Abstract
Purpose
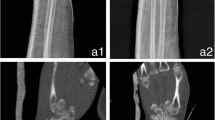
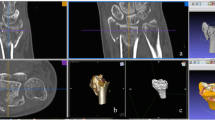
3D printing is a rapid prototyping technology that uses a 3D digital model to physically build an object. The aim of this study was to evaluate the peri-operative effect of 3D printing in treating complex elbow fractures and its role in physician–patient communication and determine which material is best for surgical model printing.
Method
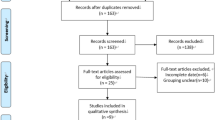
Forty patients with elbow fractures were randomly divided into a 3D printing-assisted surgery group (n = 20) and a conventional surgery group (n = 20). Surgery duration, intra-operative blood loss, anatomic reduction rate, incidence of complications and elbow function score were compared between the two groups. The printing parameters, the advantages and the disadvantages of PLA and ABS were also compared. The independent-samples t-test was used to compare the data between groups. A questionnaire was designed for orthopaedic surgeons to evaluate the verisimilitude, the appearance of being true or real, and effectiveness of the 3D printing fracture model. Another questionnaire was designed to evaluate physician–patient communication effectiveness.
Results
The 3D group showed shorter surgical duration, lower blood loss and higher elbow function score, compared with the conventional group. PLA is an environmentally friendly material, whereas ABS produce an odour in the printing process. Curling edges occurred easily in the printing process with ABS and were observed in four of ten ABS models but in only one PLA model. The overall scores given by the surgeons about the verisimilitude and effectiveness of the 3D model were relatively high. Patient satisfaction scores for the 3D model were higher than those for the 2D imaging data during physician–patient discussions.
Conclusion
3D-printed models can accurately depict the anatomic characteristics of fracture sites, help surgeons determine a surgical plan and represent an effective tool for physician–patient communication. PLA is more suitable for desktop fused deposition printing in surgical modeling applications.



Similar content being viewed by others
References
Qiao F, Li D, Jin Z, Hao D, Liao Y, Gong S (2016) A novel combination of computer-assisted reduction technique and three dimensional printed patient-specific external fixator for treatment of tibial fractures. Int Orthop 40(4):835–841
Mulford JS, Babazadeh S, Mackay N (2016) Three-dimensional printing in orthopaedic surgery: review of current and future applications. ANZ J Surg 86(9):648–653
Qiao F, Li D, Jin Z et al (2015) Application of 3D printed customized external fixator in fracture reduction. Injury 46(6):1150–1155
Li Z, Li Z, Xu R et al (2015) Three-dimensional printing models improve understanding of spinal fracture-a randomized controlled study in China. Sci Rep 5:11570
Li C, Yang M, Xie Y et al (2015) Application of the polystyrene model made by 3-D printing rapid prototyping technology for operation planning in revision lumbar discectomy. J Orthop Sci 20:475–480
Schout BM, Bemelmans BL, Martens EJ, Scherpbier AJ, Hendrikx AJ (2009) How useful and realistic is the uro trainer for training transurethral prostate and bladder tumor resection procedures? J Uro 181:1297–1303
Yang L, Shang XW, Fan JN (2016) Application of 3D printing in the surgical planning of trimalleolar fracture and doctor-patient communication. Biomed Res Int 2016:2482086, doi: https://doi.org/10.1155/2016/2482086
Zhuang Y, Cao S, Lin Y, Li R, Wang G, Wang Y (2016) Minimally invasive plate osteosynthesis of acetabular anterior column fractures using the two-incision minimally invasive approach and a preshaped three dimension plate. Int Orthop 40(10):2157–2162
Dubois-Ferrière V, Assal M (2014) Benefit of computer assisted surgery in foot and ankle surgery. Rev Med Suisse 10:562–564
Davidovitch RI, Weil Y, Karia R et al (2013) Intraoperative syndesmotic reduction: three-dimensional versus standard fluoroscopic imaging. J Bone Joint Surg Am 95:1838–1843
Durakbasa MO, Gumussuyu G, Gungor M, Ermis MN (2013) Distal humeral coronal plane fractures: management, complications and outcome. J Shoulder Elb Surg 22:560–566
Won SH, Lee YK, Ha YC, Suh YS, Koo KH (2013) Improving pre-operative planning for complex total hip replacement with a rapid prototype model enabling surgical simulation. Bone Joint J 95-B:1458–1463
Zein NN, Hanouneh IA, Bishop PD et al (2013) Three-dimensional print of a liver for preoperative planning in living donor liver transplantation. Liver Transpl 19:1304–1310
Acknowledgements
This study was funded by the Department of Science and Technology of Guiyang City (20151001) and National Natural Science Foundation (81360232) China.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Yang, L., Grottkau, B., He, Z. et al. Three dimensional printing technology and materials for treatment of elbow fractures. International Orthopaedics (SICOT) 41, 2381–2387 (2017). https://doi.org/10.1007/s00264-017-3627-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-017-3627-7