Abstract
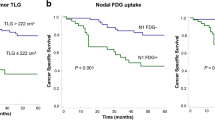
This study aimed to evaluate the clinical correlations between serum lactate dehydrogenase (LDH) levels and tumor characteristics and to investigate the prognostic impact of serum LDH levels in advanced non-small cell lung cancer (NSCLC). A total of 394 patients were included in the present study between June 2007 and January 2013. All eligible patients had serum LDH levels available before treatment, and whole-body metastatic extent was measured using whole-body metastatic scores, as determined by 18(F)-fludeoxyglucose positron emission tomography scans from 1 to 7 as the sum of each metastatic region. The diagnostic cutoff value for an abnormal serum LDH level was 450 IU/L. The median serum LDH level was 477 IU/L (range, 113–2850), and 224 (56.9 %) patients had abnormal serum LDH levels. The serum LDH levels showed no significant associations with age, gender, histology, tumor differentiation, and smoking history. However, the proportion of patients with abnormal serum LDH levels was statistically significantly higher in the high total metastatic score group (scores 3–7) than in the low total metastatic score group (scores 1–2) (65.3 vs 50.4 %, p = 0.001). In a multivariate survival analysis, age (p = 0.001), gender (p = 0.001), histology (p = 0.003), tumor differentiation (p = 0.001), Eastern Cooperative Oncology Group (ECOG) performance status (p = 0.001), LDH levels (p = 0.046), and treatment factors (p = 0.001) proved to be independent prognostic factors for survival outcomes. The results of this study suggest that the serum LDH levels at presentation may be significantly correlated with whole-body tumor extent and might independently but modestly prognosticate OS in stage IV NSCLC.

Similar content being viewed by others
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90.
O'Connell JP, Kris MG, Gralla RJ, Groshen S, Trust A, Fiore JJ, et al. Frequency and prognostic importance of pretreatment clinical characteristics in patients with advanced non-small-cell lung cancer treated with combination chemotherapy. J Clin Oncol. 1986;4:1604–14.
Albain KS, Crowley JJ, LeBlanc M, Livingston RB. Survival determinants in extensive-stage non-small-cell lung cancer: the Southwest Oncology Group experience. J Clin Oncol. 1991;9:1618–26.
Espinosa E, Feliu J, Zamora P, Gonzalez Baron M, Sanchez JJ, Ordon EZA, et al. Serum albumin and other prognostic factors related to response and survival in patients with advanced non-small cell lung cancer. Lung Cancer. 1995;12:67–76.
Hespanhol V, Queiroga H, Magalhaes A, Santos AR, Coelho M, Marques A. Survival predictors in advanced non-small cell lung cancer. Lung Cancer. 1995;13:253–67.
Ando M, Ando Y, Hasegawa Y, Shimokata K, Minami H, Wakai K, et al. Prognostic value of performance status assessed by patients themselves, nurses, and oncologists in advanced non-small cell lung cancer. Br J Cancer. 2001;85:1634–9.
Klastersky J, Paesmans M. Response to chemotherapy, quality of life benefits and survival in advanced non-small cell lung cancer: review of literature results. Lung Cancer. 2001;34 Suppl 4:S95–101.
Jeremic B, Milicic B, Dagovic A, Aleksandrovic J, Nikolic N. Pretreatment clinical prognostic factors in patients with stage IV non-small cell lung cancer (NSCLC) treated with chemotherapy. J Cancer Res Clin Oncol. 2003;129:114–22.
Toh CK. The changing epidemiology of lung cancer. Methods Mol Biol. 2009;472:397–411.
Konopa K, Jassem J. The role of pemetrexed combined with targeted agents for non-small cell lung cancer. Curr Drug Targets. 2010;11:2–11.
Somaiah N, Simon GR. Molecular targeted agents and biologic therapies for non-small cell lung cancer. J Thorac Oncol. 2010;5:S434–54.
Tas F, Aydiner A, Demir C, Topuz E. Serum lactate dehydrogenase levels at presentation predict outcome of patients with limited-stage small-cell lung cancer. Am J Clin Oncol. 2001;24:376–8.
Koukourakis MI, Giatromanolaki A, Sivridis E, Bougioukas G, Didilis V, Gatter KC, et al. Lactate dehydrogenase-5 (LDH-5) overexpression in non-small-cell lung cancer tissues is linked to tumour hypoxia, angiogenic factor production and poor prognosis. Br J Cancer. 2003;89:877–85.
Koukourakis MI, Giatromanolaki A, Sivridis E. Tumour, Angiogenesis Research G. Lactate dehydrogenase isoenzymes 1 and 5: differential expression by neoplastic and stromal cells in non-small cell lung cancer and other epithelial malignant tumors. Tumour Biol. 2003;24:199–202.
Scartozzi M, Giampieri R, Maccaroni E, Del Prete M, Faloppi L, Bianconi M, et al. Pre-treatment lactate dehydrogenase levels as predictor of efficacy of first-line bevacizumab-based therapy in metastatic colorectal cancer patients. Br J Cancer. 2012;106:799–804.
Faloppi L, Scartozzi M, Bianconi M, Svegliati Baroni G, Toniutto P, Giampieri R, et al. The role of LDH serum levels in predicting global outcome in HCC patients treated with sorafenib: implications for clinical management. BMC Cancer. 2014;14:110.
Watine J. Prognostic evaluation of primary non-small cell lung carcinoma patients using biological fluid variables. A systematic review. Scand J Clin Lab Invest. 2000;60:259–73.
Wang S, Han X, Hu X, Wang X, Zhao L, Tang L, et al. Clinical significance of pretreatment plasma biomarkers in advanced non-small cell lung cancer patients. Clin Chim Acta. 2014;430:63–70.
Lee DS, Kim SJ, Kang JH, Hong SH, Jeon EK, Kim YK, et al. Serum carcinoembryonic antigen levels and the risk of whole-body metastatic potential in advanced non-small cell lung cancer. J Cancer. 2014;5:663–9.
Lee DS, Kim YS, Jung SL, Lee KY, Kang JH, Park S, et al. The relevance of serum carcinoembryonic antigen as an indicator of brain metastasis detection in advanced non-small cell lung cancer. Tumour Biol. 2012;33:1065–73.
Lee DS, Kang JH, Lee CG, Kim SJ, Choi YJ, Lee KY, et al. Predicting survival in patients with advanced non-squamous non-small cell lung cancer: validating the extent of metastasis. Cancer Res Treat. 2013;45:95–102.
Cerny T, Blair V, Anderson H, Bramwell V, Thatcher N. Pretreatment prognostic factors and scoring system in 407 small-cell lung cancer patients. Int J Cancer. 1987;39:146–9.
Byhardt RW, Hartz A, Libnoch JA, Hansen R, Cox JD. Prognostic influence of TNM staging and LDH levels in small cell carcinoma of the lung (SCCL). Int J Radiat Oncol Biol Phys. 1986;12:771–7.
Ferrigno D, Buccheri G, Camilla T. Serum copper and zinc content in non-small cell lung cancer: abnormalities and clinical correlates. Monaldi Arch Chest Dis. 1999;54:204–8.
Ray P, Quantin X, Grenier J, Pujol JL. Predictive factors of tumor response and prognostic factors of survival during lung cancer chemotherapy. Cancer Detect Prev. 1998;22:293–304.
Goldman RD, Kaplan NO, Hall TC. Lactic dehydrogenase in human neoplastic tissues. Cancer Res. 1964;24:389–99.
Koukourakis MI, Giatromanolaki A, Sivridis E, Gatter KC, Trarbach T, Folprecht G, et al. Prognostic and predictive role of lactate dehydrogenase 5 expression in colorectal cancer patients treated with PTK787/ZK 222584 (vatalanib) antiangiogenic therapy. Clin Cancer Res. 2011;17:4892–900.
Yang Y, Su D, Zhao L, Zhang D, Xu J, Wan J, et al. Different effects of LDH-A inhibition by oxamate in non-small cell lung cancer cells. Oncotarget. 2014;5:11886–96.
Charloux A, Quoix E, Wolkove N, Small D, Pauli G, Kreisman H. The increasing incidence of lung adenocarcinoma: reality or artefact? A review of the epidemiology of lung adenocarcinoma. Int J Epidemiol. 1997;26:14–23.
Uhm JE, Park BB, Ahn MJ, Lee J, Ahn JS, Kim SW, et al. Erlotinib monotherapy for stage IIIB/IV non-small cell lung cancer: a multicenter trial by the Korean Cancer Study Group. J Thorac Oncol. 2009;4:1136–43.
Conflict of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, D.S., Park, K.R., Kim, S.J. et al. Serum lactate dehydrogenase levels at presentation in stage IV non-small cell lung cancer: predictive value of metastases and relation to survival outcomes. Tumor Biol. 37, 619–625 (2016). https://doi.org/10.1007/s13277-015-3776-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-015-3776-5