Abstract
Background
TNF inhibiting drugs (TNFi) provide symptomatic relief for patients with ankylosing spondylitis (AS), but uncertainty remains about long-term benefits. We compared hospital admissions, emergency department (ED) presentations, and direct health care costs before and after the availability of subsidized TNFi therapy for AS patients.
Methods
State-specific dispensing and cost data for TNFi therapy for AS in Western Australia (WA) were obtained from Pharmaceutical Benefits Scheme (PBS) and expressed as the number of defined daily doses (DDD)/1000 population/day. Linked admission and ED data for 1783 AS patients followed for 14,257 person-years between 1990 and 2015 were extracted. Pre- and post-2005 admission rates/100,000 population were compared by rate ratio (RR).
Results
TNFi uptake in WA reached a DDD/1000 population/day 0.45 at an annual cost of AU$17.7 million in 2020. Hospital admission rates remained unchanged (RR: 0.95, CI 0.71–1.27, p = 0.66) but increased slightly in female patients (RR 1.22; CI 0.91–1.64, p = 0.20). While there was no change in cardiovascular admissions (6.3 vs. 6.2%, p = 0.6) or ED visit rates since 2005, frequency for cancer (2.7 vs. 3.8%, p < 0.01), infection (1.1 vs. 1.7%, p < 0.01) and mental health (4.0 vs. 4.5%, p < 0.02) admissions increased. Associated direct health care costs (2020 values) averaged AU$14.7 million before and AU$ 24.7 million per year after 2005.
Conclusions
The introduction of subsidized TNFi therapy did not change all-cause hospital admission or ED visit rates for existing AS patients. Whether the significantly increased direct health care costs are offset by reductions in other health care costs remains to be determined.
Similar content being viewed by others
Hospital admissions rates for AS patients in Western Australia have not changed following the introduction of subsidized TNFi therapy in late 2004. |
The frequency of hospital admissions for mental health conditions, fractures and cancer increased slightly since 2005, but remained unchanged for cardiovascular events in AS patients. |
Emergency department visit rates for AS patients have not changed since 2005. |
Direct health care costs for AS in WA have increased on average 10 million AUD per years since 2005. |
Based on admission and TNFi inhibitor uptake data, the prevalence of AS in Western Australia is at least 0.29%. |
Introduction
Ankylosing spondylarthritis (AS) is a chronic immune-mediated inflammatory disease that predominantly affects the spinal and sacroiliac joints in 0.5–1% of the population [1]. Chronic inflammation contributes to peri-spinal ankylosis and spinal osteoporosis [2] leading to chronic back pain, impaired health-related quality of life (HRQoL), and increased risk of disability and premature death for AS patients [3,4,5,6]. Treatment options for AS patients have long been limited to physical therapy and nonsteroidal anti-inflammatory drugs (NSAIDs). However, long-term use of NSAID is associated with a range of well-known side effects that include peptic ulcer disease, heart disease, and renal insufficiency [7, 8]. The biologic drug class of tumor necrosis factor inhibitors (TNFi), which often leads to clinical improvement and a reduced need for NSAID use [9, 10], was first approved for the treatment of AS in Australia in August 2004 (https://www.pbs.gov.au/info/industry/listing/participants/public-release-docs/2016-06/bdmards--ankylosing-spondylitis-june-2016). AS patients are also at risk of a broad range of extra-articular complications (uveitis, aortic regurgitation, fractures) and associated comorbidities (cardiovascular events, inflammatory bowel disease, psoriasis, and drug toxicity), which often occur later in the disease course and are not sufficiently addressed by short-term clinical trials [11, 12]. Managing these complex features of AS thus poses a significant burden to the healthcare and public welfare systems through expenditures for medical care, disability support, and loss of productivity [13]. While there are emerging data that suggest long-term benefit of TNFi in improving mobility and lowering of cardiovascular risk [3, 13, 14], TNFi have also been associated with several serious side effects, including infections and malignancy [15]. Despite the recent introduction of biosimilars, TNFi remain expensive drugs, with an estimated annual cost of AU$10,000–15,000. This study investigated whether the uptake of TNFi by AS patients has had an impact on hospital admissions, ED presentations, and associated costs in Western Australia (WA).
Methods
Study Design
This is an observational study examining the longitudinal relation between hospital admissions, direct health care costs, and the dispensing of TNFi for patients with physician diagnosed AS in WA.
AS Population
The study cohort (Table 1) consisted of patients admitted to hospital with a diagnosis of AS between 1990 and 2015 in WA as identified in the Hospital Morbidity Data Collection (HMDC). The HMDC covers all separations from public and private hospitals in WA and includes primary and up to 20 co-diagnoses for each separation using the International Statistical Classification of Diseases and Related Health Problems (ICD) 9th or 10th revision [4]. Codes used to identify AS patients were ICD-9-CM: 720.0 and ICD-10-AM M45.0. For AS patients aged 18–80 years at their index hospital admission, we used longitudinally linked health data from the HDMC to identify the occurrence and primary reason for any prior or subsequent hospital admission in the state (Suppl Table 1) [4]. Given that regulatory approval for subsidized TNFi treatment for AS came in August 2004 (Supp Table 2) and allowing some run-in time, we used 1 Jan 2005 as the cut-off date to compare data between pre and post TNFi era. State-wide data from the Emergency Department Data Collection (EDDC) (available since 2002) for cohort patients were also extracted to similarly assess trends in ED visits. Historical population and admission data for WA over the full study period were obtained from the Australian Bureau of Statistics and provided denominators for admission rates.
TNFi Dispensing Data
In Australia, government subsidized TNFi therapy for AS is available only to patients seeing a rheumatologist for clinical findings compatible with AS, radiological evidence of ≥ grade 2 sacroiliitis, and a BASDAI score > 4 after 6 months of NSAID therapy and a 12-week exercise program (https://www.servicesaustralia.gov.au/organisations/health-professionals/forms/pb073). A paper-based application for access to TNFi then needs to be sent by the private or public rheumatologist (number of specialists is currently 25 in WA) for approval by Medicare Australia, although the selection of a particular TNFi agent remains at the discretion of the treating physician and the patient.
Annual WA-specific data for the dispensing (service) and costs (benefits) under the Pharmaceutical Benefits Scheme (PBS) for the five TNFi’s approved for AS treatment (infliximab, etanercept, adalimumab, golimumab, certolizumab) was obtained from the Australian Government Department of Human Services (http://medicarestatistics.humanservices.gov.au/statistics/pbs_item.jsp) using the disease-specific authority codes for TNFi treatment of AS in period 2005–2020 (Supp Table 1). Nr-SpA was only recognized as a PBS-listed indication for golimumab therapy by Medicare Australia in 2017 and thus not included in this dataset. Extracted data on TNFi dispensing were classified by their Anatomical Therapeutic Chemical (ATC) code and for each study year the corresponding WHO-approved defined daily dose (DDD) data were calculated. TNFi utilization was quantified as the number of DDDs/1000 population/day and cumulative annual costs in millions of Australian dollars (AU$).
Statistical Analyses
Descriptive statistics were compared by non-parametric methods (Kruskal–Wallis) for continuous variables and by crude odds ratio (OR) with 95% confidence intervals (CI) for categorical data. To reduce confounding, we excluded hospital admissions for TNFi infusions (n = 10,879 since 2005) and chronic dialysis (n = 3661) from the admission data which are presented as rate per 100,000 population and compared by rate ratios (RR) with 95% CI derived from conditional maximum likelihood estimates using Poisson distribution [17]. Direct hospital-based health care costs were based on 2008 costing data provided by the business unit at one of the metropolitan hospitals (personal communication) and adjusted for inflation using the consumer price index (CPI), health expenditure sub-class published by the Australian Bureau of Statistics and expressed in 2020 dollars (average AU$ 2,332/day), ED visits (AU$ 624) and outpatient infusions (AU$ 449). All analyses were performed using SPSS v23.0 (IBM, USA) and OpenEpi software with two-sided p values of p < 0.05 considered to be statistically significant.
Ethics
The study received ethics approval from the WA Department of Health Human Research Ethics Committee (WADOH HREC#: 2016.24).
Results
DDD for TNFi uptake rose steadily from 0.10 per 1000 persons/day in 2005 to 0.23 in 2010 to 0.33 in 2015 and continued to rise to 0.45 in 2020 (p < 0.01) (Fig. 1). There was an increasing diversity in specific TNFi drugs dispensed across WA over time (Fig. 1) and, despite the approval of multiple subcutaneous injectable TNFi, the DDD for intravenous infliximab remained high. The annual cost of subsidized TNFi therapy declined slightly after the introduction of biosimilars but later rose again after approval of golimumab for nr-SpA in 2018 (Suppl Fig. 1).
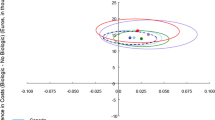
AS patients had a total of 31,709 hospital admissions over 25 years (17,492 before 2005 and 14,217 since 2005). The median annual number of admissions was higher for female (0.64, IQR 0.36–0.89) than male patients (median 0.4, IQR 0.2–0.76) (p < 0.001). Overall admission rates per 100,000 increased between 1990 and 2002, then declined to 2005 and remained relatively stable until a further decline in 2012 (Fig. 2). The mean annual hospitalization rate over the whole study period was higher, although not significantly, in female than male patients (RR: 1.22; 95%CI 0.91–1.64, p = 0.20). The mean overall annual admission rate post-2005 was not different from the pre-2005 period (RR: 0.95, 95% CI 0.71–1.27, p = 0.66) and gender-adjusted admission rate ratios were also similar (data not shown).
The frequency of cause specific admissions (Fig. 3) showed a fall in the frequency of external causes (e.g., injuries and poisoning), and increased admission for cancer (2.7 vs. 3.8%, p < 0.01), infections (1.1 vs. 1.7%, p < 0.01), mental health conditions (4.0 vs. 4.5%, p < 0.02). Notably there was no change in admissions for cardiovascular disease, but AS admission frequency was higher (5.1 vs. 6.9%). The rate of AS-related admissions adjusted for WA wide hospital admissions was 0.15/1000 before and 0.11/1000 after 2005 (rate ratio 0.77, CI 0.61–0.98), while the rate of AS-related admissions per 1000 admissions for AS patients was 68.3/1000 before and 68.7/1000 after 2005 (rate ratio 1.006, CI 0.91–1.02). The mean length of hospital stay decreased from 5.3 (± 9.3) days pre-2005 to 4.3 (± 9.9) days after 2005 (p < 0.01), while in-hospital mortality was similar in both periods (0.7 vs. 0.9%, p = 0.2). There was no significant change in mean annual overall (RR: 1.15, 95% CI 0.78–1.71, p = 0.56) or gender-specific ED visit rates since 2005 (Fig. 4).
Direct hospital-based health care costs were AU$14 million in both the pre- and post-2005 period, while the costs for TNFi drug and intravenous infusions added an average of AU$10 million to the costs (Suppl Table 3).
Finally, while not a primary aim of this study but because Australian data are lacking, we used these two datasets to estimate the population prevalence of AS. Based on the assumption that the 1925 AS patients that used a TNFi in 2020 represent 60% of all AS patients [16, 17] in WA, the estimated point prevalence for AS was 0.29% in 2020. This figure agreed with the 0.28% period prevalence rate of AS amongst all hospital admissions in WA over 20 years (Suppl Fig. 2).
Discussion
This study demonstrates a linear uptake of government subsidized TNFi drug therapy for AS patients in WA resulting in a DDD of 0.45/1000 persons/day by 2020. Over a 10-year observation period, during which TNFi therapy added between 10 and 15 million AU$ per year to direct health care costs in WA, we observed no significant change in hospital admission and ED visitation for AS patients with longer standing disease.
Given the lack of efficacy of traditional disease-modifying drugs in AS [11], the rapid uptake of TNFi following its approval for AS in Australia is not unexpected and in line with early expectations that, depending on national health care systems, 38–78% of AS patients attending rheumatology clinics in Europe would be initiated on TNFi therapy [18]. Current data suggest that at least 60% of AS patients will be initiating TNFi when following BASDAI-based guidelines, which are also in use in Australia [17]. This number can be expected to increase in the future as AS patients with BASDAI scores < 4 also have significant reductions in disease activity with TNFi [17].
All available TNFi drugs have consistently shown efficacy in reducing disease activity and patient-reported measures in clinical trials [9, 19, 20], and this is reflected in the increasing diversity of TNFi drugs used by rheumatologists in clinical practice in WA (Suppl Fig. 1). The relatively high percentage of AS patients continuing on intravenous therapy despite the availability of self-injectable TNFi is somewhat surprising, but in line with survey data from the United States (US) that suggests a continued patient/physician preference for TNFi infusion despite the added costs [19]. Fear of loss of efficacy when switching over, having difficulty with or being unable to self-inject due to poor dexterity, fear of needles, memory problems, learning disabilities, and having an 8-week window for travel were amongst arguments provided by patient experts in the NICE evaluation [21]. While drugs targeting other pathways have been approved over the last few years for AS patients not achieving a full or lasting response [22], longer-term outcome data are only available for TNFi.
AS has been reported to be associated with an increased risk of cardiovascular events and mortality [3, 12], but whether TNFi therapy mitigates this risk is yet unclear. A large observational study from Israel found that AS patients treated with TNFi did not demonstrate excess mortality compared to matched control [23]. Our data indicate that rates for hospital admission, in-hospital mortality, and ED visits did not change significantly following the introduction of TNFi therapy. The demographics and clinical characteristic of this cohort and the annual rate of hospital admission in this study (0.7/years) were comparable with recent data from Japan (0.7/years) [24] and Eastern Europe (0.9 per year) [20]. This makes it unlikely that unusual disease severity or activity in our cohort is the reason for the lack of benefit from TNFi therapy on hospital admission rates. It is also important to note that our dataset covered all hospital admissions for AS patients during the observation period regardless of location, insurance status or primary reason for admission. The analysis of primary admission diagnoses showed no impact of TNFi therapy on the frequency of heart disease requiring hospital care for AS patients, while the proportion of admissions for infections, cancer, and mental health rose slightly. This not unexpected during long-term follow-up of a cohort with a mean age of 46 years at study entry and suggests that general population changes and an aging cohort rather than TNFi usage was driving increased admissions for cancer (in Australia especially melanoma- see https://www.aihw.gov.au/reports/cancer/cancer-data-in-australia/) and mental health conditions. Overall, our data confirm that a decade of TNFi therapy did not have a major impact on admission rates for a broad category of complications [3, 25, 26]. This limited effect of TNFi on these crude outcomes may be due to the longer disease duration in this cohort of established AS patients and it would be of interest to see admission rate and type data for AS patients starting TNFi at an early age. Also, a more granular analysis into admission rates for specific complications (e.g., coronary syndromes, stroke, heart failure) was beyond the scope of this study but might be able to demonstrate more specific TNFi effects. While excluding infliximab infusions, we observed a proportional increase in admissions with a diagnostic code for AS from 5.4 to 6.9%. This is unlikely to reflect a higher rate of new AS diagnoses and although adjusted AS-specific admission rates did not change significantly, we cannot fully exclude that this was due worsening disease, however side effects of bDMARD therapy, increased public referral for TNFi consideration, or administrative coding changes for short stay admissions remain alternative explanations. Interestingly, there was a significant decrease in injury-related admissions since 2005 and while tempting to relate this to the better physical functional status in AS patients on TNFi therapy [20, 27], this remains speculative, especially as ED visit rates did not change over time.
AS is not an infrequent condition and the availability of two separate AS datasets allowed us to provide first population-based estimates of AS prevalence in (Western) Australia where diagnoses were confirmed by rheumatologists. The 0.29% AS prevalence rate was based on estimates from two separate sources (each imperfect as exemplified by the temporary rise since 2005 due to inclusion of new AS patients referred for TNF infusions) and thus needs to be considered a minimum estimate. Nonetheless, it falls within the range of reported AS prevalence (0.2–0.6%) depending on data source [1, 28].
The price-adjusted direct health care costs for admissions and ED visit for AS patients did not change significantly after 2005. As a result, the factual dollar costs for TNFi drugs (inclusive of possible price reductions) and infusions increased direct health care costs in WA on average by AU$ 10 million per year (Suppl Table 3). As WA comprises about 10% of the Australian population, this would indicate an AU$ 100 million annual increase for the national health budget while biologic therapy uptake for AS has not (yet) plateaued. These are minimum estimates as we favored a relatively simple dollar-based costing method, which is likely to have underestimated the much broader AR-DRG-based costs. Regardless of the costing method, a key unanswered question in this respect is if the potential improvements in quality of life, function, and productivity and the moderate reduction in other (e.g., GP visits) health care costs associated with TNFi use by AS patients [29,30,31,32] weigh up against this significant increase in direct health care costs. While we did not study this aspect, a few studies have tried to analyze this highly complex and potentially contentious issue. The latest NICE review in the UK indicated that anti-TNF therapies were just within the accepted limits of the recommended QALY cut-off of 20,000 GBP for cost effectiveness [21]. A recent European study of 1455 AS patients found that mean total costs increased from €6075 in the year prior to TNFi initiation to €27,871 in the year after TNFi initiation. This cost increase (> 300%) was offset by only a modest decrease in direct costs for consultations and other medication of 22% or €4761 [33]. A long-term observational study in the Czech Republic found that while indirect costs remained below €3000 in those reaching a state of low disease activity on TNFi therapy, chronic pain remained a main cause of work disability in AS, similar to findings in Portugal [13, 31]. Collectively, these data argue that the high price for symptomatic improvement in AS patients provided by TNFi (and other biologicals as well) is not clearly offset by longer-term savings for direct and indirect health care. Accordingly, reducing unduly high pricing for TNFi should become an important consideration for health authorities.
The limitations of this study need to be recognized and include the lack of clinical detail in the WARDER data base, which makes it difficult to evaluate the potential impact of specific measures for disease activity/severity. While AS patients in WA need to visit their rheumatologist at least twice a year to continue subsided TNFI treatment, we were not able to estimate potential savings on other outpatient, allied health, and GP care provision. The TNFi dispensing data were not individualized, making it impossible to correct for e.g., gender-based variations, changes in infliximab dosing or intervals or switching between TNFi and did not allow connection to AS patient data in the WARDER dataset. Finally, inclusion of a control group would have allowed more reliable long-term data for relatively rare events such as cancer. On the other hand, the long-term health data and TNFi prescription data for large numbers of patients with a physician-based AS diagnosis lends considerable strength to these observations.
Conclusions
AS prevalence in WA is at least 0.29%. The rapid uptake of TNFi in WA was not associated with a significant decline in all-cause hospital admissions for AS patients. TNFi therapy added 10–15 million AUD to the annual health care costs for AS patients in WA, but how this weighs up against improvements in quality of life, productivity, and non-hospital-based care remains unclear. Longitudinal and detailed study of AS-related resource use can provide crucial information for cost-effectiveness and improve our understanding of the natural disease history.
References
Bakland G, Nossent HC. Epidemiology of spondyloarthritis: a review. Curr Rheumatol Rep. 2013;15(9):351.
Hu LY, Lu T, Chen PM, Shen CC, Hung YM, Hsu CL. Should clinicians pay more attention to the potential underdiagnosis of osteoporosis in patients with ankylosing spondylitis? A national population-based study in Taiwan. PLoS ONE. 2019;14(2): e0211835.
Atzeni F, Nucera V, Galloway J, Zoltan S, Nurmohamed M. Cardiovascular risk in ankylosing spondylitis and the effect of anti-TNF drugs: a narrative review. Expert Opin Biol Ther. 2020;20(5):517–24.
Ognjenovic M, Raymond WD, Inderjeeth CA, Keen HI, Preen DB, Nossent JC. The risk and consequences of vertebral fracture in patients with ankylosing spondylitis: a population-based data linkage study. J Rheumatol. 2020;47(11):1629–36.
Bakland G, Gran JT, Nossent JC. Increased mortality in ankylosing spondylitis is related to disease activity. Ann Rheum Dis. 2011;70(11):1921–5.
Chiowchanwisawakit P, Thaweeratthakul P, Wattanamongkolsil L, Srinonprasert V, Koolvisoot A, Muangchan C, et al. Relationship between health-related quality of life and patient acceptable symptom state with disease activity and functional status in patients with ankylosing spondylitis in Thailand. J Clin Rheumatol. 2019;25(1):16–23.
Lee SH, Park YW, Choe JY, Shin K, Kwon SR, Cha JH, et al. Gastrointestinal risk factors and patient-reported outcomes of ankylosing spondylitis in Korea. Int J Rheum Dis. 2020;23(3):342–9.
Radner H, Ramiro S, Buchbinder R, Landewe RB, van der Heijde D, Aletaha D. Pain management for inflammatory arthritis (rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis and other spondylarthritis) and gastrointestinal or liver comorbidity. Cochrane Database Syst Rev. 2012;1: CD008951.
Maxwell LJ, Zochling J, Boonen A, Singh JA, Veras MM, Tanjong Ghogomu E, et al. TNF-alpha inhibitors for ankylosing spondylitis. Cochrane Database Syst Rev. 2015. https://doi.org/10.1002/14651858.CD005468.pub2.
Inman RD, Maksymowych WP, Group CS. A double-blind, placebo-controlled trial of low dose infliximab in ankylosing spondylitis. J Rheumatol. 2010;37(6):1203–10.
Nikiphorou E, Baraliakos X. Treat to Target in Axial Spondyloarthritis. Rheum Dis Clin N Am. 2019;45(4):519–35.
Haroon NN, Paterson JM, Li P, Inman RD, Haroon N. Patients with ankylosing spondylitis have increased cardiovascular and cerebrovascular mortality: a population-based study. Ann Intern Med. 2015;163(6):409–16.
Tuzil J, Mlcoch T, Jircikova J, Zavada J, Nekvindova L, Svoboda M, et al. Short-term response in new users of anti-TNF predicts long-term productivity and non-disability: analysis of Czech ATTRA ankylosing spondylitis biologic registry. Expert Opin Biol Ther. 2020;20(2):183–92.
Lee S, Park YJ, Lee JY. The effect of tumor necrosis factor-alpha inhibitors on uveitis in patients with ankylosing spondylitis. J Korean Med Sci. 2019;34(42): e278.
Kunnumakkara AB, Thakur KK, Rana V, Bora B, Banik K, Khatoon E, et al. Upside and downside of tumor necrosis factor blockers for treatment of immune/inflammatory diseases. Crit Rev Immunol. 2019;39(6):439–79.
Deodhar A, Strand V, Conaghan PG, Sullivan E, Blackburn S, Tian H, et al. Unmet needs in ankylosing spondylitis patients receiving tumour necrosis factor inhibitor therapy; results from a large multinational real-world study. BMC Rheumatol. 2020;4(1):19.
Marona J, Sepriano A, Rodrigues-Manica S, Pimentel-Santos F, Mourão AF, Gouveia N, et al. Eligibility criteria for biologic disease-modifying antirheumatic drugs in axial spondyloarthritis: going beyond BASDAI. RMD Open. 2020;6(1): e001145.
Pham T, Landewe R, van der Linden S, Dougados M, Sieper J, Braun J, et al. An international study on starting tumour necrosis factor-blocking agents in ankylosing spondylitis. Ann Rheum Dis. 2006;65(12):1620–5.
Mendelsohn AB, Nam YH, Marshall J, McDermott CL, Kochar B, Kappelman MD, et al. Utilization patterns and characteristics of users of biologic anti-inflammatory agents in a large, US commercially insured population. Pharmacol Res Perspect. 2021;9(1): e00708.
Opris-Belinski D, Erdes SF, Grazio S, Senolt L, Hojnik M, Nagy O, et al. Impact of adalimumab on clinical outcomes, healthcare resource utilization, and sick leave in patients with ankylosing spondylitis: an observational study from five Central and Eastern European countries. Drugs Context. 2018;7:212556.
Excellence NIFHAC. TNF-alpha inhibitors for ankylosing spondylitis and non-radiographic axial spondyloarthritis. Technology appraisal guidance [Internet]. 2016, p. 70. www.nice.org.uk/guidance/ta383. Accessed 2 Feb 2021.
D’Angelo S, Carriero A, Gilio M, Ursini F, Leccese P, Palazzi C. Safety of treatment options for spondyloarthritis: a narrative review. Expert Opin Drug Saf. 2018;17(5):475–86.
Ben-Shabat N, Shabat A, Watad A, Kridin K, Bragazzi NL, McGonagle D, et al. Mortality in ankylosing spondylitis according to treatment: a nationwide retrospective cohort study of 5900 patients from Israel. Arthritis Care Res (Hoboken). 2021. https://doi.org/10.1002/acr.24616.
Tomita T, Sato M, Esterberg E, Parikh RC, Hagimori K, Nakajo K. Treatment patterns and health care resource utilization among Japanese patients with ankylosing spondylitis: a hospital claims database analysis. Mod Rheumatol. 2021;31(2):431–41.
Holland-Fischer M, Thomsen RW, Tarp U, Norgaard M. Ankylosing spondylitis and mortality following hospitalised pneumonia: a population-based cohort study. RMD Open. 2020;6(1): e001140.
Xu Z, Xu P, Fan W, Yang G, Wang J, Cheng Q, et al. Risk of infection in patients with spondyloarthritis and ankylosing spondylitis receiving antitumor necrosis factor therapy: a meta-analysis of randomized controlled trials. Exp Ther Med. 2017;14(4):3491–500.
Komaki Y, Yamada A, Komaki F, Kudaravalli P, Micic D, Ido A, et al. Efficacy, safety and pharmacokinetics of biosimilars of anti-tumor necrosis factor-alpha agents in rheumatic diseases; a systematic review and meta-analysis. J Autoimmun. 2017;79:4–16.
Wang R, Ward MM. Epidemiology of axial spondyloarthritis: an update. Curr Opin Rheumatol. 2018;30(2):137–43.
Bakland G, Gran JT, Becker-Merok A, Nordvag BY, Nossent JC. Work disability in patients with ankylosing spondylitis in Norway. J Rheumatol. 2011;38(3):479–84.
Nikiphorou E, Ramiro S. Work disability in axial spondyloarthritis. Curr Rheumatol Rep. 2020;22(9):55.
Rodrigues J, Rodrigues AM, Dias SS, Sousa RD, Branco JC, Canhao H. Psoriatic arthritis and ankylosing spondylitis impact on health-related quality of life and working life: a comparative population-based study. Acta Reumatol Port. 2019;44(4):254–65.
Shim J, Jones GT, Pathan EMI, Macfarlane GJ. Impact of biological therapy on work outcomes in patients with axial spondyloarthritis: results from the British Society for Rheumatology Biologics Register (BSRBR-AS) and meta-analysis. Ann Rheum Dis. 2018;77(11):1578–84.
Redeker I, Callhoff J, Hoffmann F, Saam J, Haibel H, Sieper J, et al. Krankheitskosten bei axialer Spondyloarthritis für Patienten mit und ohne Tumor-Nekrose-Faktor-Inhibitor-Behandlung: Ergebnisse einer Routinedatenanalyse. Z Rheumatol. 2020;79(1):85–94.
Acknowledgements
The authors thank the Data Custodians of the Hospital Morbidity Data Collection (HMDC), Emergency Department Data Collection (EDDC), the Western Australian Cancer Registry (WACR), the State Registry of Births, Deaths and Marriages, the WA Electoral Commission, and the NCIS for use of the CODURF dataset, and the staff at Data Linkage Branch at the Western Australian Department of Health for their assistance in provision of data and DJ Nossent for PBS data extraction.
Funding
This work was supported by ‘Arthritis Australia’ [PG21/19] and ‘Arthritis Foundation of Western Australia’ [unrestricted grant]. No funding or sponsorship was received for the publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
JCN designed the study. JCN, EK were responsible for acquisition of the data, which were analyzed by JCN, EK, and IL. All authors contributed to interpretation of the data and were involved in drafting the manuscript or revising it critically and approved the final manuscript.
Disclosures
H Keen reports personal fees from AbbVie, Cornerstones, Roche, and Pfizer outside of the submitted work. C Inderjeeth reports research funding from AbbVie outside of the submitted work. Authors J Nossent, D preen, I Li, and E Kelty have nothing to disclose.
Compliance with Ethics Guidelines
Approval for use of de-identified data was obtained from the Human Research Ethics Committee at the WA Department of Health (WADOH HREC# 2016.24). As this study was considered low risk by the WA Health HREC and due to the de-identified nature of the linked health data set, the requirement for patient consent was waived. WA Health is proprietor of this administrative health data dataset. This study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments.
Data Availability
The data that support the findings of this study were used under license from WA Health Data Linkage Branch. Restrictions apply to the availability of these data, but upon reasonable request and following permission of WA Health and WA Data Linkage Branch data are available from the authors.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Nossent, J., Inderjeeth, C., Keen, H. et al. The Association Between TNF Inhibitor Therapy Availability and Hospital Admission Rates for Patients with Ankylosing Spondylitis. A Longitudinal Population-Based Study. Rheumatol Ther 9, 127–137 (2022). https://doi.org/10.1007/s40744-021-00393-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40744-021-00393-x