Abstract
The epidemiology of lung cancer differs between men and women. The role of androgens in lung cancer remains unclear. This study was performed to determine if exposure to androgen pathway manipulation (APM) is associated with greater survival in male patients diagnosed with lung cancer. Using a retrospective cohort design, all men diagnosed with lung cancer from January 1, 2004 to December 31, 2010 were identified from the population-based Manitoba Cancer Registry and Manitoba Health Administrative Databases. Information from the Drug Program Information Network (DPIN) was used to determine prescriptions filled for antiandrogens, 5-alpha reductase inhibitors, and gonadotropin-releasing hormone (GnRH) agonists. Multivariable Cox proportional hazards analysis with time-varying exposure variables was used to compare survival. A total of 3018 men with lung cancer were identified between 2004 and 2010. Of these, 339 (11.5 %) were identified as having used a form of APM. The majority of patients received 5-alpha reductase inhibitors. Patients who received APM prior to the diagnosis of lung cancer had no significant difference in survival (HR 0.97, p = 0.69) compared to those who did not. Patients exposed to APM after their diagnosis were found to have a significantly better survival (HR 0.36, p = 0.0007), as were those exposed both before and after diagnosis (HR 0.53, p < 0.0001). In male patients diagnosed with lung cancer, exposure to APM is associated with significantly better survival when compared with no exposure. The association is only seen when some or all of the exposure has occurred after the diagnosis of lung cancer.
Similar content being viewed by others
Introduction
It is estimated that 20,500 people will have died of lung cancer in Canada during 2014 [1]. Lung cancer continues to be the leading cause of cancer-related death; however, differences in the epidemiology of lung cancer exist between males and females. The incidence and mortality of lung cancer in males has been dropping steadily since the 1980s; however, mortality has only now begun to plateau in Canadian women [1]. The proportion of histological subtypes differs as well, with adenocarcinoma and bronchioloalveolar carcinoma being more common among women [2, 3]. There is also a difference in survival between men and women, with recent evidence suggesting that female sex is an independent good prognostic factor accounting for age, histology, treatment, and year of diagnosis [2, 4]. These observations suggest that sex hormones may have a role in lung cancer pathophysiology.
While lung cancer is not classically thought to be a hormone-sensitive malignancy, there is data suggesting that androgens may have a role in lung cancer pathophysiology. The androgen receptor (AR) is present in normal human lung, non-small cell, and small cell lung cancer tissue [5–7]. Testosterone has been shown to stimulate the growth of small cell lung cancer cell lines which express the AR [7]. In AR-positive murine lung tissue and human non-small cell lung cancer (NSCLC) cell lines, gene expression is significantly altered upon exposure to androgens [8]. In particular, genes involved in oxygen transport and utilization are upregulated, while genes involved in DNA repair and DNA recombination are downregulated [8]. Further data from in vitro analyses indicate a significant growth response to dihydrotestosterone (DHT) exposure in lung cancer cell lines with an AR-specific pattern of mRNA expression [9]. Recent work using archival tissue from 64 patients with stage II/III NSCLC treated with radiation found that the AR was expressed in 31 % of patients; however, it was not an independent prognostic factor in this group [10]. Interestingly, patients with advanced or recurrent NSCLC treated with the epidermal growth factor receptor (EGFR) tyrosine kinase inhibitor gefitinib had significantly lower androgen levels post-treatment, and lower androgen levels were associated with response to gefitinib in women [11]. While these findings suggest a possible role of the androgen pathway in the biology of lung cancer, it remains unknown whether direct manipulation of the pathway may have an effect on clinical outcomes.
The androgen pathway can be manipulated by a variety of medications. 5-alpha reductase inhibitors such as finasteride function by competitively inhibiting 5-alpha reductase, which is responsible for converting testosterone to DHT [12]. Non-steroidal antiandrogens, which include bicalutamide, nilutamide, and flutamide, bind to the androgen receptor itself and competitively inhibit the action of testosterone and DHT [13]. Cyproterone acetate is a steroidal antiandrogen, which, in addition to competitively inhibiting the action of androgens, also inhibits luteinizing hormone (LH) secretion leading to decreased testosterone production [13]. The gonadotropin-releasing hormone (GnRH) agonists include buserelin, goserelin, and leuprolide. After an initial surge in LH and testosterone, GnRH receptors are downregulated via negative feedback, leading to a drop in LH and eventually testosterone [14]. While other medications such as spironolactone and ketoconazole have antiandrogenic properties, this article will focus on the medications listed above.
Manitoba is a Canadian province with a stable population of 1.2 million and a publicly funded health care system. Approximately 800 new cases of lung cancer are diagnosed each year. All neoplastic diagnoses are recorded in the Manitoba Cancer Registry (MCR). The Manitoba Health administrative databases prospectively collect physician claim information and all outpatient prescription medications dispensed in Manitoba. We compiled a cohort of all patients diagnosed with lung cancer in Manitoba between 2004 and 2010 and identified those undergoing androgen pathway manipulation (APM) using information from the administrative data. Using this population-based cohort, we tested the hypothesis that exposure to APM will have an impact on survival in males with lung cancer.
Methods
Data Sources
All neoplastic diagnoses have been collected in the MCR through a legislated reporting system, since 1956. The MCR consistently attains the highest standing for cancer registries as assessed by the North American Association of Central Cancer Registries [15]. Manitoba Health is the single entity responsible for administrating health care in Manitoba, and prospectively maintains a number of administrative datasets, including the Drug Program Information Network (DPIN) and a physician claims database. Beginning in 1984, all citizens of Manitoba have been assigned a unique Personal Health Identification Number (PHIN), which allows for the linking of population-based datasets. DPIN is a point-of-sale electronic outpatient drug dispensation database that has been in place since 1995. DPIN tracks all relevant prescription information, including patient demographics, medication name, date of dispensation, and dose and quantity of medication. The physician claims database captures all unique physician interactions that result in a billing event, collected at the time a physician submits for fee-for-service payment. To protect patient confidentiality, the linkage in this study was performed, via scrambled PHINs, using anonymized versions of the above databases.
Study Population
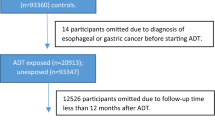
Using a retrospective cohort study design, we identified all patients with lung cancer from January 1, 2004 to December 31, 2010, using population-based datasets from the MCR. Information extracted included age, sex, histological subtype, stage at diagnosis, date of diagnosis, and date of death. Data regarding smoking history, asbestos exposure, and previous occupation were not available.
Data from the Manitoba Health administrative databases from January 1, 2004 to December 21, 2010 were used to determine exposure. APM was defined as exposure to antiandrogens, 5-alpha reductase inhibitors, GnRH agonists, or bilateral orchiectomy. DPIN was used to determine prescriptions filled for these medications as a measure of exposure to these medications. A significant exposure was defined as having filled two or more prescriptions for a medication in one of the above classes. Physician claims data was used to determine if the patient received bilateral orchiectomy at any time since 1984.
Statistical Analysis
Exposure to APM was categorized into mutually exclusive groups of no exposure, before, after, and both before and after diagnosis with lung cancer using a time-varying exposure model. Stage was separated into stages I, II, III, IV, and unknown/missing. Histological subtypes were categorized as adenocarcinoma, non-adenocarcinoma, and small cell lung cancer.
Tables of demographics and exposure were constructed. Univariate Cox regression was used to determine the impact of age, cancer stage, histology, history of prostate cancer, and the timing of APM on survival. A multivariable Cox model with time-varying covariates was constructed to evaluate for independent effects of APM exposure, age, stage, histology, and history of prostate cancer on survival. These variables were considered clinically important to keep in the model regardless of univariate/stepwise significance during model construction. Death from any cause was used in the analysis. Sensitivity analyses were performed on histology and type of APM exposure. An interaction term was added to assess the association between exposure time and outcome. Additional sensitivity analyses were constructed to address the potential for immortal time bias. This included a landmark analysis, using a landmark time of 6 month. An immediate time-varying model was constructed with the current user group defined as those with a 60-day supply of drug without a 30-day interruption. Former users were defined as those with a 30-day interruption, taking into account prescription refills. Non-users were defined as either having no record of a 60-day drug supply per DPIN, or being a former user for 1 year.
Results
A total of 3018 men with lung cancer were identified between 2004 and 2010 (Table 1). The most common histological subtype was non-adenocarcinoma NSCLC, and the majority of patients identified had stage IV disease. Those exposed to APM after their diagnosis of lung cancer had a greater proportion of stage I and II disease (60 %) compared to those exposed before diagnosis (16.7 %) or those never exposed (22.3 %). Patients exposed to APM both before and after their disease had a high proportion of stage I and II disease, but more closely resembled the distribution seen in patients with exposure before diagnosis, or no exposure (31.3 %). In addition, those exposed after, or before and after diagnosis, had a high proportion of adenocarcinoma histology (40.0 and 39.1 %, respectively). The proportion of adenocarcinoma was lower in those exposed either before diagnosis or never exposed (25.3 and 27.1 %, respectively). Two hundred and five (6.8 %) patients also had a history of prostate cancer. Of these, 113 patients were exposed to APM. There were a number of non-prostate cancer malignancies present in the lung cancer cohort, the most common being non-melanoma skin cancer (N = 390), colorectal and anal cancers (N = 99), bladder cancer (N = 62), kidney cancer (N = 38), and non-Hodgkin’s lymphoma (N = 32).
Of those patients included in the cohort, 339 (11.2 %) were identified as having exposure to some form of APM. The most common APM prescription was for the 5-alpha reductase inhibitor finasteride (Table 2). Bicalutamide was the most common antiandrogen prescribed. Among the patients on GnRH agonists, goserelin and leuprolide were the most frequently prescribed. Two hundred and fifty six patients were exposed to either antiandrogens or 5-alpha reductase inhibitors alone, 5 were exposed to GnRH agonists alone, and 60 were exposed to a combination of an anti-androgen and a GnRH agonist. Bilateral orchiectomy had occurred in 18 men (5.3 %).
Univariable analysis demonstrated that poor survival was associated with both increased age and stage at diagnosis. Patients with adenocarcinoma had better survival than those with non-adenocarcinoma (HR 0.64, p < 0.0001); conversely, patients with small cell lung cancer (SCLC) had poorer survival (HR 1.19, p = 0.009). There was no difference in survival in patients with a previous diagnosis of prostate cancer compared with those who did not (HR 1.06, p = 0.47). Significantly better survival was seen in patients with lung cancer exposed to APM compared to those with no exposure (Fig. 1). A statistically significant difference in survival was only seen when patients were exposed to APM either after (HR 0.37, p = 0.0007) or before and after their diagnosis of lung cancer (HR 0.60, p < 0.0001).
Kaplan-Meier estimates and the log-rank test were used to compare overall survival in patients with both lung cancer and prostate cancer who had exposure to APM versus no exposure. There was no statistically significant difference in survival between these two groups (p = 0.23).
In the multivariable analysis, patients with a diagnosis of lung cancer exposed to APM prior to their diagnosis demonstrated no statistically significant difference in survival compared to those who did not (HR 0.97, p = 0.69) (Table 3). A significantly greater survival was seen in patients exposed to APM after their diagnosis (HR 0.36, p = 0.0007) or both before and after their diagnosis (HR 0.53, p < 0.0001). To account for the difference in stage distribution between exposure groups, the analysis was stratified for stage (Fig. 2). A statistically significant difference was seen in early stage disease having been exposed to APM after diagnosis (HR 0.28, p = 0.03). In those exposed before and after, the difference in survival did not meet statistical significance (HR 0.48, p = 0.06). In late stage disease, a statistically significant difference in survival was seen in those exposed to APM after diagnosis (HR 0.41, p = 0.02) as well as before and after diagnosis (HR 0.54 p < 0.0001). When the impact of time after exposure was analyzed, it was found that the impact of androgen exposure diminished with each year (HR 1.39, p < 0.0001) (Table 3). This was consistent in both early and late stage groups (Table 3).
A sensitivity analysis was performed to estimate the effect by histology. In adenocarcinoma, significantly greater survival was seen when exposure to APM occurred both before and after diagnosis (HR 0.53, p = 0.02), or only after diagnosis (HR 0.29, p = 0.02). Patients with non-adenocarcinoma histology had a significantly greater survival when exposure occurred both before and after diagnosis (HR 0.62, p = 0.004), but this association with survival was not statistically significant for those exposed after the diagnosis (HR 0.51, 0.06). As SCLC histology was not associated with a different survival than non-adenocarcinoma, it was excluded from this sensitivity analysis.
Sensitivity analysis was also performed with type of APM. The association of APM exposure and survival was maintained in males exposed to 5-alpha reductase inhibitors and androgen receptor blockers (before: HR 1.13, p = 0.18; after: HR 0.29, p = 0.001; before and after: HR 0.53, p < 0.0001). Too few observations were present to evaluate other types of APM individually.
Using a landmark time of 9 months, the landmark analysis demonstrated a trend towards improved survival with APM exposure, but this was not significant (HR 0.79, p = 0.20) (Table 4). Similarly, the immediate time-varying model demonstrated a non-significant trend towards improved survival in those previously exposed to APM (HR 0.60, p = 0.16) (Table 4). Those on APM at the time of analysis did not demonstrate any difference in survival compared to those with no exposure (HR 1.00, p = 0.98).
Data on cause of death was also analyzed. Of those not exposed to APM, 1837 (81.8 %) died from lung cancer. In patients exposed to APM, 213 (79.8 %) died from lung cancer, while only 13 (4.9 %) died from prostate cancer. Other causes of death, including ischemic heart disease and COPD, were considerably less frequent.
Discussion
Male patients with lung cancer in Manitoba who were exposed to APM either after or both before and after the diagnosis of lung cancer had better overall survival compared with those who had no exposure, or were only exposed before diagnosis. Greater survival in the setting of APM exposure was independent of age, stage, and histology. To our knowledge, this is the first study to demonstrate an association between APM and greater survival in a lung cancer population. While lung cancer is not thought of as a hormone-sensitive malignancy, there is mounting evidence that sex hormones may play a role in its pathophysiology and patient outcome.
There are several potential mechanisms by which androgens could alter the pathophysiology of lung cancer. The androgen receptor is present in both NSCLC and SCLC tissue [5–7]. Exposure to androgens alters gene expression profiles in human NSCLC lines, including those related to cell growth and apoptosis [8]. Suppression of the androgen pathway may therefore have a direct effect on lung cancer cell proliferation, cell survival, or sensitivity to chemotherapy. There is evidence of cross-talk between AR and the epidermal growth factor receptor (EGFR), which is known to play a role in lung cancer pathogenesis [16]. Stimulation of either receptor using DHT or epidermal growth factor (EGF) can lead to activation of the p38MAPK-mTOR transduction pathway, which results in cell proliferation [16]. In addition, selective inhibitors of AR and EGFR cause a cessation of cell proliferation previously induced by DHT or EGF [16]. The importance of EGFR in lung cancer has been well established, and the use of EGFR tyrosine kinase inhibitors improves progression-free survival in advanced adenocarcinoma of the lung in which an EGFR gene mutation is identified [17, 18].
It is important to note that the majority of patients exposed to APM received a 5-alpha reductase inhibitor, either finasteride or dutasteride. Three isoenzymes of 5-alpha reductase exist: types 1, 2, and 3. Finasteride inhibits type 2 and 3 5-alpha reductase, while dutasteride inhibits all three isoenzymes [19]. 5-alpha reductase is expressed fairly ubiquitously throughout human tissues in adulthood, and the expression varies depending on the isoenzyme [19]. 5-alpha reductase type 3 has been identified in both benign and malignant lung tissue, and has been demonstrated to be overexpressed in lung adenocarcinoma tissue [20]. While the exact role of 5-alpha reductase type 3 in lung tissue is unclear, this suggests a mechanism by which 5-alpha reductase inhibitors could exert a protective effect.
It remains possible that the potential effect of APM on survival may not be related to a lung cancer-specific pathway. Males have a shorter life expectancy compared to females at baseline [21], and are known to have an increased risk of death from cardiovascular disease [22]. Alteration of the hormonal environment may offer protective effects related to alternate disease processes. This explanation is less likely as finasteride given preventatively to men at increased risk of prostate cancer has had no impact in survival in previous studies [23].
Although visually there appeared to be a greater survival difference in survival in patients with early stage disease compared to late stage disease (Fig. 2), the hazard ratios calculated in the multivariable analysis were similar, suggesting that any true difference may be small. The idea that patients with early stage disease may derive benefit from APM does have biological basis, however, as there is data suggesting that the androgen receptor could play a role in metastasis via modulation of cell migration in hepatocellular carcinoma [24]. As many patients with early stage disease will be candidates for resection, further study would be required to determine if APM use in the neoadjuvant or adjuvant setting would improve survival. The potential use of androgen pathway blockade in late stage disease is also an important consideration as the medications studied here have a mild side effect profile compared to current options for palliative chemotherapy.
There are several potential reasons why no difference in survival was seen in patients exposed to APM before the diagnosis of lung cancer. It is possible that if APM does have a protective effect in lung cancer patients, the effect is only significant when tumor growth is already underway. It is also possible that any protective effect of APM may be lost as soon as treatment is discontinued. Consideration must be given to the underlying differences in histology and stage between the exposed before diagnosis group and the exposed after diagnosis group, as the underlying characteristics of each group were not completely balanced.
This study is retrospective in design and therefore causation cannot be inferred from these results. We used a population-based dataset to maximize the power of the associations and eliminate the influence of referral bias in our inclusion criteria. The use of the DPIN and the CancerCare Manitoba database also provides a reliable means of capturing prescription data for the population. Selection bias for treatment with APM is a potential confounder in this study, and there were differences in the baseline characteristics of the three exposure groups. Importantly, the distribution of stage was skewed towards early stage disease in those exposed before and after diagnosis, which could clearly lead to better survival in this groups. Similarly, a greater proportion of patients in the exposed before diagnosis group and those never exposed to APM had non-adenocarcinoma histology. This is also a potential confounder as patients with non-adenocarcinoma histology had poorer survival. Several steps were undertaken to account for these underlying differences. A multivariable Cox regression analysis was used to analyze the data and provide a measure of overall effect. We then stratified this analysis into early stage and late stage groups to remove the potential confounding effect of stage. This did not qualitatively change the results as a statistically significant difference was still found in both the early stage group and the late stage group. Finally, multivariable sensitivity analysis on histology demonstrated the same qualitative effects of APM on survival. Pre-existing selection bias is an inherent limitation of retrospective cohort designs, and further prospective analysis with randomization to different exposure groups is required to completely eliminate this potential source of bias.
A proportion of patients with lung cancer also had a diagnosis of a second malignancy. It is possible that the second malignancy could have impacted the performance status and treatment of the lung cancer patients. There is minimal interaction between the standard treatments of lung cancer and the most common second malignancies identified (prostate, colorectal, renal, lymphoma); therefore, we feel it is unlikely that these diagnoses would have influenced the selection of lung cancer treatment. Also, lung cancer was the cause of death for approximately 80 % of patients in this study regardless of exposure to APM; therefore, it is unlikely that alternate malignancies had a significant impact on the survival analysis.
The issue of immortal time bias (ITB) [25] was addressed by using a multivariable Cox model with time-varying covariates for the primary analysis. This was selected as a primary analysis because the effect of APM on cancer pathogenesis is likely to take time, in which case, maintaining consistent exposure groups is important. As an additional sensitivity analysis, a landmark analysis as well as an immediate time-varying model were used. While the landmark analysis demonstrated a trend towards longer survival, this was not significant. This may be related to the loss of statistical power inherent to a conditional landmark analysis; however, it is possible this represents a more accurate method of accounting for ITB and suggests a smaller or null effect. The immediate time-varying model demonstrated a non-significant trend towards greater survival, but only in former users of APM. This model may be a better representation of the more immediate on/off effects of APM, and the lack of a significant association supports the theory that APM exposure has an impact on cancer pathogenesis and growth over a longer period of time.
Conclusion
Exposure to APM after a diagnosis of lung cancer is associated with longer survival in male patients. This study provides further evidence that sex hormones may play a role in lung cancer pathophysiology, and that androgens in particular may have a greater role than previously thought. Our results generate new hypotheses to be tested, such as determining the potential mechanism of this effect and determining the clinical utility of the AR as a biomarker. While androgen receptor expression has not been linked to prognosis [10], it may help identify a subgroup of patients who would derive benefit from APM. Further supporting evidence of a protective effect of APM in lung cancer could potentially support a randomized controlled trial of APM in a select group of lung cancer patients. Validation of the data in a larger population and exploration of tissue bank data for an association between AR expression and outcomes with APM treatment may improve our understanding of androgens in lung cancer, but ultimately randomized trials would be necessary to assess the therapeutic effects of these agents. As we move towards individualized therapy in oncology, the utilization of APM in specific lung cancer populations has the potential to be a simple, widely available, and cost-effective treatment for this disease.
References
Canadian Cancer Society’s Advisory Committee on Cancer Statistics (2014) Canadian cancer statistics 2014. Canadian Cancer Society, Toronto
Fu JB, Kau TY, Severson RK, Kalemkerian GP (2005) Lung cancer in women: analysis of the national surveillance, epidemiology, and end results database. Chest 127(3):768–777
Rivera MP (2009) Lung cancer in women: the differences in epidemiology, biology and treatment outcomes. Expert Rev Respir Med 3(6):627–634
Pitz MW, Musto G, Navaratnam S (2013) Sex as an independent prognostic factor in a population-based non-small cell lung cancer cohort. Can Respir J 20(1):30–34
Beattie CW, Hansen NW, Thomas PA (1985) Steroid receptors in human lung cancer. Cancer Res 45(9):4206–4214
Kaiser U, Hofmann J, Schilli M, Wegmann B, Klotz U, Wedel S et al (1996) Steroid-hormone receptors in cell lines and tumor biopsies of human lung cancer. Int J Cancer 67(3):357–364
Maasberg M, Rotsch M, Jaques G, Enderle-Schmidt U, Weehle R, Havemann K (1989) Androgen receptors, androgen-dependent proliferation, and 5 alpha-reductase activity of small-cell lung cancer cell lines. Int J Cancer 43(4):685–691
Mikkonen L, Pihlajamaa P, Sahu B, Zhang FP, Jänne OA (2010) Androgen receptor and androgen-dependent gene expression in lung. Mol Cell Endocrinol 317(1–2):14–24
Jeong Y, Xie Y, Lee W, Bookout AL, Girard L, Raso G et al (2012) Research resource: diagnostic and therapeutic potential of nuclear receptor expression in lung cancer. Mol Endocrinol 26(8):1443–1454
Rades D, Setter C, Dahl O, Schild SE, Noack F (2012) The prognostic impact of tumor cell expression of estrogen receptor-α, progesterone receptor, and androgen receptor in patients irradiated for nonsmall cell lung cancer. Cancer 118(1):157–163
Nishio M, Ohyanagi F, Horiike A, Ishikawa Y, Satoh Y, Okumura S et al (2005) Gefitinib treatment affects androgen levels in non-small-cell lung cancer patients. Br J Cancer 92(10):1877–1880
Foley CL, Kirby RS (2003) 5 alpha-reductase inhibitors: what's new? Curr Opin Urol 13(1):31–37
Mahler C, Verhelst J, Denis L (1998) Clinical pharmacokinetics of the antiandrogens and their efficacy in prostate cancer. Clin Pharmacokinet 34(5):405–417
Moreau JP, Delavault P, Blumberg J (2006) Luteinizing hormone-releasing hormone agonists in the treatment of prostate cancer: a review of their discovery, development, and place in therapy. Clin Ther 28(10):1485–1508
Chen VW, Wu XC (1999) Incidence, cancer in North America, 1991–1995. North American Association of Central Cancer Registries
Recchia AG, Musti AM, Lanzino M, Panno ML, Turano E, Zumpano R et al (2009) A cross-talk between the androgen receptor and the epidermal growth factor receptor leads to p38mapk-dependent activation of mtor and cyclind1 expression in prostate and lung cancer cells. Int J Biochem Cell Biol 41(3):603–614
Rosell R, Carcereny E, Gervais R, Vergnenegre A, Massuti B, Felip E et al (2012) Erlotinib versus standard chemotherapy as first-line treatment for european patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol 13(3):239–246
Mok TS, Wu YL, Thongprasert S, Yang CH, Chu DT, Saijo N et al (2009) Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med 361(10):947–957
Azzouni F, Godoy A, Li Y, Mohler J (2012) The 5 alpha-reductase isozyme family: a review of basic biology and their role in human diseases. Adv Urol 2012:530121
Godoy A, Kawinski E, Li Y, Oka D, Alexiev B, Azzouni F et al (2011) 5Α-Reductase type 3 expression in human benign and malignant tissues: a comparative analysis during prostate cancer progression. Prostate 71(10):1033–1046
Statistics Canada (2012) Life expectancy at birth, by sex, by province (table). “Statistics Canada, Canadian Vital Statistics, Birth and Death Databases and population estimates.” CANSIM. Statistics Canada catalogue no. 84-537-XIE. Ottawa, Ontario. Last updated May 31 2012. http://www.statcan.gc.ca/tables-tableaux/sum-som/l01/cst01/health26-eng.htm. Accessed 24 Aug 2014)
Lloyd-Jones DM, Larson MG, Beiser A, Levy D (1999) Lifetime risk of developing coronary heart disease. Lancet 353(9147):89–92
Thompson IM, Goodman PJ, Tangen CM, Parnes HL, Minasian LM, Godley PA et al (2013) Long-term survival of participants in the prostate cancer prevention trial. N Engl J Med 369(7):603–610
Ma WL, Hsu CL, Yeh CC, Wu MH, Huang CK, Jeng LB et al (2012) Hepatic androgen receptor suppresses hepatocellular carcinoma metastasis through modulation of cell migration and anoikis. Hepatology 56(1):176–185
Giobbie-Hurder A, Gelber RD, Regan MM (2013) Challenges of guarantee-time bias. J Clin Oncol 31(23):2963–2969
Acknowledgments
The authors would like to thank Dr. Salah Mahmud for his advice on the analysis. The results and conclusions are those of the authors, and no official endorsement by Manitoba Health is intended or should be inferred
Conflict of Interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Harlos, C., Musto, G., Lambert, P. et al. Androgen Pathway Manipulation and Survival in Patients with Lung Cancer. HORM CANC 6, 120–127 (2015). https://doi.org/10.1007/s12672-015-0218-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12672-015-0218-1