Abstract
Purpose
To determine if a non-exercise algorithm-derived assessment of cardiorespiratory fitness (CRFA) accurately predicted estimated values obtained using a six-minute walk test (CRF6MWD) and the Duke Activity Status Index (CRFDASI).
Methods
Following research ethics board approval, an observational cohort study was conducted in selected, consenting patients undergoing elective surgery. Participants completed questionnaires assessing their self-reported exercise capacity. Their height, weight, waist circumference, and vital signs were measured. A six-minute walk test was performed twice with a 45-min rest interval between tests. The correlation between CRFA and both CRF6MWD and CRFDASI was determined.
Results
Two hundred forty-two participants were included. Mean age was 62 (range 45-88 yr); 150 (62%) were male, 87 (36%) self-reported walking or jogging > 16 km per week, and 49 (20%) were current smokers. The CRFA and CRF6MWD were highly correlated (Pearson r = 0.878; P < 0.001). CRFA and CRFDASI were less strongly correlated (Pearson r = 0.252; P < 0.001). Among patients capable of walking > 427 m in the six-minute walk test, CRFA, CRF6MWD, and CRFDASI were equivalent.
Conclusion
A non-exercise algorithm can estimate cardiorespiratory fitness in patients presenting for elective surgery. The variables required to compute CRFA can be obtained in a clinic setting without the need to engage in formal exercise testing. Further evaluation of CRFA as a predictor of long-term outcome in patients is warranted.
Résumé
Objectif
Nous avons tenté de déterminer si une évaluation de la capacité cardiorespiratoire (CRFA) non fondée sur l’exercice mais dérivée d’un algorithme permettrait de prédire de façon précise les valeurs estimées obtenues dans le cadre d’un test de marche de six minutes (CRF6MM) et du test de DASI (Duke Activity Status Index (CRFDASI)).
Méthode
Après avoir obtenu le consentement du Comité d’éthique de la recherche, une étude de cohorte observationnelle a été réalisée auprès de patients préalablement choisis et ayant donné leur consentement, qui devaient subir une chirurgie non urgente. Les participants ont répondu à des questionnaires évaluant leur capacité d’effort selon leur propre appréciation; leur taille, poids, tour de taille et signes vitaux ont été mesurés. Un test de marche de six minutes a été réalisé à deux reprises, avec un intervalle de repos de 45 minutes entre les deux phases du test.
Résultats
Deux cent quarante-deux participants ont pris part à l’étude. L’âge moyen était de 62 ans (45-88 ans); 150 (62 %) participants étaient des hommes, 87 (36 %) ont rapporté marcher ou courir > 16 km par semaine, et 49 (20 %) étaient actuellement fumeurs. La CRFA et la CRF6MM étaient très corrélées (coefficient de Pearson r 0,878, P < 0,001); la CRFA et la CRFDASI étaient moins corrélées (coefficient de Pearson r 0,252, P < 0,001). Parmi les patients capables de marcher > 427 m au cours du test de marche de 6 minutes, la CRFA, CRF6MM et la CRFDASI étaient équivalentes.
Conclusion
Un algorithme non fondé sur l’exercice peut estimer la capacité cardiorespiratoire des patients se présentant pour une chirurgie non urgente. Les variables nécessaires à calculer la CRFA peuvent être obtenues dans un contexte clinique sans devoir tester l’exercice de façon formelle. Une évaluation approfondie de la CRFA en tant que prédicteur des pronostics à long terme des patients serait nécessaire.
Similar content being viewed by others
In the evaluation of patients presenting for elective surgery, assessment of functional status assists in estimating perioperative risk and establishing the need for further testing before surgery.1 Usually, functional status is determined by inquiring about the patient’s capacity to perform routine activities of daily living or, more specifically, their ability to “climb a flight of stairs”. The inability to perform the latter is closely correlated with an increase in perioperative complications2 and is equated with an exercise capacity of < 4 metabolic equivalent of task (MET) - i.e., the metabolic rate while sitting quietly in a chair where 1 MET is approx. 3.5 mL O2·kg−1·min−1.3 The reliability of this form of assessment has recently been called into question, and emphasis is being placed on the need for more accurate estimates of exercise capacity.4
The gold standard for assessing cardiorespiratory fitness (CRF) is the cardiopulmonary exercise test (CPET) which assesses maximum oxygen consumption (VO2max) and the anerobic threshold. Hill and Lupton5 defined VO2max as “the oxygen intake during an exercise intensity at which actual oxygen intake reaches a maximum beyond which no increase in effort can raise it.” Anerobic threshold is defined as “the level of work or O2 consumption just below that at which metabolic acidosis and the associated changes in gas exchange occur.”6 Studies have shown that the CPET accurately predicts the risk of postoperative cardiorespiratory events in surgical patients.7,8 A systematic review concluded that VO2max, as determined by a CPET, is a predictor of perioperative morbidly and mortality in a non-cardiopulmonary surgical population.9 Unfortunately, CPET is impractical to perform in routine practice.
The six-minute walk test (6MWT) is a less resource-intensive method of estimating CRF.10,11 It assesses the submaximum level of functional activity, is reflective of a patient’s capacity to perform daily activities, has been validated in several populations, and is predictive of adverse outcomes following surgery. The 6MWT is considered a useful test in risk stratification of elective surgical patients. Distances walked > 563 m during the 6MWT indicate that a CPET is not necessary, whereas a walk distance of < 427 m indicates that a patient is at high preoperative risk and should undergo further evaluation.12 Nevertheless, the 6MWT requires personnel to supervise and monitor the patient during the performance of the test. It takes time to perform and, consequently, is not widely used in preoperative assessment.
A non-exercise algorithm using routinely available clinical variables (height, weight, waist circumference, resting heart rate, smoking status, and self-reported fitness level) provides MET values that are closely correlated with treadmill testing data in healthy individuals.13 We postulated that using a non-exercise algorithm to determine CRF preoperatively might prove to be a more accurate and feasible option in terms of time, resources, and patient burden.
This study used a consecutive sample of selected elective surgical patients to estimate and compare CRF obtained by means of 1) a non-exercise algorithm developed by Jackson et al.,14 2) data derived from two 6MWTs performed in accordance with the guidelines developed by the American Thoracic Society,15 and 3) the Duke Activity Status Index (DASI).16 We hypothesized that, in a population of patients awaiting elective non-cardiac surgery, CRF estimated using the non-exercise algorithm (CRFA) would accurately predict CRF values objectively determined from the distance walked on the 6MWT (CRF6MWD) and those self-reported using the widely known DASI (CRFDASI).
Methods
Participants
The study was approved by the Ethics Review Board at the University of Alberta on 2014-12-17. Recruitment occurred from May to September 2015. Patients undergoing major elective surgery (see Table 1) were pre-screened, approached, and enrolled during their appointment at the pre-admission clinic (PAC) at the University of Alberta and the Royal Alexandra hospitals in Edmonton, AB, Canada. All patients were considered for inclusion unless they were American Society of Anesthesiologists class I or II or < 45 yr of age. This approach was taken in an attempt to include patients across a spectrum of CRF, not just healthy young individuals. Exclusion criteria were patients with uncontrolled hypertension (> 180/110 mmHg), unstable angina, history of a recent heart attack in the last month, or a resting heart rate > 120 beats·min−1. Patients who were taking beta-blocker medication, scheduled to be admitted to an intensive care unit postoperatively, or unable to provide written and informed consent were also excluded from the study. In addition, patients with physical limitations affecting their ability to perform the 6MWT were excluded. Patients gave their informed written consent prior to enrolment and data collection. Two trained medical students took the measurements, collected data, and monitored 6MWT performance.
Procedures
Before performing the 6MWT, participants provided data on their demographics, smoking status (smoker, non-smoker, ex-smoker), medical history, medications, and physical activity level by self-reporting their level of physical activity in the past 30 days (walked or jogged less or more than 16 km·wk−1). They also completed the DASI questionnaire.
Patients’ height and weight were taken with a medical grade scale and stadiometer, and their waist circumference was measured at the midpoint between the iliac crest and the bottom of the rib cage in accordance with World Health Organization recommendations.17 After patients rested for five minutes, their vital signs (blood pressure, heart rate, O2 saturation) were recorded. Respiration rate was recorded over 15 sec and adjusted to the number of breaths per minute. Patients were to abstain from alcohol, caffeine, and nicotine for at least 30 min prior to measurement.18
The 6MWT was performed according to the American Thoracic Society guidelines.15 The test was performed twice with at least a 45-min rest between the first and second tests. Patients were instructed to walk laps around a track to achieve the farthest distance possible within six minutes. The track consisted of two orange cones placed 30 m apart in a level hallway marked at 3-m intervals. Patients proceeded 30 m, turned 180° around a cone, and continued back to their initial position to complete 60 m per lap. Before and after the exercise, patients were asked to rate their shortness of breath and perceived exertion using the 6-20 Borg scale,15 where 6 = no exertion at all, and 20 = maximum exertion. The distance walked in both tests was recorded to the nearest metre completed, and the test with the greatest distance was used in our analysis.
The CRF values, expressed in METS, were estimated for the non-exercise algorithm (CRFA),14,19 the distance on the 6MWT (CRF6MWD),20 and the DASI (CRFDASI)16 using the following formulae. VO2max values were converted to METS by dividing by 3.5, where appropriate:



where age = age (yr); BMI = body mass index (kg·m−2); WC = waist circumference (cm); RHR = resting heart rate (beats·min−1); PAI = physical activity index as assessed by self-reporting of walking >16 km·week−1 (0 inactive, 1 active); CS = currently smoke (0 no, 1 yes). 6MWD = six-minute walk test distance (m); sex = (male = 0, female = 1).
Statistical analysis
Our sample size was calculated to assess surgical short-term outcomes and the impact on quality of life at six months following the initial test (not reported in this manuscript). According to Burr et al.,20 the mean (standard deviation [SD]) aerobic demand of the 6MWT for healthy adults is 28.7 (5.7) mL·kg−1·min−1 (MET value = 8.2). To test our hypothesis, the power was set at 0.80, and an alpha of P < 0.05 was used. A sample size of 201 patients was calculated as required for a one-sample non-inferiority test with the true mean (SD) MET value of 8.2 (1.6) and the equivalence margin of 0.3. Accounting for a 30% attrition rate at the six-month follow-up - according to a recently published study in Canadian surgical patients21 - a sample size of 261 was determined.
Two variables had a single missing value, which were imputed using the median of all entries for the variable.
Continuous variables were reported using mean (SD) and compared using Student’s t test and analysis of variance. Categorical variables were presented using frequency and percentages and compared using the Chi square test. Bivariate correlation analysis was performed, and linear regression analysis models were used to investigate the correlation between CRFA, CRF6MWD, and CRFDASI.
Results
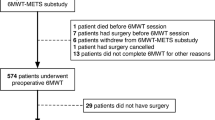
Six of the 266 recruited participants withdrew their consent and an additional 18 were excluded from analyses. Two patients refused to provide a waist circumference measurement; one was using a beta blocker; one had a pacemaker; nine showed physical limitations that prevented appropriate performance of the 6MWT; three did not follow the instructions when performing the 6MWT; and two were identified outliers for their high 6MWT distance (Fig. 1). Of the remaining 242 participants (mean age 62 yr, range 45-88 yr) included in the analysis, 150 (62%) were male, 87 (36%) self-reported being physically active, and 49 (20%) were current smokers. No significant difference was found between the two hospital groups. Table 1 shows the baseline characteristics and measures of cardiorespiratory fitness of our participants stratified by sex. There were no adverse events during the 6MWT. Borg scale data in both tests showed that < 5% of our participants reported somewhat severe to severe shortness of breath or fatigue post-test (Table 2). Patients who self-reported walking or jogging > 16 km·wk−1 walked farther on the 6MWT than less-active patients [540 (69) m vs 519 (71) m; Student’s t = 2.3; P = 0.03].
The CRFA and CRF6MWD were highly correlated (Pearson r = 0.878; P < 0.001, Fig. 2a); CRFA and CRFDASI were less strongly correlated (Pearson r = 0.252; P < 0.001, Fig. 2b). These correlations remained when stratified by sex and level of physical activity. A comparison of CRFA and the unadjusted distance walked during the 6MWT is also presented (Pearson r = 0.420; P < 0.001, Fig. 2C).
Correlation of CRFA with (a) CRF6MWD, (b) CRFDASI, and (c) 6MWD. CRF = cardiorespiratory fitness; CRFA = CRF derived from the non-exercise algorithm (METS); CRF6MWD = CRF derived from the distance walked on the six-minute walk test (METS); CRFDASI = CRF derived from Duke Activity Status Index (METS); 6MWD = distance walked on the six-minute walk test (m)
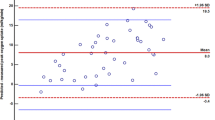
Paired-sample Student’s t test showed no significant difference between CRF6MWD and CRFA in patients who walked < 427 m (Student’s t = 1.61; P = 0.13) or walked 427-563 m (Student’s t = 1.22; P = 0.23). Nevertheless, this difference was statistically significant between CRF6MWD and CRFDASI for both groups (Student’s t = 4.2; P = 0.001 and Student’s t = 4.8; P < 0.001, respectively). For patients who walked > 563 m, no significant difference was seen for any of the estimations (Table 3). Fig. 3 graphically shows that the CRFA is equivalent to the measured CRF6MWD in patients capable of walking > 427 m.
Differences between CRFA, CRF6MWD, and CRFDASI using 6MWD cut points. CRFA = CRF derived from the non-exercise algorithm (METS); CRF6MWD = CRF derived from the distance walked on the 6 minute walk test (METS); CRFDASI = CRF derived from Duke Activity Status Index (METS); 6MWD = distance walked on the six-minute walk test (m)
Discussion
In this observational study involving a cohort of surgical patients, < 40% of participants self-reported being physically active. Study results showed a strong correlation between CRFA and CRF6MWD and a weak correlation with CRFDASI. The mean CRFA was significantly lower for patients who walked < 563 m than those who walked > 563 m. To predict CRF in this study, we used a non-exercise algorithm developed from longitudinal rather than cross-sectional data and one that accounts for the nonlinear decline in CRF that occurs with advancing age. This algorithm has been shown to predict the future risk of non-fatal cardiovascular events and related mortality in a large cohort of more than 34,000 males and 9,000 females after adjusting for the appropriate risk factors.19 Unlike the cohort initially used to determine the non-exercise algorithm - which was predominantly white, well-educated, and essentially healthy individuals participating in a preventive health program in Texas - our sample consisted of a wide spectrum of patients aged over 45 yr and attending preoperative assessment clinics at two tertiary care hospitals. All were covered by a provincially funded universal health care system and came from diverse social backgrounds. Our study population was older and had coexisting health issues, including cancer, diabetes, and cardiovascular disease.
We compared the estimated CRFA using the CRF6MWD derived from an analysis of the 6MWT data - obtained on two occasions 45 min apart at the time of a PAC visit. The 6MWT is considered a reasonable alternative to the CPET approach, particularly when modified by anthropometric and demographic variables.20,22 The importance of including these variables in the estimation of CRF by the 6MWT is underscored by our finding that the distance walked according to the 6MWT or 6MWT data modified by standard constants23,24 correlated poorly with CRFA in our patient population. We found an excellent correlation between the estimated CRFA and the CRF6MWD, both of which adjust for anthropomorphic and demographic variables, suggesting that both equations could be used to estimate the CRF. Using the CRFA may well obviate the need to perform a 6MWT. However, we excluded patients who were being treated with beta blocking drugs as the CRFA includes the resting heart rate as one of the parameters of the algorithm. In consequence, only ~11% of the study group had a history of heart disease. The utility of CRFA in populations with a greater prevalence of heart disease remains unknown.
In our comparison of estimated MET values using the CRFA, CRF6MWD, and CRFDASI, we compared across cut points similar to those described by Sinclair et al. 12 These 6MWD values are of course arbitrary, but they seem reasonable for comparison purposes given the limited data on outcomes and CRF, in large part because of the practical difficulty of measuring the latter. Our data suggest that CRFDASI may overestimate CRF in those who have a lower 6MWD value. Also, our observations must be treated cautiously as we had few subjects (n = 19) in the < 427 6MWD cohort, and all of the compared MET values were estimated. Others who have focused on older patients with previously diagnosed cardiac and respiratory disease have found a reasonable relation between functional tests such as the incremental shuttle walk test and the DASI.25
The 6MWT distance achieved by our study group was less than that recently observed in a group of healthy Canadian individuals.24 Interestingly, positive answers to the question “In the past 30 days did you participate in some regular physical activity?” were associated with better CRF using all three measures studied (data not shown). Nevertheless, it may be valuable to include a question about participation in regular physical activity as part of routine preoperative assessment.
One study limitation was that we did not attempt to correlate the CRF - calculated by any of the three measures - with surgery outcomes, including cardiovascular outcomes. The population studied was not representative of all patients who require surgery, as the exclusion criteria eliminated the vast majority of patients with heart disease from participation. Our sample of patients who walked < 427 (19) m was relatively small, further limiting our ability to draw a firm conclusion about equivalency in this subset of patients with poor exercise capacity.
In conclusion, CRF can be relatively accurately estimated by a non-exercise algorithm in a defined subgroup of patients presenting for elective surgery. The variables required to obtain CRF in this fashion can be easily obtained in a clinical setting without the need to engage in exercise-related testing. Further evaluation of CRFA as a predictor of long-term postoperative outcome in patients is warranted.
References
Fleisher LA, Fleishmann KE, Uretsky BF, Wijeysundera DN. ACC/AHA Guideline on Perioperative Cardiovascular Evaluation and Management of Patients Undergoing Noncardiac Surgery. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2014; 64: e77-137.
Reilly CS. Can we accurately assess an individual’s perioperative risk? Br J Anaesth 2008; 101: 747-9.
Jette M, Sidney K, Blumchen G. Metabolic equivalents (METS) in exercise testing, exercise prescription, and evaluation of functional capacity. Clin Cardiol 1990; 13: 555-65.
Melon CC, Eshtiaghi P, Luksun WJ, Wijeysundera DN. Validated questionnaire vs physicians’ judgment to estimate preoperative exercise capacity. JAMA Intern Med 2014; 174: 1507-8.
Hill AV, Lupton H. Muscular exercise, lactic acid, and the supply and utilization of oxygen. Q J M 1923; 13: 135-71.
Wasserman K, Whipp BJ, Koyl SN, Beaver WL. Anaerobic threshold and respiratory gas exchange during exercise. J Appl Physiol 1973; 35: 236-43.
Snowden CP, Prentis J, Jacques B, et al. Cardiorespiratory fitness predicts mortality and hospital length of stay after major elective surgery in older people. Ann Surg 2013; 257: 999-1004.
Brunelli A, Belardinelli R, Refai M, et al. Peak oxygen consumption during cardiopulmonary exercise test improves risk stratification in candidates to major lung resection. Chest 2009; 135: 1260-7.
Smith TB, Stonell C, Purkayastha S, Paraskevas P. Cardiopulmonary exercise testing as a risk assessment method in non cardio-pulmonary surgery: a systematic review. Anaesthesia 2009; 64: 883-93.
Enright PL. The six-minute walk test. Respir Care 2003; 48: 783-5.
Tveter AT, Dagfinrud H, Moseng T, Holm I. Health-related physical fitness measures: reference values and reference equations for use in clinical practice. Arch Phys Med Rehabil 2014; 95: 1366-73.
Sinclair RC, Batterham AM, Davies S, Cawthorn L, Danjoux GR. Validity of the 6 min walk test in prediction of the anaerobic threshold before major non-cardiac surgery. Br J Anaesth 2012; 108: 30-5.
Jackson AS, Wier LT, Ross RM. The validity of non-exercise cardiorespiratory fitness prediction models. Med Sci Sports Exerc 1995; 27: 1096-8.
Jackson AS, Sui X, O’Connor DP, et al. Longitudinal cardiorespiratory fitness algorithms for clinical settings. Am J Prev Med 2012; 43: 512-9.
ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: Guidelines for the six-minute walk test. Am J Respir Crit Care Med 2002; 166: 111-7.
Hlatky MA, Boineau RE, Higginbotham MB, et al. A brief self-administered questionnaire to determine functional capacity (the Duke Activity Status Index). Am J Cardiol 1989; 64: 651-4.
Anonymous. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser 2000; 894: i-xii, 1-253.
Pickering TG, HallJE Appel LJ, et al. Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation 2005; 111: 697-716.
Artero EG, Jackson AS, Sui X, et al. Longitudinal algorithms to estimate cardiorespiratory fitness: associations with nonfatal cardiovascular disease and disease-specific mortality. J Am Coll Cardiol 2014; 63: 2289-96.
Burr JF, Bredin SS, Faktor MD, Warburton DE. The 6-minute walk test as a predictor of objectively measured aerobic fitness in healthy working-aged adults. Phys Sportsmed 2011; 39: 133-9.
Hoogerboord M, Wiebe S, Klassen D, Ransom T, Lawlor D, Ellsmere J. Laparoscopic sleeve gastrectomy: perioperative outcomes, weight loss and impact on type 2 diabetes mellitus over 2 years. Can J Surg 2014; 57: 101-5.
Mandic S, Walker R, Stevens E, et al. Estimating exercise capacity from walking tests in elderly individuals with stable coronary artery disease. Disabil Rehabil 2013; 35: 1853-8.
Ross RM, Murthy JN, Wollak ID, Jackson AS. The six minute walk test accurately estimates mean peak oxygen uptake. BMC Pulm Med 2010; 10: 31.
Hill K, Wickerson LM, Woon LJ, et al. The 6-min walk test: responses in healthy Canadians aged 45 to 85 years. Appl Physiol Nutr Metab 2011; 36: 643-9.
Struthers R, Erasmus P, Holmes K, Warman P, Collingwood A, Sneyd JR. Assessing fitness for surgery: a comparison of questionnaire, incremental shuttle walk, and cardiopulmonary exercise testing in general surgical patients. Br J Anaesth 2008; 101: 774-80.
Conflicts of interest
None declared.
Editorial responsibility
This submission was handled by Dr. Gregory L. Bryson, Deputy Editor-in-Chief, Canadian Journal of Anesthesia.
Author contributions
Fadi Hammal and Barry A. Finegan contributed substantially to all aspects of this manuscript, including conception and design; acquisition, analysis, and interpretation of data; and drafting the article. Tanis Quaife and Kieran Purich contributed substantially to the acquisition of data. Robert Haennel and Ferrante Gragasin contributed substantially to the conception and design of the manuscript. Daniella San Martin-Feeney contributed substantially to the conception and design of the manuscript and to the acquisition of data.
Funding
Internal sources.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hammal, F., Quaife, T., Purich, K. et al. Assessing the accuracy of algorithm-derived cardiorespiratory fitness in surgical patients: a prospective cohort study. Can J Anesth/J Can Anesth 64, 361–369 (2017). https://doi.org/10.1007/s12630-017-0812-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-017-0812-5