Abstract
Introduction
A co-payment fee of EUR10 was introduced in Cyprus, in order to cope with overcrowding of emergency room services. The scope of this paper is the assessment of the short-term impact of this measure.
Methods
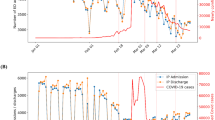
We used an interrupted time-series autoregressive integrated moving average model, and we analyzed official data from Cyprus’ largest emergency room facility for three years.
Results
Co-payment is associated with a 16 % statistically significant reduction of emergency room visits. No impact was observed in categories of teenagers, children, infants, and people over 70 years old.
Conclusions
Co-payment was proven to be effective in Cyprus’ emergency room setting and is expected to lessen congestion in the emergency room. The price insensitivity of people aged over 70 years, teenagers, children and infants, merits additional research for the identification of the underlying reasons.


Similar content being viewed by others
References
Selby JV, Fireman BH, Swain BE. Effect of a copayment on use of the emergency department in a health maintenance organization. N Engl J Med. 1996;334(10):635–41.
O’Grady KF, Manning WG, Newhouse JP. The impact of cost sharing on emergency department use. N Engl J Med. 1985;313(8):484–90.
Weiss Am L, D’Angelo L, Rucker A. Adolescent use of the emergency department instead of the primary care provider: who, why, and how urgent? J Adolesc Health. 2014;54(4):416–20.
National Hospital Ambulatory Medical Care Survey: 2010 Emergency Department Summary Tables. Atlanta: Centers for Disease Control and Prevention; 2013. www.cdc.gov/nchs/data/ahcd/nhamcs_emergency/2010_ed_web_tables.pdf. Accessed Dec 2013.
Weinick R, Billings J, Thorpe J. Ambulatory care sensitive emergency department visits: a national perspective. In: Abstract Academy Health Meeting, vol 20 (abstr no. 8), 2003. p. 525–526.
Ragin DF, Hwang U, Cydulka RK, Holson D, Haley LL Jr, Richards CF, Becker BM. Richardson LD Reasons for using the emergency department: results of the EMPATH Study. Acad Emerg Med. 2005;12(12):1158–66 (Epub 2005 Nov 10).
Mehrotra A, Liu H, Adams J, Wang M, Lave J, Thygeson M, et al. Comparing costs and quality of care at retail clinics with that of other medical settings for 3 common illnesses. Ann Intern Med. 2009;151(5):321–8 (PubMed: 19721020).
Machlin S, Chowdhury S. Expenses and characteristics of physician visits in different ambulatory care settings, 2008. Statistical Brief #318. 2011. Agency for Healthcare Research and Quality: Rockville. http://www.meps.ahrq.gov/mepsweb/data_files/publications/st318/stat318.pdf.
Martin BC. Emergency medicine versus primary care: a case study of three prevalent, costly, and non-emergent diagnoses at a community teaching hospital. J Health Care Finance. 2000;27(2):51–65.
New England Healthcare Institute. A matter of urgency: reducing emergency department overuse A NEHI research brief. 2010.
Baker LC, Baker LS. Excess cost of emergency department visits for nonurgent care. Health Aff. 1994;13(5):162–71.
Pines JM, Hollander JE. Emergency department crowding is associated with poor care for patients with severe pain. Ann Emerg Med. 2008;51(1):1–5.
Carter EJ, et al. The relationship between emergency department crowding and patient outcomes: a systematic review. J Nurs Scholarsh. 2014;46(2):106–15.
Waste and Inefficiency in the U.S. Healthcare System. Clinical care: a comprehensive analysis in support of system-wide improvements. New England Healthcare Institute. 2008.
Lowe RA, Localio AR, Schwarz DF, et al. Association between primary care practice characteristics and emergency department use in a Medicaid managed care organization. Med Care. 2005;43(8):792–800.
Jayaprakash N, O’Sullivan R, Bey T, Ahmed S, Lotfipour S. Crowding and delivery of healthcare in emergency departments: the European perspective. West J Emerg Med. 2009;10(4):233–9.
Pines JM, Hilton JA, Weber EJ, Alkemade AJ, Al Shabanah H, Anderson PD, et al. International perspectives on emergency department crowding. Acad Emerg Med. 2011;18(12):1358–70.
Grumbach K, Bodenheimer T, Grundy, P. The outcomes of implementing patient-centered medical home interventions: a review of the evidence on quality, access and costs from recent prospective evaluation studies. Washington, DC: Patient-Centered Primary Care Collaborative; 2009. Available at: www.pcpcc.net/files/Grumbach_et-al_Evidence-of-Quality_%20101609_0.pdf. Accessed Nov 2013.
Franco SM, Mitchell CK, Buzon RM. Primary care physician access and gatekeeping: a key to reducing emergency department use. Clin Pediatr. 1997;36(2):63–8.
O’Connell JM, Johnson DA, Stallmayer J, et al. A satisfaction and return-on-investment of a nurse triage service. Am J Manag Care. 2001;7(2):159–69.
Manning WG, Newhouse JP, Duan N, et al. Health insurance and the demand for medical care. Santa Monica: The RAND Corporation; 1988.
Aron-Dine A, Einav L, Finkelstein A. The RAND health insurance experiment, three decades later. J Econ Perspect. 2013;27(1):197–222.
Zweifel P, Manning W. Moral hazard and consumer incentives in health care. In: Culyer A, Newhouse J, editors. Handbook of health economics. Oxford: North-Holland; 2000. p. 409–59.
Albert Ma CT, Riordan MH. Health insurance, moral hazard, and managed care. J Econ Manag Strategy. 2002;11(1):81–107.
Kanavos P. Pharmaceutical regulation in Europe. In: Institute for Research on Public Policy Conference – Toward a National Strategy on Drug Insurance: Challenges and Priorities, September 23 2002, Toronto, Ontario.
Newhouse J, The Insurance Experiment Group. Free for all? Lessons from the RAND Health insurance experiment. Cambridge: Harvard University Press; 1993.
Drummond M, Towse A. Is it time to reconsider the role of patient copayments for pharmaceuticals in Europe? Eur J Health Econ. 2012;13(1):1–5.
Atella V, Peracchi F, Depalo D, Rossetti C. Drug compliance, co-payment and health outcomes: evidence from a panel of Italian patients. Health Econ. 2006;15(9):875–92.
Austvoll-Dahlgren A, Aaserud M, Vist G, Ramsay C, Oxman AD, Sturm H, Kösters JP, Vernby A. Cochrane Database Syst Rev. 2008;23(1):CD007017. doi:10.1002/14651858.CD007017.
Wagstaff A, van Doorslaer E, Calonge S, Christiansen T, Gerfin M, Gottschalk P, Janssen R, Lachaud C, Leu RE, Nolan B, et al. Equity in the finance of health care: some international comparisons. J Health Econ. 1992;11(4):361–87.
De Graeve D, Van Ourti T. The distributional impact of health financing in Europe: a review. World Econ. 2003;26(10):1459–79.
Becker D, Blackburn J, Morrisey M, Sen B, Kilgore M, Caldwell C, Menachemi N. Co- payments and the use of emergency department services in the children’s health insurance program. Med Care Res Rev. 2013;70:514.
Falcone M, Fabozzi F, Bachini L. Tuscany case study health impact assessment tools: copayment policies evaluation Agenzia Regionale di Sanità Toscana, ITALY. Available at: https://www.ars.toscana.it/files/aree_intervento/indicatori_equita_qualita/equity_action/WP4_HIA_CASE_%20STUDY_Tuscany_2014.pdf.
Mortensen K. Departments copayments did not reduce medicaid enrollees’ nonemergency use of emergency. Health Aff. 2010;29(9):1643–50.
Ministry of Finance. Memorandum of understanding on specific economic policy conditionality. Nicosia: Republic of Cyprus, 2013.
Petrou P. The power of r-pharmaceutical sales decomposition in Cyprus public healthcare sector and determinants of drug expenditure evolution: any lessons learned? Expert Rev Pharmacoecon Outcomes Res. 2014;14(2):289–300.
Petrou P. Eurohealth financial crisis as a reform mediator in Cyprus’s health services Eurohealth incorporating euro observer. 2014;20(4).
Penfold RB, Zhang F. Use of interrupted time series analysis in evaluating health care quality improvements. Acad Pediatr. 2013;13:S38–44.
Ramsay C, Matowe L, Grilli R, Grimshaw J, Thomas R. Interrupted time series designs in health technology assessment: lessons from two systematic reviews of behavior change strategies. Int J Technol Assess Health Care. 2003;19(4):613–23
Yaffee R, McGee M. Introduction to Time Series Analysis and Forecasting with Applications of SAS and SPSS, San Diego: Academic Press, 2000
Effective Practice and Organisation of Care (EPOC). Interrupted time series (ITS) analyses. EPOC Resources for review authors. Oslo: Norwegian Knowledge Centre for the Health Services; 2015. Available at: http://epoc.cochrane.org/epoc-specific-resources-review-authors. Accessed 2015
Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002;27:299–309.
Box GEP, Jenkins GM. Time series analysis: forecasting and control. San Francisco: Holden-Day; 1976.
Biglan A, Ary D, Wagenaar AC. The value of interrupted time-series experiments for community intervention research. Prev Sci. 2000;1:31–49.
Witt SF, Witt CA. Forecasting tourism demand: a review of empirical research. Int J Forecast. 1995;11(3):447–90.
Lewis CD. Industrial and business forecasting methods: a practical guide to exponential smoothing and curve fitting. London: Butterworth Scientific; 1982
Shung-King M. The dilemmas of co-payment and moral hazard in the context of an NHI. HEU working paper. Cape Town, Health Economics Unit, University of Cape Town, 2011. Available at: http://uct-heu.s3.amazonaws.com/wp-content/uploads/2012/03/CO-PAYMENT-WORKING-PAPER.pdf. Accessed April 2015
Hsu J, Price M, Brand R, Ray GT, Fireman B, Newhouse JP, Selby JV. Cost-sharing for emergency care and unfavorable clinical events: findings from the safety and financial ramifications of ED copayments study. Health Serv Res. 2006;41:1801–20 (NO. 9 (2010): 1643–1650).
Kim J, Ko S, Yang B. The effects of patient cost sharing on ambulatory utilization in South Korea. Health Policy. 2005;72:293–300.
Lin YL, Hsiao CK, Ma HM, Hsu HY, Wang SM, Tseng YZ. The impact of National Health Insurance on the volume and severity of emergency department use. Am J Emerg Med. 1998;16:92–4.
Clinical Guidelines and Clinical Pathways Workshop. Cyprus Ministry of Health and National Institute for Health and care Excellence. 2014.
Chow SK, Wong FK, Chan TM, Chung LY, Chang KK, Lee RP. Community Nursing services for postdischarge chronically ill patients. J Clin Nurs. 2008;17(7B):260–71.
Efficiency in the Emergency Department. Doing things faster without sacrificing quality. ACEP Reference and Resource Guide American College of emergency practicians; 2004.
Cystat. Social protection report. Cyprus statistical services. Nicosia; 2013.
Rechel B, Doyle Y, Grundy E, McKee M. How can health systems respond to population ageing? Health Systems and Policy Analysis, World Health Organization 2009 and World Health Organization, on behalf of the European Observatory on Health Systems and Policies. 2009.
Rice T, Morrison KR. Patient cost sharing for medical services: a review of the literature and implications for health care reform. Med Care Rev. 1994;51(3):235–87.
Cherkin DC, Crothaus L, Wagner EH. Is magnitude of co-payment effect related to income? Using census data for health services research. Soc Sci Med. 1992;34:33–41.
Gelormino E, Bambra C, Spadea T, Bellini S, Costa G. The effects of health care reforms on health inequalities: a review and analysis of the european evidence base. Int J Health Serv. 2011;41(2):209–30.
Kellermann AL, Martinez R. The ER, 50 years on. N Engl J Med. 2011;364:2278–9.
NYU Center for Health and Public Service Research. ED ALGORITHM. Available at: http://wagner.nyu.edu/faculty/billings/nyued-background.
Theodorou M. Testing the waters for GeSY: patients’ opinion of cost-sharing arrangements in the public health care system in Cyprus. Cyprus Econ Policy Rev. 2014;8(2):37–59
Barish R, Mcgauly P, Arnold T. Emergency room crowding: a marker of hospital health. Trans Am Clin Climatol Assoc. 2012;123:304–10; discussion 310–1.
Asplin BR, Knopp RK. A room with a view: on-call specialist panels and other health policy challenges in the emergency department. Ann Emerg Med. 2001;37:500–3.
Acknowledgments
This study was approved by Cyprus Health Research Board (0059/2012). We are grateful to the Editor of the Journal, Tim Wrightson, and two anonymous referees for their constructive comments.
Funding
No funding was received.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Petrou, P. An Interrupted Time-Series Analysis to Assess Impact of Introduction of Co-Payment on Emergency Room Visits in Cyprus. Appl Health Econ Health Policy 13, 515–523 (2015). https://doi.org/10.1007/s40258-015-0169-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-015-0169-2