Abstract
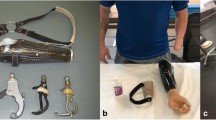
Osseointegration (OI) is the direct attachment of bone onto a titanium implant. Recently, the term is used to describe “transdermal” implants that allow an external prosthesis to be connected directly to the skeleton. This technology eliminates the challenges of conventional socket-based prostheses, such as skin breakdown and poor fit, which are common in patients with major extremity amputations. Osseointegration patients demonstrate encouraging improvements in quality of life and function. Patients report improvement in prosthetic use, prosthetic mobility, global health, and pain reduction on a variety of clinical assessment tools. Various implants have been developed for osseointegration for amputees. These implants use a variety of fixation strategies and surface augments to allow for successful integration into the host bone. Regardless of design, all OI implants face similar challenges, particularly infections. Other challenges include the inability to determine when integration has occurred and the inability to detect loss of integration. These challenges may be met by incorporating sensing systems into the implants. The percutaneous nature of the metal devices can be leveraged so that internal sensors need not be wireless, and can be interrogated by external monitoring systems, thus providing crucial, real-time information about the state of the implant. The purpose of this review is to (1) review the basic science behind osseointegration, (2) provide an overview of current implants, practice patterns, and clinical outcomes, and (3) preview sensor technologies which may prove useful in future generations of transdermal orthopaedic implants.


Similar content being viewed by others
References
Brånemark PI. Osseointegration and its experimental background. J Prosthet Dent. 1983;50:399–410.
Li Y, Brånemark R. Osseointegrated prostheses for rehabilitation following amputation: the pioneering Swedish model. Unfallchirurg. 2017;120:285–92.
Davies JE. Mechanisms of endosseous integration. Int J Prosthodont. 1998;11:391–401.
Alexander KA, Raggatt L-J, Millard S, Batoon L, Chiu-Ku WuA, Chang M-K, et al. Resting and injury-induced inflamed periosteum contain multiple macrophage subsets that are located at sites of bone growth and regeneration. Immunol Cell Biol. 2017;95:7–16.
Franchi M, Fini M, Martini D, Orsini E, Leonardi L, Ruggeri A, et al. Biological fixation of endosseous implants. Micron. 2005;36:665–71.
Berglundh T, Abrahamsson I, Lang NP, Lindhe J. De novo alveolar bone formation adjacent to endosseous implants. Clin Oral Implants Res. 2003;14:251–62.
Nguyen TS, Lapidot T, Ruf W. Extravascular coagulation in hematopoietic stem and progenitor cell regulation. Blood. 2018;132:123–31.
Meyer U, Joos U, Mythili J, Stamm T, Hohoff A, Fillies T, et al. Ultrastructural characterization of the implant/bone interface of immediately loaded dental implants. Biomaterials. 2004;25:1959–67.
Hesketh M, Sahin KB, West ZE, Murray RZ. Macrophage phenotypes regulate scar formation and chronic wound healing. Int J Mol Sci. 2017;18:1545.
Lévesque J-P, Helwani FM, Winkler IG. The endosteal “osteoblastic” niche and its role in hematopoietic stem cell homing and mobilization. Leukemia. 2010;24:1979–92.
Linder L, Albrektsson T, Brånemark PI, Hansson HA, Ivarsson B, Jönsson U, et al. Electron microscopic analysis of the bone-titanium interface. Acta Orthop Scand. 1983;54:45–52.
Stanford CM, Keller JC. The concept of osseointegration and bone matrix expression. Crit Rev Oral Biol Med. 1991;2:83–101.
Søballe K. Hydroxyapatite ceramic coating for bone implant fixation. Mechanical and histological studies in dogs. Acta Orthop Scand Suppl. 1993;255:1–58.
Munting E. The contributions and limitations of hydroxyapatite coatings to implant fixation: A histomorphometric study of load bearing implants in dogs. Int Orthop. 1996;20:1–6.
Van Hamersveld KT, Marang-Van De Mheen PJ, Nelissen RGHH, Toksvig-Larsen S. Peri-apatite coating decreases uncemented tibial component migration: long-term RSA results of a randomized controlled trial and limitations of short-term results. Acta Orthop. 2018;89:425–30.
King S, Klineberg I, Levinger I, Brennan-Speranza TC. The effect of hyperglycaemia on osseointegration: a review of animal models of diabetes mellitus and titanium implant placement. Arch Osteoporos. 2016;11:29.
Dereka X, Calciolari E, Donos N, Mardas N. Osseointegration in osteoporotic-like condition: a systematic review of preclinical studies. J Periodont Res. 2018;53:933–40.
Søballe K, Hansen ES, Brockstedt-Rasmussen H, Hjortdal VE, Juhl GI, Pedersen CM, et al. Fixation of titanium and hydroxyapatite-coated implants in arthritic osteopenic bone. J Arthroplasty. 1991;6:307–16.
Li JY, Pow EHN, Zheng LW, Ma L, Kwong DLW, Cheung LK. Dose-dependent effect of radiation on titanium implants: a quantitative study in rabbits. Clin Oral Implants Res. 2014;25:260–5.
Al-Mahalawy H, Marei HF, Abuohashish H, Alhawaj H, Alrefaee M, Al-Jandan B. Effects of cisplatin chemotherapy on the osseointegration of titanium implants. J Craniomaxillofac Surg. 2016;44:337–46.
DDS OEO. Implant surface material, design, and osseointegration. Dent Clin NA. 2015;59:505–20.
Baggi L, Di Girolamo M, Vairo G, Sannino G. Comparative evaluation of osseointegrated dental implants based on platform-switching concept: influence of diameter, length, thread shape, and in-bone positioning depth on stress-based performance. Comput Math Methods Med. 2013;2013:250929–35.
Barikani H, Rashtak S, Akbari S, Badri S, Daneshparvar N, Rokn A. The effect of implant length and diameter on the primary stability in different bone types. J Dent (Tehran). 2013;10:449–55.
Kruyt IJ, Nelissen RC, Mylanus EAM, Hol MKS. Three-year outcomes of a randomized controlled trial comparing a 4.5-mm-wide to a 3.75-mm-wide titanium implant for bone conduction hearing. Otol Neurotol. 2018;39:609–15.
Baggi L, Cappelloni I, Di Girolamo M, Maceri F, Vairo G. The influence of implant diameter and length on stress distribution of osseointegrated implants related to crestal bone geometry: a three-dimensional finite element analysis. J Prosthet Dent. 2008;100:422–31.
Anitua E, Tapia R, Luzuriaga F, Orive G. Influence of implant length, diameter, and geometry on stress distribution: a finite element analysis. Int J Periodontics Restor Dent. 2010;30:89–95.
Orsini E, Giavaresi G, Trirè A, Ottani V, Salgarello S. Dental implant thread pitch and its influence on the osseointegration process: an in vivo comparison study. Int J Oral Maxillofac Implants. 2012;27:383–92.
Chung SH, Heo SJ, Koak JY, Kim SK, Lee JB, Han JS, et al. Effects of implant geometry and surface treatment on osseointegration after functional loading: a dog study. J Oral Rehabil. 2008;35:229–36.
Ausiello P, Franciosa P, Martorelli M, Watts DC. Effects of thread features in osseo-integrated titanium implants using a statistics-based finite element method. Dent Mater. 2012;28:919–27.
Goriainov V, Cook R, Latham JM, Dunlop DG, Oreffo ROC. Bone and metal: an orthopaedic perspective on osseointegration of metals. Acta Biomater. 2014;10:4043–57.
Isaacson BM, Orthopedic SJ. Osseointegration: a review of the fundamentals for assuring cementless skeletal fixation, 300AD. Orthop Res Rev. 2014;6:55.
Mantripragada VP, Czernik BL, Ebraheim NA, Jayasuriya AC. An overview of recent advances in designing orthopedic and craniofacial implants. J Biomed Mater Res A. 2013;101:3349–64.
Lewallen EA, Riester SM, Bonin CA, Kremers HM, Dudakovic A, Kakar S, et al. Biological strategies for improved osseointegration and osteoinduction of porous metal orthopedic implants. Tissue Eng Part B Rev. 2015;21:218–30.
Kumar V, Gill KD. Aluminium neurotoxicity: neurobehavioural and oxidative aspects. Arch Toxicol. 2009;83:965–78.
Abdel-Hady Gepreel M, Niinomi M. Biocompatibility of Ti-alloys for long-term implantation. J Mech Behav Biomed Mater. 2013;20:407–15.
Eisenbarth E, Velten D, Müller M, Thull R, Breme J. Biocompatibility of beta-stabilizing elements of titanium alloys. Biomaterials. 2004;25:5705–13.
Jarmar T, Palmquist A, Brånemark R, Hermansson L, Engqvist H, Thomsen P. Characterization of the surface properties of commercially available dental implants using scanning electron microscopy, focused ion beam, and high-resolution transmission electron microscopy. Clin Implant Dent Relat Res. 2008;10:11–22.
Nishiguchi S, Nakamura T, Kobayashi M, Kim HM, Miyaji F, Kokubo T. The effect of heat treatment on bone-bonding ability of alkali-treated titanium. Biomaterials. 1999;20:491–500.
Pałka K, Pokrowiecki R. Porous titanium implants: a review. Adv Eng Mater. 2018;20:1700648.
de Vasconcellos LMR, Leite DO, de Oliveira FN, Carvalho YR, Cairo CAA. Evaluation of bone ingrowth into porous titanium implant: histomorphometric analysis in rabbits. Braz Oral Res. 2010;24:399–405.
Taniguchi N, Fujibayashi S, Takemoto M, Sasaki K, Otsuki B, Nakamura T, et al. Effect of pore size on bone ingrowth into porous titanium implants fabricated by additive manufacturing: an in vivo experiment. Mater Sci Eng C. 2016;59:690–701.
Chastand V, Tezenas A, Cadoret Y, Quaegebeur P, Maia W, Charkaluk E. Fatigue characterization of Titanium Ti–6Al–4V samples produced by Additive Manufacturing. Procedia Struct Integr. 2016;2:3168–76.
Tillander J, Hagberg K, Hagberg L, Brånemark R. Osseointegrated titanium implants for limb prostheses attachments: infectious complications. Clin Orthop Relat Res. 2010;468:2781–8.
Kunutsor SK, Gillatt D, Blom AW. Systematic review of the safety and efficacy of osseointegration prosthesis after limb amputation. Br J Surg. 2018;105:1731–41.
Tsikandylakis G, Berlin Ö, Brånemark R. Implant survival, adverse events, and bone remodeling of osseointegrated percutaneous implants for transhumeral amputees. Clin Orthop Relat Res. 2014;472:2947–56.
Brånemark R, Berlin O, Hagberg K, Bergh P, Gunterberg B, Rydevik B. A novel osseointegrated percutaneous prosthetic system for the treatment of patients with transfemoral amputation: a prospective study of 51 patients. Bone Joint J. 2014;96-B:106–13.
Atsuta I, Ayukawa Y, Kondo R, Oshiro W, Matsuura Y, Furuhashi A, et al. Soft tissue sealing around dental implants based on histological interpretation. J Prosthodont Res. 2016;60:3–11.
Chen J, Zhu Y, Xiong M, Hu G, Zhan J, Li T, et al. Antimicrobial titanium surface via click-immobilization of peptide and its in vitro/vivo activity. ACS Biomater Sci Eng. 2018;5:1034–44.
Campoccia D, Montanaro L, Speziale P, Arciola CR. Antibiotic-loaded biomaterials and the risks for the spread of antibiotic resistance following their prophylactic and therapeutic clinical use. Biomaterials. 2010;31:6363–77.
Zilberman M, Elsner JJ. Antibiotic-eluting medical devices for various applications. J Control Release. 2008;130:202–15.
Hickok NJ, Shapiro IM, Chen AF. The impact of incorporating antimicrobials into implant surfaces. J Dent Res. 2018;97:14–22.
Jeyapalina S, Beck JP, Bachus KN, Williams DL, Bloebaum RD. Efficacy of a porous-structured titanium subdermal barrier for preventing infection in percutaneous osseointegrated prostheses. J Orthop Res. 2012;30:1304–11.
Pendegrass CJ, Goodship AE, Blunn GW. Development of a soft tissue seal around bone-anchored transcutaneous amputation prostheses. Biomaterials. 2006;27:4183–91.
Koidou VP, Argyris PP, Skoe EP, Mota Siqueira J, Chen X, Zhang L, et al. Peptide coatings enhance keratinocyte attachment towards improving the peri-implant mucosal seal. Biomater Sci. 2018;6:1936–45.
Pendegrass CJ, El-Husseiny M, Blunn GW. The development of fibronectin-functionalised hydroxyapatite coatings to improve dermal fibroblast attachment in vitro. J Bone Joint Surg Br Vol. 2012;94:564–9.
Pendegrass CJ, Tucker B, Patel S, Dowling R, Blunn GW. The effect of adherens junction components on keratinocyte adhesion in vitro: potential implications for sealing the skin-implant interface of intraosseous transcutaneous amputation prostheses. J Biomed Mater Res A. 2012;100:3463–71.
Gordon DJ, Bhagawati DD, Pendegrass CJ, Middleton CA, Blunn GW. Modification of titanium alloy surfaces for percutaneous implants by covalently attaching laminin. J Biomed Mater Res A. 2010;94:586–93.
Kinumatsu T, Hashimoto S, Muramatsu T, Sasaki H, Jung H-S, Yamada S, et al. Involvement of laminin and integrins in adhesion and migration of junctional epithelium cells. J Periodont Res. 2009;44:13–20.
Kim J-M, Park WH, Min B-M. The PPFLMLLKGSTR motif in globular domain 3 of the human laminin-5 alpha3 chain is crucial for integrin alpha3beta1 binding and cell adhesion. Exp Cell Res. 2005;304:317–27.
Min S-K, Lee S-C, Hong S-D, Chung C-P, Park WH, Min B-M. The effect of a laminin-5-derived peptide coated onto chitin microfibers on re-epithelialization in early-stage wound healing. Biomaterials. 2010;31:4725–30.
Zhang J, Wang H, Wang Y, Dong W, Jiang Z, Yang G. Substrate-mediated gene transduction of LAMA3 for promoting biological sealing between titanium surface and gingival epithelium. Colloids Surf B Biointerfaces. 2018;161:314–23.
Albrektsson T, Brånemark PI, Hansson HA, Lindström J. Osseointegrated titanium implants. Requirements for ensuring a long-lasting, direct bone-to-implant anchorage in man. Acta Orthop Scand. 1981;52:155–70.
Webster JB, Bachus KN, Beck JP, Jeyapalina S, Drew AJ, Bloebaum RD. Osseointegration research. Full stride. New York: Springer; 2017. p. 167–93.
Maryniak A, Laschowski B, Andrysek J. Technical overview of osseointegrated transfemoral prostheses: orthopedic surgery and implant design centered. ASME J Med Diagn. 2018;1:020801.
Nebergall A, Bragdon C, Antonellis A, Kärrholm J, Brånemark R, Malchau H. Stable fixation of an osseointegated implant system for above-the-knee amputees. Acta Orthop. 2012;83:121–8.
Hagberg K, Brånemark R, Gunterberg B, Rydevik B. Osseointegrated trans-femoral amputation prostheses: prospective results of general and condition-specific quality of life in 18 patients at 2-year follow-up. Prosthet Orthot Int. 2008;32:29–41.
Hagberg K, Brånemark R. One hundred patients treated with osseointegrated transfemoral amputation prostheses–rehabilitation perspective. J Rehabil Res Dev. 2009;46:331–44.
Matthews DJ, Arastu M, Uden M, Sullivan JP, Bolsakova K, Robinson K, et al. UK trial of the osseointegrated prosthesis for the rehabilitation for amputees: 1995–2018. Prosthet Orthot Int. 2018;82:1–11.
Thesleff A, Brånemark R, Håkansson B, Ortiz-Catalan M. Biomechanical characterisation of bone-anchored implant systems for amputation limb prostheses: a systematic review. Ann Biomed Eng. 2018;46:377–91.
McGough RL, Goodman MA, Randall RL, Forsberg JA, Potter BK, Lindsey B. The Compress® transcutaneous implant for rehabilitation following limb amputation. Unfallchirurg. 2017;120:300–5.
Pedtke AC, Wustrack RL, Fang AS, Grimer RJ, O’Donnell RJ. Aseptic failure: how does the Compress(®) implant compare to cemented stems? Clin Orthop Relat Res. 2012;470:735–42.
Zimel MN, Farfalli GL, Zindman AM, Riedel ER, Morris CD, Boland PJ, et al. Revision distal femoral arthroplasty with the Compress(®) prosthesis has a low rate of mechanical failure at 10 years. Clin Orthop Relat Res. 2016;474:528–36.
Korabi R, Shemtov-Yona K, Rittel D. On stress/strain shielding and the material stiffness paradigm for dental implants. Clin Implant Dent Relat Res. 2017;19:935–43.
Denard PJ, Raiss P, Gobezie R, Edwards TB, Lederman E. Stress shielding of the humerus in press-fit anatomic shoulder arthroplasty: review and recommendations for evaluation. J Shoulder Elbow Surg. 2018;27:1139–47.
Huiskes R, Weinans H, van Rietbergen B. The relationship between stress shielding and bone resorption around total hip stems and the effects of flexible materials. Clin Orthop Relat Res. 1992;274:124–34.
Kagan R, Adams J, Schulman C, Laursen R, Espana K, Yoo J, et al. What factors are associated with failure of compressive osseointegration fixation? Clin Orthop Relat Res. 2016;475:698–704.
Tyler WK, Healey JH, Morris CD, Boland PJ, O’Donnell RJ. Compress periprosthetic fractures: interface stability and ease of revision. Clin Orthop Relat Res. 2009;467:2800–6.
Kancherla VK, Del Gaizo DJ, Paprosky WG, Sporer SM. Utility of trephine reamers in revision hip arthroplasty. J Arthroplasty. 2014;29:210–3.
Juhnke D-L, Beck JP, Jeyapalina S, Aschoff HH. Fifteen years of experience with Integral-Leg-Prosthesis: cohort study of artificial limb attachment system. J Rehabil Res Dev. 2015;52:407–20.
Frölke JPM, Leijendekkers RA, van de Meent H. Osseointegrated prosthesis for patients with an amputation: multidisciplinary team approach in the Netherlands. Unfallchirurg. 2017;120:293–9.
Muderis Al M, Lu W, Li JJ. Osseointegrated Prosthetic Limb for the treatment of lower limb amputations: experience and outcomes. Unfallchirurg. 2017;120:306–11.
Muderis Al M, Khemka A, Lord SJ, Van de Meent H, Frölke JPM. Safety of osseointegrated implants for transfemoral amputees. J Bone Joint Surg Am Vol. 2016;98:900–9.
Muderis MA, Tetsworth K, Khemka A, Wilmot S, Bosley B, Lord SJ, et al. The Osseointegration Group of Australia Accelerated Protocol (OGAAP-1) for two-stage osseointegrated reconstruction of amputated limbs. Bone Joint J. 2016;98:952–60.
Muderis MA, Lu W, Glatt V, Tetsworth K. Two-stage osseointegrated reconstruction of post-traumatic unilateral transfemoral amputees. Mil Med. 2018;183:496–502.
Atallah R, Li JJ, Lu W, Leijendekkers R, Frölke JP, Muderis Al M. Osseointegrated transtibial implants in patients with peripheral vascular disease. J Bone Joint Surg Am Vol. 2017;99:1516–23.
Leijendekkers RA, van Hinte G, Nijhuis-van der Sanden MW, Staal JB. Gait rehabilitation for a patient with an osseointegrated prosthesis following transfemoral amputation. Physiother Theory Pract. 2017;33:147–61.
Hebert JS, Rehani M, Stiegelmar R. Osseointegration for lower-limb amputation: a systematic review of clinical outcomes. JBJS Rev. 2017;5:e10.
Van de Meent H, Hopman MT, Frölke JP. Walking ability and quality of life in subjects with transfemoral amputation: a comparison of osseointegration with socket prostheses. Arch Phys Med Rehabil. 2013;94:2174–8.
Jacobs R, Brånemark R, Olmarker K, Rydevik B, Van Steenberghe D, Brånemark PI. Evaluation of the psychophysical detection threshold level for vibrotactile and pressure stimulation of prosthetic limbs using bone anchorage or soft tissue support. Prosthet Orthot Int. 2000;24:133–42.
Lapin B, Thompson NR, Schuster A, Katzan IL. Clinical utility of patient-reported outcome measurement information system domain scales. Circ Cardiovasc Qual Outcomes. 2019;12:e004753.
Sullivan J, Uden M, Robinson KP, Sooriakumaran S. Rehabilitation of the trans-femoral amputee with an osseointegrated prosthesis: the United Kingdom experience. Prosthet Orthot Int. 2003;27:114–20.
He J, Chen J, Hu G, Wang L, Zheng J, Zhan J, et al. Immobilization of an antimicrobial peptide on silicon surface with stable activity by click chemistry. J Mater Chem B. 2018;6:68–74.
Zhao L, Wang H, Huo K, Cui L, Zhang W, Ni H, et al. Antibacterial nano-structured titania coating incorporated with silver nanoparticles. Biomaterials. 2011;32:5706–16.
Lucke M, Schmidmaier G, Sadoni S, Wildemann B, Schiller R, Haas NP, et al. Gentamicin coating of metallic implants reduces implant-related osteomyelitis in rats. Bone. 2003;32:521–31.
Hetrick EM, Schoenfisch MH. Reducing implant-related infections: active release strategies. Chem Soc Rev. 2006;35:780–9.
Ehrensberger MT, Tobias ME, Nodzo SR, Hansen LA, Luke-Marshall NR, Cole RF, et al. Cathodic voltage-controlled electrical stimulation of titanium implants as treatment for methicillin-resistant Staphylococcus aureus periprosthetic infections. Biomaterials. 2015;41:97–105.
Poortinga AT, Smit J, van der Mei HC, Busscher HJ. Electric field induced desorption of bacteria from a conditioning film covered substratum. Biotechnol Bioeng. 2001;76:395–9.
Blenkinsopp SA, Khoury AE, Costerton JW. Electrical enhancement of biocide efficacy against Pseudomonas aeruginosa biofilms. Appl Environ Microbiol. 1992;58:3770–3.
Nodzo SR, Tobias M, Ahn R, Hansen L, Luke-Marshall NR, Howard C, et al. Cathodic voltage-controlled electrical stimulation plus prolonged vancomycin reduce bacterial burden of a titanium implant-associated infection in a rodent model. Clin Orthop Relat Res. 2016;474:1668–75.
Canty M, Luke-Marshall N, Campagnari A, Ehrensberger M. Cathodic voltage-controlled electrical stimulation of titanium for prevention of methicillin-resistant Staphylococcus aureus and Acinetobacter baumannii biofilm infections. Acta Biomater. 2017;48:451–60.
Gupta S, Loh KJ. Noncontact electrical permittivity mapping and pH-sensitive films for osseointegrated prosthesis and infection monitoring. IEEE Trans Med Imaging. 2017;36:2193–203.
Frossard LA. Load on osseointegrated fixation of a transfemoral amputee during a fall: determination of the time and duration of descent. Prosthet Orthot Int. 2010;34:472–87.
Gupta S, Lee H-J, Loh KJ, Todd MD, Reed J, Barnett AD. Noncontact strain monitoring of osseointegrated prostheses. Sensors (Basel). 2018;18:3015.
Vien BS, Chiu WK, Russ M, Fitzgerald M. A quantitative approach for the bone-implant osseointegration assessment based on ultrasonic elastic guided waves. Sensors. 2019;19:454.
Wang Y, Lynch JP, Law KH. A wireless structural health monitoring system with multithreaded sensing devices: design and validation. Struct Infrastruct Eng. 2007;3:103–20.
Lynch JP. Design of a wireless active sensing unit for localized structural health monitoring. Struct Control Health Monit. 2005;12:405–23.
Ortiz-Catalan M, Håkansson B, Brånemark R. An osseointegrated human-machine gateway for long-term sensory feedback and motor control of artificial limbs. Sci Transl Med. 2014;6:257re6.
Funding
No funding was used in creating this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Both author declares that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The designated authors are employees of the US Government. This work was prepared as part of their official duties. Title 17 U.S.C. §105 provides that “Copyright protection under this title is not available for any work of the United States Government.” Title 17 U.S.C. §101 defined a US Government work as a work prepared by a military service member or employees of the US Government as part of that person’s official duties. The opinions or assertions contained in this paper are the private views of the authors and are not to be construed as reflecting the views, policy or positions of the Department of the Navy, Department of the Army, Department of Defense nor the US Government.
Rights and permissions
About this article
Cite this article
Overmann, A.L., Forsberg, J.A. The state of the art of osseointegration for limb prosthesis. Biomed. Eng. Lett. 10, 5–16 (2020). https://doi.org/10.1007/s13534-019-00133-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13534-019-00133-9