Abstract
Purpose
This study was designed to assess the enhanced effect of high intensity focused ultrasound (HIFU) ablation with microbubbles on rabbit hepatic VX2 tumors and to compare the detection sensitivity of CEUS and CECT to determine the residual viable tissue after ablation of HIFU.
Methods
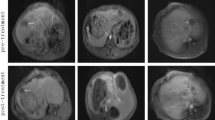
Forty rabbits with hepatic VX2 tumors were randomly separated into two groups (20 animals per group) before HIFU ablation. A bolus of 0.2 mL of saline or a microbubble-based ultrasound (US) contrast agent was injected intravenously to group I rabbits and group II rabbits, respectively. The HIFU ablation procedure was started 15 s after the injection. Tumors were examined with grayscale contrast-enhanced ultrasound (CEUS) and contrast-enhanced computed tomography (CECT) immediately before and after HIFU ablation. Histopathologic assessment was performed immediately after treatment imaging.
Results
Before ablation, intense contrast enhancement during arterial phase was observed at the whole tumors or the periphery of the tumors by CEUS and CECT. Lower HIFU energy was used in group II than in group I (P < 0.001). Histopathologic assessment revealed local residual viable tumor tissues due to incomplete ablation in 47.4% (9/19) of tumors in group I and 10% (2/20) of tumors in group II (P < 0.05). The concordance rate of CEUS (90.9%) with histopathology on residual tumor detection was higher than that of CECT (27.3%, P < 0.05).
Conclusions
Introduction of the microbubble agent enhances HIFU therapeutic efficacy. CEUS proves to have high sensitivity in assessment of residual viable rabbit VX2 tumor after HIFU.




Similar content being viewed by others
References
Hwang JH, Crum LA (2009) Current status of clinical high-intensity focused ultrasound. Conf Proc IEEE Eng Med Biol Soc 2009:130–133
Li Q, Du J, Yu M et al (2009) Transmission electron microscopy of VX2 liver tumors after high-intensity focused ultrasound ablation enhanced with SonoVue. Adv Ther 26(1):117–125
Li JJ, Gu MF, Luo GY et al (2009) Complications of high intensity focused ultrasound for patients with hepatocellular carcinoma. Technol Cancer Res Treat 8(3):217–224
Thuroff S, Chaussy C (2000) High-intensity focused ultrasound: complications and adverse events. Mol Urol 4(3):183–187
Wu F, Wang ZB, Chen WZ et al (2004) Extracorporeal high intensity focused ultrasound ablation in the treatment of patients with large hepatocellular carcinoma. Ann Surg Oncol 11(12):1061–1069
Luo W, Zhou X, Yu M et al (2009) Ablation of high-intensity focused ultrasound assisted with SonoVue on Rabbit VX2 liver tumors: sequential findings with histopathology, immunohistochemistry, and enzyme histochemistry. Ann Surg Oncol 16(8):2359–2368
Yu T, Xiong S, Mason TJ et al (2006) The use of a micro-bubble agent to enhance rabbit liver destruction using high intensity focused ultrasound. Ultrason Sonochem 13(2):143–149
Luo W, Zhou X, Ren X et al (2007) Enhancing effects of SonoVue, a microbubble sonographic contrast agent, on high-intensity focused ultrasound ablation in rabbit livers in vivo. J Ultrasound Med 26(4):469–476
Jiang Y, Tian X, Luo W et al (2007) Transmission electron microscopy of rabbit liver after high-intensity focused ultrasound ablation combined with ultrasound contrast agents. Adv Ther 24(4):700–705
Wu F, Chen WZ, Bai J et al (2002) Tumor vessel destruction resulting from high-intensity focused ultrasound in patients with solid malignancies. Ultrasound Med Biol 28(4):535–542
Goldberg SN, Gazelle GS, Compton CC (2000) Treatment of intrahepatic malignancy with radiofrequency ablation: radiologic-pathologic correlation. Cancer 88(11):2452–2463
Goldberg SN, Gazelle GS, Mueller PR (2000) Thermal ablation therapy for focal malignancy: a unified approach to underlying principles, techniques, and diagnostic imaging guidance. AJR Am J Roentgenol 174(2):323–331
Illing RO, Kennedy JE, Wu F et al (2005) The safety and feasibility of extracorporeal high-intensity focused ultrasound (HIFU) for the treatment of liver and kidney tumours in a western population. Br J Cancer 93(8):890–895
Schwarz KQ, Chen X, Steinmetz S (1997) Harmonic imaging with Levovist. J Am Soc Echocardiogr 10(1):1–10
Xu HX, Lu MD, Xie XH et al (2009) Treatment response evaluation with three-dimensional contrast-enhanced ultrasound for liver cancer after local therapies. Eur J Radiol doi:10.1016/j.ejrad.2009.05.006 [Epub ahead of print]
Hwang JH, Wang YN, Warren C et al (2009) Preclinical in vivo evaluation of an extracorporeal HIFU device for ablation of pancreatic tumors. Ultrasound Med Biol 35(6):967–975
Yu T, Wang G, Hu K et al (2004) A microbubble agent improves the therapeutic efficiency of high intensity focused ultrasound: a rabbit kidney study. Urol Res 32(1):14–19
Hansler J, Neureiter D, Wasserburger M et al (2004) Percutaneous US-guided radiofrequency ablation with perfused needle applicators: improved survival with the VX2 tumor model in rabbits. Radiology 230(1):169–174
Bonte FJ, Curry GC, Parkey RW (1969) Experimental studies of the splanchnic circulation of the rabbit after ligation of the superior mesenteric artery. I. Angiographic and physiologic studies. Am J Roentgenol Radium Ther Nucl Med 106(4):691–699
Wu H, Exner AA, Shi H et al (2009) Dynamic evolutionary changes in blood flow measured by CECT in a hepatic VX2 tumor implant over an extended 28-day growth period: time-density curve analysis. Acad Radiol 16(12):1483–1492
Kuszyk BS, Boitnott JK, Choti MA et al (2000) Local tumor recurrence following hepatic cryoablation: radiologic-histopathologic correlation in a rabbit model. Radiology 217(2):477–486
Chen L, ter Haar G, Hill CR et al (1993) Effect of blood perfusion on the ablation of liver parenchyma with high-intensity focused ultrasound. Phys Med Biol 38(11):1661–1673
Hariharan P, Myers MR, Banerjee RK (2007) HIFU procedures at moderate intensities—effect of large blood vessels. Phys Med Biol 52(12):3493–3513
Fry FJ (1993) Intense focused ultrasound in medicine. Some practical guiding physical principles from sound source to focal site in tissue. Eur Urol 23(Suppl 1):2–7
Giorgio A, Ferraioli G, Tarantino L et al (2004) Contrast-enhanced sonographic appearance of hepatocellular carcinoma in patients with cirrhosis: comparison with contrast-enhanced helical CT appearance. AJR Am J Roentgenol 183(5):1319–1326
Farny CH, Glynn Holt R, Roy RA (2010) The correlation between bubble-enhanced HIFU heating and cavitation power. IEEE Trans Biomed Eng 57(1):175–184
Sasaki K, Medan MS, Azuma T, Umemura S et al (2006) Effect of echo-guided high-intensity focused ultrasound ablation on localized experimental tumors. J Vet Med Sci 68(10):1069–1074
Jaspers K, Nijenhuis RJ, Backes WH (2007) Differentiation of spinal cord arteries and veins by time-resolved MR angiography. J Magn Reson Imaging 26(1):31–40
Kato T, Nemoto R, Mori H et al (1984) Magnetic microcapsules for targeted delivery of anticancer drugs. Appl Biochem Biotechnol 10:199–211
Maruyama H, Matsutani S, Saisho H et al (2005) Sonographic shift of hypervascular liver tumor on blood pool harmonic images with definity: time-related changes of contrast-enhanced appearance in rabbit VX2 tumor under extra-low acoustic power. Eur J Radiol 56(1):60–65
Zhao JG, Feng GS, Kong XQ et al (2004) Changes of tumor microcirculation after transcatheter arterial chemoembolization: first pass perfusion MR imaging and Chinese ink casting in a rabbit model. World J Gastroenterol 10(10):1415–1420
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
He, W., Wang, W., Zhou, P. et al. Enhanced Ablation of High Intensity Focused Ultrasound with Microbubbles: An Experimental Study on Rabbit Hepatic VX2 Tumors. Cardiovasc Intervent Radiol 34, 1050–1057 (2011). https://doi.org/10.1007/s00270-010-0052-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-010-0052-3