissue inflammation in obesity. Nat Med 15:914–920. doi:10.1038/nm.1964
O’Rourke RW, Metcalf MD, White AE, Madala A, Winters BR, Maizlin II, Jobe BA, Roberts CT Jr, Slifka MK, Marks DL (2009) Depot-specific differences in inflammatory mediators and a role for NK cells and IFN-gamma in inflammation in human adipose tissue. Int J Obes (Lond) 33:978–990. doi:10.1038/ijo.2009.133
Orlandi A, Chavakis E, Seeger F, Tjwa M, Zeiher AM, Dimmeler S (2010) Long-term diabetes impairs repopulation of hematopoietic progenitor cells and dysregulates the cytokine expression in the bone marrow microenvironment in mice. Basic Res Cardiol 105:703–712. doi:10.1007/s00395-010-0109-0
Pannirselvam M, Wiehler WB, Anderson T, Triggle CR (2005) Enhanced vascular reactivity of small mesenteric arteries from diabetic mice is associated with enhanced oxidative stress and cyclooxygenase products. Br J Pharmacol 144:953–960. doi:10.1038/sj.bjp.0706121
Park Y, Yang J, Zhang H, Chen X, Zhang C (2011) Effect of PAR2 in regulating TNF-alpha and NAD(P)H oxidase in coronary arterioles in type 2 diabetic mice. Basic Res Cardiol 106:111–123. doi:10.1007/s00395-010-0129-9
Pfaffl MW (2001) A new mathematical model for relative quantification in real-time RT-PCR. Nucleic Acids Res 29:e45
Plotnicky-Gilquin H, Cyblat-Chanal D, Aubry JP, Champion T, Beck A, Nguyen T, Bonnefoy JY, Corvaia N (2002) Gamma interferon-dependent protection of the mouse upper respiratory tract following parenteral immunization with a respiratory syncytial virus G protein fragment. J Virol 76:10203–10210
Rimbach G, Valacchi G, Canali R, Virgili F (2000) Macrophages stimulated with IFN-gamma activate NF-kappa B and induce MCP-1 gene expression in primary human endothelial cells. Mol Cell Biol Res Commun 3:238–242. doi:10.1006/mcbr.2000.0219
Rocha VZ, Folco EJ, Sukhova G, Shimizu K, Gotsman I, Vernon AH, Libby P (2008) Interferon-gamma, a Th1 cytokine, regulates fat inflammation: a role for adaptive immunity in obesity. Circ Res 103:467–476. doi:10.1161/CIRCRESAHA.108.177105
Sommer G, Kralisch S, Stangl V, Vietzke A, Kohler U, Stepan H, Faber R, Schubert A, Lossner U, Bluher M, Stumvoll M, Fasshauer M (2009) Secretory products from human adipocytes stimulate proinflammatory cytokine secretion from human endothelial cells. J Cell Biochem 106:729–737. doi:10.1002/jcb.22068
Stein AD, Conlisk A, Torun B, Schroeder DG, Grajeda R, Martorell R (2002) Cardiovascular disease risk factors are related to adult adiposity but not birth weight in young guatemalan adults. J Nutr 132:2208–2214
Su J, Lucchesi PA, Gonzalez-Villalobos RA, Palen DI, Rezk BM, Suzuki Y, Boulares HA, Matrougui K (2008) Role of advanced glycation end products with oxidative stress in resistance artery dysfunction in type 2 diabetic mice. Arterioscler Thromb Vasc Biol 28:1432–1438. doi:10.1161/ATVBAHA.108.167205
Tanaka Y, Koido S, Xia J, Ohana M, Liu C, Cote GM, Sawyer DB, Calderwood S, Gong J (2004) Development of antigen-specific CD8 + CTL in MHC class I-deficient mice through CD4 to CD8 conversion. J Immunol 172:7848–7858
Tiyerili V, Zimmer S, Jung S, Wassmann K, Naehle CP, Lutjohann D, Zimmer A, Nickenig G, Wassmann S (2010) CB1 receptor inhibition leads to decreased vascular AT1 receptor expression, inhibition of oxidative stress and improved endothelial function. Basic Res Cardiol 105:465–477. doi:10.1007/s00395-010-0090-7
Wexler DJ, Hu FB, Manson JE, Rifai N, Meigs JB (2005) Mediating effects of inflammatory biomarkers on insulin resistance associated with obesity. Obes Res 13:1772–1783. doi:10.1038/oby.2005.216
Whiteland JL, Nicholls SM, Shimeld C, Easty DL, Williams NA, Hill TJ (1995) Immunohistochemical detection of T-cell subsets and other leukocytes in paraffin-embedded rat and mouse tissues with monoclonal antibodies. J Histochem Cytochem 43:313–320
Wu J, Li J, Zhang N, Zhang C (2011) Stem cell-based therapies in ischemic heart diseases: a focus on aspects of microcirculation and inflammation. Basic Res Cardiol 106:317–324. doi:10.1007/s00395-011-0168-x
Xu H, Barnes GT, Yang Q, Tan G, Yang D, Chou CJ, Sole J, Nichols A, Ross JS, Tartaglia LA, Chen H (2003) Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. J Clin Invest 112:1821–1830. doi:10.1172/JCI19451
Yudkin JS, Coppack SW, Bulmer K, Rawesh A, Mohamed-Ali V (1999) Lack of evidence for secretion of plasminogen activator inhibitor-1 by human subcutaneous adipose tissue in vivo. Thromb Res 96:1–9. doi:S0049-3848(99)00061-4[pii]
Zhang C, Wu J, Xu X, Potter BJ, Gao X (2010) Direct relationship between levels of TNF-alpha expression and endothelial dysfunction in reperfusion injury. Basic Res Cardiol 105:453–464. doi:10.1007/s00395-010-0083-6
Zhang C, Xu X, Potter BJ, Wang W, Kuo L, Michael L, Bagby GJ, Chilian WM (2006) TNF-alpha contributes to endothelial dysfunction in ischemia/reperfusion injury. Arterioscler Thromb Vasc Biol 26:475–480. doi:01.ATV.0000201932.32678.7e[pii]10.1161/01.ATV.0000201932.32678.7e
Zhang H, Park Y, Zhang C (2010) Coronary and aortic endothelial function affected by feedback between adiponectin and tumor necrosis factor alpha in type 2 diabetic mice. Arterioscler Thromb Vasc Biol 30:2156–2163. doi:10.1161/ATVBAHA.110.214700
Zhang H, Wang Y, Zhang J, Potter BJ, Sowers JR, Zhang C (2011) Bariatric Surgery Reduces Visceral Adipose Inflammation and Improves Endothelial Function in Type 2 Diabetic Mice. Arterioscler Thromb Vasc Biol 10.1161/ATVBAHA.111.225870
Zhang H, Zhang C (2010) Adipose “Talks” to distant organs to regulate insulin sensitivity and vascular function. Obesity (Silver Spring) 18(11):2071–2076. doi:10.1038/oby.2010.91
Zhang H, Zhang C (2009) Regulation of microvascular function by adipose tissue in obesity and type 2 diabetes: evidence of an adipose-vascular loop. Am J Biomed Sci 1:133–142
Acknowledgments
This study was supported by grants from NIH grants (RO1-HL077566 and RO1-HL085119, to C.Z., R01-DK085495 to J Ye and C.Z. and RO1-HL073101 to J Sowers and C.Z.) and American Heart Association Pre-doctoral Fellowship (10PRE4300043 to H.Z.).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhang, H., Potter, B.J., Cao, JM. et al. Interferon-gamma induced adipose tissue inflammation is linked to endothelial dysfunction in type 2 diabetic mice. Basic Res Cardiol 106, 1135–1145 (2011). https://doi.org/10.1007/s00395-011-0212-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00395-011-0212-x