Abstract
Background and Objectives
Covid-19 vaccines approved by the EU, UK and USA have been found to be safe and effective. The cost effectiveness of these vaccines depends upon a number of factors. The aim of this paper is to explore the cost effectiveness of a COVID-19 vaccine and to analyse how the price of the vaccine and the cost of administrating it influence its cost effectiveness.
Methods
We considered an epidemiological model developed by an expert group within ‘Statens Serum Institut’, which is a unit under the auspices of the Danish Ministry of Health. The model allowed us to differentiate between two population groups, those aged ≥60 years and those aged <60 years. We used the model to consider four scenarios: (i) vaccination of 25% of the total population (corresponding to approximately 1.5 million persons) but targeting vaccines towards the population aged ≥60 years, (ii) vaccination of 25% of the total population, targeting vaccines only towards the population aged <60 years, (iii) vaccination of 40% of the total population where 15% are aged <60 years and 25% are aged ≥60 years (corresponding approximately to the full Danish population aged >60 years), and (iv) 40% of the total population is vaccinated but vaccines are targeted solely towards those aged <60 years. The time horizon of the analysis was six months, and the perspective was that of the Danish healthcare sector.
Results
The results show that inclusion of the elderly population aged ≥60 years was more cost effective than a vaccination strategy that targeted a population aged <60 years old only, when productivity losses were not included. Furthermore, the results show that an extension of the target group from the elderly population only, to also include the younger population comes with an increasing cost per life-year gained. The incremental cost-effectiveness ratio depends on the price of the vaccine, hereunder also the administration costs, and the discount rate used for the estimation of life-years or quality-adjusted life-years gained from a vaccine. Furthermore, inclusion of productivity losses in the analyses influenced the cost effectiveness of vaccination of the population aged <60 years of age.
Conclusion
The cost effectiveness of a COVID-19 vaccine is sensitive to whether or not productivity losses are included in the analyses. Without productivity losses, the elderly population should always be part of the target group for a COVID-19 vaccination programme. Taking productivity losses into account, at least in the case of low vaccine prices, vaccinating the younger population first can actually be cost effective.
Similar content being viewed by others
Vaccination of the population aged 60 years and older against COVID-19 is a cost-effective strategy compared with other strategies in the Danish vaccination programme. |
Whether the vaccination programme against COVID-19 for the population younger than 60 years old is cost-effective depends on the price of the vaccine and the costs of its administration as well as the testing costs. |
1 Introduction
At an unprecedented pace, several vaccines against coronavirus disease 2019 (COVID-19) have been developed, and several countries have adopted the vaccines in their efforts to control the disease [1, 2]. In addition to preventing the spread of the disease with all its consequences for the health and life of the infected, it is expected that many of the restrictions on human interactions can be lifted.
The vaccines that have been approved by the EU, UK and the USA have been found to be safe and 70%–95% effective against COVID-19 after two doses [3,4,5].
However, the cost effectiveness of the vaccines depends on several factors. An important aspect is the price of the vaccination and the costs of administrating it. That is, the total cost of vaccinating the population should be seen in relation to the costs of, for example, hospital treatment that can be avoided because of reduced cases of COVID-19.
Since healthcare systems are organised nationally, all countries in the world need to handle a shortage of vaccines in the short term. In the long term, national policy makers may also need to consider how the distribution of a vaccine should be organised and how it should be financed. In this paper we address these questions from the perspective of the Danish healthcare system.
In Denmark, universal healthcare coverage is provided to all permanent residents. Each resident is listed with a general practitioner (GP), and GPs are reimbursed by a combination of capitation (based on the number of residents on their list) and fee-for-service [6]. Hospital treatment and healthcare services from GPs are, with a few exceptions, provided free of charge to patients.
In terms of vaccination, all children in Denmark are covered by a national comprehensive childhood vaccination programme, which among others includes vaccination against diphtheria, tetanus, pertussis, polio, measles, mumps, rubella [7]. The human papillomavirus (HPV) vaccination against cervical cancer for girls and boys has been included in the programme since 2009 and 2019, respectively [8, 9].
In the national programme, all persons aged ≥65 years and persons with chronic diseases are recommended to be vaccinated against seasonal influenza and pneumonia.
The regions cover the cost of vaccinations that are included in the national immunisation programmes [6].
The cost-effectiveness of these vaccines has been studied in a Danish context previously, even though such considerations may not have been included directly in the decision to include these vaccinations in the Danish Immunisation programme [10,11,12,13].
The aim of this paper is to explore the cost-effectiveness of a COVID-19 vaccination. However, since significant aspects of the vaccine remain uncertain, such as availability and target groups, we aim to analyse how these aspects influence the cost-effectiveness of the vaccine.
2 Methods
2.1 Overview
We used a dynamic transmission model, which was developed by an expert group in ‘Statens Serum Institut’ (SSI), which is a unit under the auspices of the Danish Ministry of Health [14]. We added a vaccination component to analyse the effects of a COVID-19 vaccine on both health and economic outcomes for the Danish population over a time horizon of 6 months.
The health outcome was measured as life-years and quality-adjusted life-years (QALYs) gained. Costs were assessed from the perspective of the Danish healthcare sector, which included cost of vaccine and administration of the vaccine, testing for COVID-19 and GPs follow-up service on detection of a virus infection, and the costs of hospitalisation of patients because of an infection with COVID-19 virus. In addition, we included costs in terms of productivity loss.
The epidemiologic model allowed us to differentiate between two groups of individuals, those aged above and those aged below 60 years of age, respectively.
We limited the analyses to study the cost-effectiveness of a limited number of vaccine doses corresponding to vaccinating 25% and 40% of the total population, corresponding to approximately 1.5 million persons and 2.4 million persons, respectively.
2.2 Scenarios
We considered four scenarios, where we used the following notation: Vaccinated population = \((v;w)\) where \(v\) refers to individuals aged <60 years who were vaccinated, measured in percentage of the total population, and correspondingly, \(w\) denotes the percentage of the total population aged ≥60 years that was vaccinated .
In two scenarios we considered vaccination of a population size equivalent to the elderly population. Based on official Danish statistics, the number of persons aged ≥60 years was 1,513,240 in the 3rd quarter of 2020 [15]. This corresponded to approximately 25% of the total population. In the other two scenarios we consider availability of the vaccine corresponding to 50% of the population aged ≥16 years, approximately corresponding to vaccination of 40% of the population (2.4 million persons).
The four scenarios were compared to status quo: \(\mathrm{Vaccinated population }= (0 \%;0 \%)\). We defined four mutually exclusive scenarios:
-
\(\mathrm{Vaccinated population }= (0\mathrm{ \%};25\mathrm{ \%})\)
-
\(\mathrm{Vaccinated population }= (25\mathrm{ \%};0\mathrm{ \%})\)
-
\(\mathrm{Vaccinated population }= (15\mathrm{ \%};25\mathrm{ \%})\)
-
\(\mathrm{Vaccinated population} = (40 \%;0)\)
For modelling purposes, we assumed that the vaccines were available from the beginning of the time period applied in the model.
2.3 Transmission Model
The dynamic transition model used a SEIR (susceptible, exposed, infectious, recovered) structure (Fig. 1).
SSI’s extended structured SEIR model. SSI Statens Serum Institut, SEIR susceptible, exposed, infectious, recovered. S denotes the percentage of individuals susceptible to the virus, E1 to E3 the percentage of individuals having been exposed, so being infected but not yet infecting themselves, IR,1 to IR,3 the percentage of infected individuals recovering at home, IH,1 to IH,3 the percentage of infected individuals that will need hospital care, HR the percentage of hospitalised individuals recovering, HC the percentage of hospitalised individuals coming in need for intensive care, CR the percentage of individuals on intensive care that are going to recover, CD the percentage of individuals on intensive care that are going to die, D the percentage of individuals that died in the hospital. Each state distinguished between patients above 60 years old (i=2) and patients younger than 60 years (i=1)
For details about parameter ranges and the associated ordinary differential equation model see [14, 16]. We do repeated simulations (bootstraps, in our case 10.000) with parameters chosen uniformly from the parameter ranges given in Table 1. These simulations are weighted according to how well the number of predicted hospitalised individuals fit the actual number of hospitalised individuals in Denmark between March 11th and August 26th, 2020, split between the younger and older populations according to the corresponding ratio of all hospitalisations until May 19th. The 60% of simulations that fit worst were discarded. The differential equation model is listed in Fig. 2, and we list parameters and initial values used in the Supplementary material. We implemented the differential equation model in MATLAB and solved it using the stiff solver ode15s [17].
The model predicted the number of individuals dying on intensive care due to COVID-19, while the official definition of COVID19-related deaths counts the individuals dying within 30 days after a COVID-19 diagnosis. Therefore, we determined the ratio of the estimated weighted median of the cumulative number of individuals dying on intensive care and number of individuals dying within 30 days after a COVID-19 diagnosis from March 11th to August 26th. We did so for both age groups. We used these ratios to estimate for each of the two age groups the number of individuals dying 30 days after a COVID-19 diagnosis from the cumulative number of individuals dying on intensive care.
As for the number of individuals dying within 30 days after a COVID-19 diagnosis from March 11th to August 26th, the distribution on the two age groups was not available so we estimated it by using the ratio between the number of younger and older individuals dying within 30 days after a COVID-19 diagnosis from March 11th to May 19th.
2.4 Resource Use and Costs
All costs were measured for the year 2020 and reported in Danish kroner (DKK).Footnote 1
The cost of vaccination incorporates a number of uncertainties. First, apparently the price of the vaccine varies widely. Second, the cost of administering the vaccine will depend on the organisation of the vaccination programme. To deal with these uncertainties, we varied the unit cost from 300 to 500 DKK per vaccinated person, where we assumed that each person requires two vaccinations to be fully immunised against COVID-19. We based this on the following reasoning.
First, it is based on a now deleted entry on a social media platform by a European Minister of Health, who reported that the price of the vaccines was to be from 13 to 109 DKK per dose [18].
Second, since some of the vaccinations in Denmark will be carried out by general practitioners, the regional health authorities have made an agreement with the GPs’ organisation. In this agreement, a GP is remunerated with 146.25 DKK for a vaccination that is given on weekdays [19]. Furthermore, it is expected that GPs primarily vaccinate persons who live in nursing homes, whereas vaccination of the rest of the Danish population is expected to take place in vaccination centres [20].
The cost of hospitalisation was estimated on the basis of the diagnosis-related group (DRG) tariffs, which reflect the average operating cost for treatment of a patient in the group in a Danish publicly owned hospital [21]. Thus, since the charges are used for hospitalisations due to contagious infections, it includes preventive materials. Furthermore, it was based on documentation by The Danish Health Data Authority (DHDA) on how to assign hospitalisations due to COVID-19 in the DRG system [22]. Unfortunately, we were not able to access information on the distribution of hospitalised patients on their diagnoses and DRG classification.
We assumed that patients were hospitalised for more than one day, and that patients who were hospitalised in an intensive care unit suffered from a severe acute respiratory syndrome, whereas patients who were hospitalised outside an intensive care unit suffered from COVID-19 infection without specification of the localisation, and that patients hospitalised outside an intensive care unit did not suffer from complications. We also assumed that all hospitalised patients were aged ≥18 years. The latter was based on the observation that <3% of all hospitalised patients were aged ≤19 years [23].
In accordance with the DHDA’s classification, patients in need of respirator treatment were assumed to be classified in one of four intensive care groups, which included organ failure.
Since the distributions of patient diagnoses and DRG classifications were unknown, we used three different specifications for the hospitalisation cost parameters presented in Table 2. In particular, the unit cost for patients in respirator treatment varied.
In the presentation of the results, we used specification number 1 as the base case, and used the other specifications for sensitivity analyses.
Finally, we expected that vaccine administration would reduce the number of tests for infection with the virus which causes COVID-19. We assumed that the unit cost of a test was 200 DKK based on information from the regional health authorities interest organisation Danish Region brought forward in news media. The unit costs included test equipment, reagents, and salary to staff who carry out the test and the analyses of the test [24].
In addition to the cost of the test, we included the costs to general practitioners for follow-up services when a test proves a positive. According to an agreement between the Danish regional health authorities and the general practitioners’ organisation, the general practitioners were remunerated 146.25 DKK [25].
To carry out the analyses we needed an estimate of the number of people diagnosed with COVID-19 and we needed an estimate of the number of tests.
The number of people being diagnosed with COVID-19 required a stepwise calculation as the epidemiological model only calculated the number of people being infected. To transform the cumulative number of individuals infected with COVID-19 to the number of people being diagnosed, we needed to know the proportionality between the two. Thus, we calculated the ratio of the estimated weighted median of the cumulative number of infected individuals, when no vaccine was provided, to the actual number of individuals diagnosed with COVID-19 until August 26th, 2020, in Denmark. This ratio was denoted by \(\frac{1}{\mu }\) and allowed us to estimate the number of people being diagnosed.
To estimate the number of tests, we used the proportion of the total number of tests that were carried out as of 26th August 2020 relative to the cumulative number of persons diagnosed with COVID-19 as of this date, we call this \(\zeta \). Then, this proportionality factor was multiplied by the estimated number of people being diagnosed in our model.
Table 2 summarises the different costs applied and presents the relation to the model states.
2.5 Productivity Loss
To estimate the costs of lost production because of infection with COVID-19, we used results from a telephone survey by Statens Serum Institut about the duration of the illness. The survey was conducted 27th February–31st March 2020, and included 265 persons who had been identified from a national database with laboratory-confirmed COVID-19 incidences [26]. Furthermore, we used statistics on earnings per hour and the employment and population size by age groups from Statistics Denmark [27,28,29], and statistics on the number of usual hours of work from Eurostat [30] (see Supplementary material for calculations of productivity loss).
2.6 Outcomes
In the model we used two different outcome measures, namely gained life-years (LY) and quality-adjusted life-years (QALY). The LY allowed us to determine the efficiency of the different alternatives in comparison with other public health interventions and vaccine programmes in Denmark. The QALY allowed us to determine the efficiency of the different alternatives in comparison with other healthcare interventions in general.
With both outcome measures, we found the cumulative effects over a 6-month period. We determined the total additional effects of the intervention, which was the life-years or quality-adjusted life-years gained, with vaccination compared to the situation with no vaccination.
We estimated the number of lost life-years for individuals aged ≥60 years and those aged <60 years (see Table 3) by weighting the expected number of life-years for men and women in the age groups 20–59, 60–69, 70–79, 80–89 and 90–99 retrieved from Statistics Denmark [31, 32] with the relative occurrence of men and women in those age groups among the individuals infected with COVID-19 that according to SSI had died up to June 3rd, 2020 [33].
To adjust the expected life-years for quality of life, we used the approach suggested by Briggs et al. [34]. The approach suggests adjusting QALYs gained from interventions against COVID-19 for pre-existing diseases that may influence quality of life and mortality. For the base case analysis, we assumed that infected individuals did not suffer from any other morbidity that could affect their quality of life or mortality ratio. In sensitivity analyses we relaxed these assumptions. We also applied QALY as effectiveness measure to capture the full value of a vaccination programme, which also has an impact on the quality of life. The quality-of-life weights used to calculate QALYs were obtained from a Danish study that surveyed quality-of-life in the Danish population aged 20–79 years [35].
QALYs are presented undiscounted and discounted with a discount rate of 2% or 4% (Table 4), as the Ministry of Finance recommends a discount rate of 4% for projects with a time horizon up to 35 years and 2% for effects beyond 35 years [36].
2.7 Assumptions
Findings from controlled studies of vaccine efficacy demonstrate approximately 95% efficacy, which is considered to be compatible to 100% efficacy against severe disease [37]. In the model simulation we therefore assume that the vaccination provides 100% effectiveness against COVID-19. In a sensitivity analysis, we also estimated the cost-effectiveness if the vaccine had lower efficacy (80%).
The epidemiological model is calibrated to the observations in the Spring of 2020 and not the Autumn of 2020, it therefore implicitly assumes that the human behaviour related to social distance, facemasks in public transportation, hygiene, cleaning as of Spring 2020 is maintained.
3 Results
3.1 General Results
The following sections show the results from the simulation model. Figure 3 shows the fourteen-days sliding average of the effective reproduction number, \({R}_{t}\).
Table 4 shows the number of QALYs lost under the five alternatives and the number of QALYs gained from a vaccination programme to various target groups. From this analysis we see that vaccination programmes that included the elderly population aged ≥60 years increased the number of QALYs gained compared to programmes that only targeted those aged <60 years.
Table 5 shows the healthcare costs under the five alternatives and with the three different specifications of the cost parameters for hospital in the model. It shows that healthcare costs were lower with a vaccination programme than without vaccination.
The healthcare costs are considerably lower when vaccinating the younger population than vaccinating the older population (Scenario 1 vs 2). This may seem counter-intuitive due to older infected people being more likely to need hospital treatment, but it is caused by the composition of the healthcare costs. The cost of hospitalisation only accounts for a smaller share of the healthcare costs (between 5 and 41% of the total healthcare costs in specification 1; slightly more in specification 2 and slightly less in specification 3). The largest part of healthcare costs is testing and follow-up, which depend on the number of overall infected people. This is lower when vaccinating the younger population, as in this case the number of unvaccinated people is distributed more evenly between the age groups, and infections are much more likely within a group than across the two age groups.
As healthcare costs comprise hospital costs, costs of testing and follow up, it follows that these costs will reduce if more people are vaccinated (from 1.5 to 2.4 million).
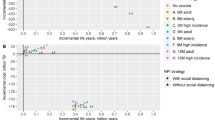
Figure 4 presents the cost-effectiveness plane applying specification 1 for the hospital costs with undiscounted gained life-years.
In all cases, scenarios 2 (25%; 0%) and 4 (40%; 0%) are dominated by alternatives that include the elderly population in the target group when not including productivity loss, whereas scenario 2 (25%; 0%) would be on the cost-effectiveness frontier (Fig. 4b), if productivity costs were included and the price of the vaccine was 300 DKK.
Figure 4 shows the cost-effectiveness plane for the four vaccination programmes and the status quo alternative without vaccination. In the figure, the costs of the vaccination were included with 300, 400 or 500 DKK per full vaccination. The upper panel is the cost-effectiveness plane without productivity loss, the lower panel with productivity loss. The colour of the points refers to the cost of the vaccination. For each vaccination cost specification, the frontier is represented by the linear connections between the alternatives with the lowest costs and the highest number of life-years gained. Points above the frontier are dominated by alternatives on the frontier.
Figure 5 illustrates the incremental cost-effectiveness ratios (ICER) for the vaccination programmes not dominated for the various total vaccination costs including administration in the range of 300 DKK to 500 DKK per full vaccination. The figure includes the gained QALYs undiscounted, the upper panel without productivity loss, the lower panel with productivity loss.
Especially for higher vaccination costs, the ICER is significantly lower for the scenario of vaccinating 25% of the population persons compared to the scenario of vaccinating 40% of the population.
3.2 Robustness Check and Sensitivity Analysis
Due to the uncertainty about the distribution of hospitalised patients on their diagnoses and DRG classification, we do a robustness check of our results using the costs as described in Table 6.
From Table 6 we conclude that the ICER for a gained life-year or QALY, given the intervention with a vaccination programme, is not sensitive to the costs of hospitalisation.
We have presented four scenarios assuming up to 40% of the population has been vaccinated. At the time of writing, the number and availability of vaccine doses are uncertain. For the sake of comparison, we have also examined a scenario where 70% of the total Danish population is vaccinated. This scenario would imply that 45% of the total population vaccinated are aged <60 years and 25% of the total vaccinated population is aged ≥60 years. The gain in life-years would be 6140 (undiscounted) and the gain in QALYs would be 5170 (undiscounted), which should be compared with the numbers in Table 4.
If, on the other hand, this 70% scenario is compared to doing nothing, the ICER per QALY compared to status quo would be in the range from approximately 141–298 measured in 1000 DKK without productivity loss and approximately 94–251 with productivity loss, with the vaccination costs ranging from 300 to 500 DKK.
Our analysis did not adjust for comorbidity, and we therefore conducted a sensitivity analysis to evaluate the robustness of our results. We compared results including a standard mortality rate (SMR) increasing to 1.5 and 2 and a parameter to adjust for the specific impact of pre‐existing comorbidity on quality of life (qCM) ranging 100%, to 90% and 80%.
From Table 7 we conclude that incorporating co-morbidity in the analysis increased the ICER caused by reduced QALYs.
Finally, we evaluated the consequences of the assumption that the vaccine has 100% effectiveness against COVID-19. A reduction in effectiveness from 100 to 80% implied a reduction in gained QALYs between 13 and 16%, an increase in total healthcare costs between 7 and 18%, and an increased productivity loss around 4–14% for scenarios 1 and 3. This followed the line that the ICER on average increases if the vaccine is less effective.
4 Discussion
In this study we aimed to examine the cost-effectiveness of a vaccine against COVID-19, where we added an economic component to an epidemiological model. The results show that inclusion of the elderly population ≥60 years of age is more cost-effective than a vaccination strategy targeted a population aged <60 years only independently of using life-years or QALYs gained when productivity losses are not included; whereas vaccination targeted the population <60 years of age may be cost-effective when productivity losses are included, and vaccine prices are low. Furthermore, the results show that an extension of the target group from the elderly population only to also include younger populations comes with an increasing cost per life-year gained. This could be an indication of diminishing marginal product of the vaccination combined with increasing costs, which follows from the observation that mortality from COVID-19 is low for individuals below 60 years of age. These findings were independent of the specification of the cost of hospitalisation for treating COVID-19 infections and the price of the vaccine. However, the ICER depends on the price of the vaccine and the administration costs.
Our model presents the cost-effectiveness ratio for the different scenarios, which allows for comparison of these ratios in-between scenarios and to other vaccination programmes. In an alternative scenario we examined the cost-effectiveness of a vaccination strategy where 70% of the adult population is vaccinated. The results suggest that the costs per life-year or QALY gained are within the same range as those in the four scenarios we analysed initially.
An essential strength of this study is that we build on an epidemiological model for the Danish population. We added a component to include the possibility of vaccination and cost parameters and an effectiveness measure in terms of life-years gained.
However, the results should also be seen in light of a number of limitations. First, detailed information about the costs of hospitalisation for treatment of COVID-19 infections is not available at the time of writing. Thus, the analysis is based on assumptions presenting different cost specifications.
In addition, we do not include costs outside the healthcare sector. It is well known that governments impose restrictions such as lockdowns, assembly bans and other measures to limit the spread of the virus that causes COVID-19. The costs of managing the epidemic are significant [38]. These costs affect the whole society and not only the individuals who are infected. Furthermore, there can also be production costs due to quarantine while individuals who suspect they are infected wait for a test.
Because costs outside the healthcare sector are not included, we regard the presented estimates of costs per gained life-year as an upper price of the life-years gained in a vaccination programme.
In a study of the economic value of a COVID-19 vaccine in the USA, Kohli et al. finds that a vaccination would be cost-saving in the high-risk group, and that ICERs are below US$50,000 per QALY gained in other risk groups assuming a single dose vaccine cost of US$35 (US$70 per course, i.e., two doses) [39]. This study differs from our study in several ways. First, they use a Markov cohort model, whereas we use a differential equation model. Second, the time horizon of their study is one year, whereas we use a time horizon of six months.
As mentioned in the introduction, several vaccines are included in the Danish immunisation programme. The cost-effectiveness of these vaccines has been examined in previous studies. The HPV vaccine has been shown to cost 85,000–139,000 DKK per life-year gained (2007 values, 3% discount rate) [11], whereas an expansion of that programme to include boys has been found to cost 33,000 DKK per QALY gained (2019 values) without production costs [12].
In analyses of screening programmes against cancer, the ICERs of these programmes have been found to be in the range of 76,000–157,000 DKK per life-year gained (2008 values) [40].
In our analysis we find an ICER in the range of approximately 45,000 DKK–274,000 DKK with undiscounted life-years and a cost of full vaccination at 300 DKK. For higher costs of vaccination or discounted life-years the cost-effectiveness ratio will increase.
Compared to these estimates, our findings of the costs per life-year gained for a vaccination against COVID-19 for the elderly population are below or within the ranges of that for other preventive programmes in Denmark. For the population below 60 years of age, the cost-effectiveness of a vaccine depends on the price of the vaccine, including the administration costs, and whether productivity losses are included. Demonstration of the cost-effectiveness of the vaccine to this age group would require additional analyses including costs outside the healthcare sector. However, since our results suggest a diminishing marginal product of vaccination, further research should look into the optimal distribution of the vaccine between the two population groups.
5 Conclusion
The cost-effectiveness of a COVID-19 vaccine is sensitive to whether or not productivity losses are included in the analyses. Without productivity losses, the elderly population should always be part of the target group for a COVID-19 vaccination programme. At the same time this secures the highest number of life-years gained given a limited availability of doses of the vaccine. Taking productivity losses into account, at least in case of low vaccine prices vaccinating the younger population first, can actually be cost-effective.
Compared to other interventions, e.g., cancer screening programmes, COVID-19 vaccination of the elderly population is cost-effective for cost of vaccination. For the population group aged <60 years the cost-effectiveness compared to other programmes depends on the costs of the vaccination and the discount rate, and other costs related to COVID-19 not included in our model.
Notes
1 USD corresponds approximately to 6 DKK, 1 EUR corresponds approximately 7.4 DKK (January 2021).
References
The New York Times. Corona Virus Tracker. https://www.nytimes.com/interactive/2020/science/coronavirus-vaccine-tracker.html. Accessed 3 Feb 2021.
European Medicines Agency. Treatments and vaccines for COVID-19: authorised medicines. https://www.ema.europa.eu/en/human-regulatory/overview/public-health-threats/coronavirus-disease-covid-19/treatments-vaccines/treatments-vaccines-covid-19-authorised-medicines. Accessed 3 Feb 2021.
Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, C4591001 Clinical Trial Group. Safety and efficacy of the BNT162b2 mRNA covid-19 vaccine. N Engl J Med. 2020;383(27):2603–15. https://doi.org/10.1056/NEJMoa2034577.
Baden LR, El Sahly HM, Essink B, Kotloff K, Frey S, Novak R, COVE Study Group. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med. 2020. https://doi.org/10.1056/NEJMoa2035389.
Voysey M, Madhi SA, Weckx LY, Folegatti PM, Aley PK, Oxford COVID Vaccine Trial Group. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet (British Edition). 2021;397(10269):99–111. https://doi.org/10.1016/S0140-6736(20)32661-1.
Ministry of Health, Healthcare in Denmark—An Overview. https://www.healthcaredenmark.dk/media/ykedbhsl/healthcare-dk.pdf. Accessed 6 Oct 2021.
Danish Health Authority, Statens Serum Institut, Danish Medicines Agency, The Danish childhood vaccination program. Summary in English. 2018. https://www.sst.dk/-/media/Udgivelser/2018/Børnevaccinationsprogrammet-årsrapport-2017/The-Danish-childhood-vaccination-program,-d-,-Summary-in-English.ashx. Accessed 6 Oct 2021.
Sander BB, Rebolj M, Valentiner-Branth P, Lynge E. Introduction of human papillomavirus vaccination in Nordic countries. Vaccine. 2012;30(8):1425–33. https://doi.org/10.1016/j.vaccine.2011.11.097.
Statens Serum Institut. HPV vaccination for boys, EPI-News, No 24/25-2019. https://en.ssi.dk/news/epi-news/2019/no-24-25---2019. Accessed 6 Oct 2021.
Bjerregaard P, Pedersen KM, Kamper-Jørgensen F, Koch C, Pedersen FK, Wagner AL, Zoffmann H. Vaccination mod mæslinger, fåresyge og røde hunde I: Lægelige og epidemiologiske aspekter. Ugeskrift Læger. 1985;147(38):3013–7.
Sundhedsstyrelsen. Reduktion af risikoen for livmoderhalskræft ved vaccination mod humant papillomvirus (HPV)—en medicinsk teknologivurdering Reduktion af risikoen for livmoderhalskræft ved vaccination mod humant papillomvirus (HPV)—en medicinsk teknologivurdering. København: Sundhedsstyrelsen, Enhed for Medicinsk Teknologivurdering, 2007 Serienavn 2007; 9(1). https://www.sst.dk/-/media/Udgivelser/2007/Publ2007/MTV/HPV/HPV_vaccination_smfatn,-d-,pdf.ashx. Accessed 6 Oct 2021.
Sundhedsstyrelsen. Medicinsk teknologivurdering (MTV) af HPV-vaccination af drenge. 2019. https://www.sst.dk/-/media/Udgivelser/2019/HPV-til-drenge/MTV_HPV_vaccination_drenge_270619.ashx?la=da&hash=9124D3490CC61CD9BE125B1C9F25599A5761F9EC. Accessed 6 Oct 2021..
Statens Institut for Medicinsk Teknologivurdering: Influenzavaccination af ældre Medicinsk Teknologivurdering 2000;2(1). https://www.sst.dk/Udgivelser/2000/~/media/CEB9430D2B1145589CD34E9E9D39EE5A.ashx. Accessed 6 Oct 2021.
SSI expert group, COVID-19 DK. https://github.com/laecdtu/C19DK. 2020. Accessed 6 Oct 2021.
Statistics Denmark. StatBank Denmark, FOLK1A: population at the first day of the quarter by region, sex, age and marital status. https://www.statistikbanken.dk/statbank5a/default.asp?w=1440. Accessed 6 Oct 2021.
Teknisk gennemgang af modellerne, Technical report, Statens Serum Institut, June 2020. Version 1.0.
Shampine LF, Reichelt MW. The MATLAB ODE suite. SIAM J Sci Comput. 1997;18:1–22 (dedicated to C. William Gear on the occasion of his 60th birthday).
TV2, Minister kom til at afsløre hemmelig prisliste—så meget koster de forskellige vacciner, 19th December 2020. https://nyheder.tv2.dk/udland/2020-12-19-minister-kom-til-at-afsloere-hemmelig-prisliste-saa-meget-koster-de-forskellige. Accessed 8 Jan 2021.
Praktiserende Lægers Organisation, COVID-19-vaccine. https://www.laeger.dk/PLO/covid-19-vaccine#honorar. Accessed 8 Jan 2021.
Sundhedsstyrelsen, Selve vaccinationsprogrammet. https://www.sst.dk/da/corona/Vaccination-mod-COVID-19/Selve-vaccinationsprogrammet. Accessed 8 Jan 2021.
Sundhedsdatastyrelsen, DRG-takster 2020. https://sundhedsdatastyrelsen.dk/da/afregning-og-finansiering/takster-drg/takster-2020. Accessed 6 Oct 2021.
Sundhedsdatastyrelsen. Håndtering af COVID-19 i DRG. https://sundhedsdatastyrelsen.dk/-/media/sds/filer/finansiering-og-afregning/gruppering/noegler/2020/haandtering-af-covid_19-i-drg.pdf?la=da. Accessed 6 Oct 2021.
Statens Serum Institut, Indlagte patienter: køn og alder—akkumuleret. https://www.sst.dk/da/corona/status-for-epidemien/tal-og-overvaagning#2. Accessed 18 Dec 2020.
BT, Så meget koster det regionerne at teste én person for corona, 18th September 2020. Accessed 8 Jan 2021.
https://www.sundhed.dk/sundhedsfaglig/information-til-praksis/syddanmark/almen-praksis/nyheder-og-meddelelser/nyhedsbreve/nyt-fra-regionen/nyt-2020-juni-test-henvisning-naere-kontakter/. Accessed 20 Jan 2021.
Statens Serum Institut. COVID-19 i Danmark. Epidemiologisk trend og fokus: Symptomer. 25. maj 2020. https://files.ssi.dk/COVID19-epi-trendogfokus-25052020-us12 . Accessed 30 Aug 2021.
Statistics Denmark. StatBank Denmark. LONS60: LONS60: Earnings per hour worked by industry (DB07), age, sex and components.
Statistics Denmark. StatBank Denmark. FOLK1B: population at the first day of the quarter by citizenship, sex, region, age and time. https://www.statistikbanken.dk/statbank5a/default.asp?w=1440. Accessed 6 Oct 2021.
Statistics Denmark. StatBank Denmark. RAS300: employed (end November) by industry (DB07), socioeconomic status, age and sex. https://www.statistikbanken.dk/statbank5a/default.asp?w=1440. Accessed 6 Oct 2021.
Eurostat. Average number of usual weekly hours of work in main job, by sex, professional status, full-time/part-time and economic activity (from 2008 onwards, NACE Rev. 2)—hours. http://appsso.eurostat.ec.europa.eu/nui/show.do?dataset=lfsa_ewhun2&lang=en. Accessed 6 Oct 2021.
Statistics Denmark. StatBank, HISB8: life table (2 years tables) by sex, age, and life table. https://statistikbanken.dk/statbank5a/SelectVarVal/Define.asp?Maintable=HISB8&PLanguage=1. Accessed 6 Oct 2021.
Statistics Denmark. StatBank, FOLK2: population 1. January by sex, age, ancestry, country of origin and citizenship. https://www.statistikbanken.dk/FOLK2. Accessed 6 Oct 2021.
Danmarks Statistik. Eksperimentel statistik—COVID-19. https://www.dst.dk/da/Statistik/eksperimentel-statistik-covid-19. Accessed 18 Dec 2020.
Briggs AH, Goldstein DA, Kirwin E, Meacock R, Pandya A, Cannes DJ, Wisløff T. Estimating (quality-adjusted) life-year losses associated with deaths: with application to COVID-19. Health Econ. 2021;30(3):699–707.
Sørensen J, Davidsen M, Gudex C, Pedersen Km, Brønnum-Hansen H. Danish EQ-5D population norms. Scand J Public Health 2009;37:467–474.
Folketinget, Det international Sekretariat. Notat om samfundsøkonomisk diskonteringsrente. https://www.ft.dk/samling/20181/almdel/FIU/bilag/21/1967824.pdf. Accessed 6 Oct 2021.
Mahase E. Covid-19: moderna applies for US and EU approval as vaccine trial reports 94.1% efficacy. BMJ. 2020;371. https://doi.org/10.1136/bmj.m4709.
The Economic Council. Danish Economy, autumn 2020. https://dors.dk/english/list-of-reports. Accessed 6 Oct 2021.
Kohli M, Maschio M, Becker D, Weinstein MC. The potential public health and economic value of a hypothetical COVID-19 vaccine in the United States: Use of cost-effectiveness modeling to inform vaccination prioritization. Vaccine. 2021;39(7):1157–1164.
Sundhedsstyrelsen, Monitorering & Medicinsk Teknologivurdering Screening for tarmkræft: Deltagelsesprocentens betydning—en medicinsk teknologivurdering København: Sundhedsstyrelsen, Monitorering & Medicinsk Teknologivurdering, 2008 Medicinsk Teknologivurdering 2008;10(1). https://www.sst.dk/-/media/Udgivelser/2008/Publ2008/MTV/screening_tarmkraeft/MTV_tarmkraeft_net_final_version2,-d-,pdf.ashx. Accessed 6 Oct 2021.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
All authors are employed at the University of Southern Denmark. No other funding was received.
Conflicts of interest
There are no conflicts of interests.
Availability of data and material
All necessary information concerning data estimations are included in the manuscript. Further details are available upon request.
Code availability
The code is available upon request.
Ethics approval
The project did not collect or use data on individual level. Only statistical information, which was publicly available, was used in the study. Therefore, the project did not require ethical approval. According to Danish law, health research projects must be notified and approved by a scientific committee where it is understood that a health research project “(…) must involve a research participant (or material from a research participant) who is exposed to an intervention, and in most cases, this will mean treatment, examination or preventive intervention” (National Committee on Health Research Ethics, What to notify, https://en.nvk.dk/how-to-notify/what-to-notify). Thus, the project does not qualify as a health research project under the Danish Committee Act (https://www.retsinformation.dk/eli/lta/2020/1338).
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Author contributions
All authors contributed equally to all parts of the project.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Debrabant, K., Grønbæk, L. & Kronborg, C. The Cost-Effectiveness of a COVID-19 Vaccine in a Danish Context. Clin Drug Investig 41, 975–988 (2021). https://doi.org/10.1007/s40261-021-01085-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-021-01085-8