Abstract
Acute coronary syndrome (ACS) still remains one of the leading causes of mortality and morbidity worldwide. Seven to fifteen percent of patients presenting with ACS have unobstructed coronary artery disease (CAD) on urgent angiography. Patients with ACS and unobstructed coronary arteries represent a clinical dilemma and their diagnosis and management is quite variable in current practice. Cardiovascular magnetic resonance imaging with its unique non-invasive myocardial tissue characterization property has the potential to identify underlying etiologies and reach a final diagnosis. These include acute and chronic myocarditis, embolic/spontaneous recanalization myocardial infarction, and Tako-Tsubo cardiomyopathy, and other conditions. Establishing a final diagnosis has a direct implication on patient’s management and prognosis. In this article, we have reviewed the current evidence on the diagnostic role of cardiac magnetic resonance (CMR) in patients with ACS and unobstructed coronary arteries. We have also highlighted the potential role of CMR as a risk stratification or prognostication tool for this patient population.
Similar content being viewed by others
Introduction
Globally, acute coronary syndrome (ACS) still remains one of the leading causes of mortality and morbidity. Emergency or early angiography is recommended in suspected ACS with ST-elevation myocardial infarction (STEMI) or in non-ST elevation ACS (NSTE-ACS) with an intermediate-high Global Registry of Acute Coronary Events (GRACE) score. The literature suggests that 7–10 % of patients presenting with STEMI and 10–15 % of patients presenting with NSTE-ACS have unobstructed coronary artery disease (CAD) on urgent angiography [1–8]. Patients with ACS and unobstructed coronary arteries represent a clinical dilemma and their management is quite variable in current practice. Secondary prevention medications for ACS are used less frequently in these patients than in patients with obstructive CAD [9, 10]. This is partly due to our lack of understanding of the underlying patho-physiological mechanisms leading to the troponin rise and the lack of clear-cut guidelines. A common clinical misconception is that patients in this group have a relatively good prognosis in comparison with patients with an MI with obstructive CAD; several studies have shown that the mortality rate or re-infarction is not negligible following ACS with unobstructed CAD [8, 10–13, 14•]. A recent systematic review of patients presenting with suspected MI and unobstructed coronary arteries by Pasupathy et al. showed an overall all-cause mortality of 4.7 % at 12 months [15••]. Several recent studies have shown that additional imaging like cardiac magnetic resonance (CMR) may be particularly useful in determining the diagnosis. Accurate diagnosis helps to tailor medical treatment, for example the diagnosis of a non-ischemic underlying etiology may obviate the need for anti-platelet and anti-atherosclerotic therapies.
CMR in ACS and Unobstructed Coronaries
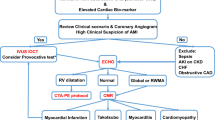
Three possible etiologies explain the clinical presentation in up to 95 % of cases of acute chest pain, elevated troponin, and unobstructed coronary arteries [16–18, 19••, 20•, 21••, 22•, 23•, 24•, 25•]. These include: (1) acute myocarditis, (2) acute MI, and (3) cardiomyopathy, in particular Tako-Tsubo cardiomyopathy (TCM). All of these conditions can be easily diagnosed with an appropriately tailored CMR study.
CMR diagnostic accuracy is based on the use of a number of different sequences, which includes—long- and short-axis cine, and T2-weighted and late gadolinium enhancement (LGE) imaging repeated in the same slice positions as the cine imaging. These three sequences assess the presence of regional wall motion abnormalities and ventricular volumes calculation, presence, and extent of myocardial edema/inflammation and myocardial scar/fibrosis, respectively.
First-pass perfusion and T1 and T2 mapping sequences can be added depending on the clinical question or the research interest (Table 1). This will result in a total scan duration time of ∼45 min. [26••]
All of the three acute pathologies (myocarditis, MI, or TCM) cause myocardial injury leading to edema. Edema in CMR corresponds to an increase in the T2 relaxation time which can be delineated with T2-weighted imaging [27]. There are various sequences available for delineation of myocardial edema. T2-weighted short-tau inversion recovery (T2-STIR) is the most commonly used sequence to image edema in clinical practice. However, T2-STIR image quality is easily degraded with respiratory motion or tachyarrhythmia, which are both common in patients with ACS and unobstructed coronaries (Fig. 1). Newer sequences such as ACUT2E (cardiac unified T2 edema) and T2 mapping are less prone to such artefacts. However, a recent study by McAlindon et al. demonstrated that the different methods for detecting and quantifying myocardial edema are not interchangeable, and that T2 mapping was the most reproducible method, albeit this sequence comparison was done just in the context of STEMI [28••].
Three CMR sequences have diagnostic role in patients suspected with myocarditis: (1) LGE sequences for detection of myocardial necrosis and/or fibrosis, (2) T2-weighted images for assessment of myocardial edema, and (3) T1-weighted sequences before and after contrast injection for detection of myocardial hyperemia (Fig. 2). Myocardial infarction can be diagnosed on CMR by identifying a subendocardial or transmural LGE pattern (Fig. 3) [29] whereas TCM can be diagnosed by the characteristic mid-apical myocardial edema with corresponding regional wall motion abnormalities and apical ballooning, but with no or only subtle LGE (Fig. 4).
Acute myocarditis in a 38-year male. Late gadolinium enhancement (LGE) sequence (white arrows) showing a patchy and diffuse epicardial LGE in the basal and mid-cavity lateral wall (a). T2−weighted images of same patient showing increased myocardial signal intensity (red arrows) of the basal and mid-cavity epicardial lateral wall (b) signifying myocardial edema
A 63-year-old man with small transmural myocardial infarction in the distal anterior and anterolateral walls. T2-weighted images showing small area of myocardial edema in the apical anterior and lateral walls, corresponding to the distal LAD territory (a). LGE images showing transmural infarction in the distal anterior and anterolateral walls (b)
Although a number of retrospective and prospective clinical studies have reported the diagnostic role of CMR in this patient cohort, the diagnostic pick-up rate is variable. This could be attributed to the time delay between CMR imaging from the acute presentation, as well as the CMR sequences and imaging protocol used.
Role of CMR in Diagnosis
Acute Myocarditis
Several studies have shown that the commonest underlying etiology of patients presenting with suspected ACS and unobstructed coronary arteries is myocarditis. The prevalence of myocarditis is variable and ranges from 15 to 75 % [16–18, 19••, 20•, 21••, 22•, 23•, 24•, 25•]. This large variation is probably due to the CMR imaging sequences being used and the timing of the scan from the acute presentation. The use of T2-weighted images for assessment of myocardial edema/inflammation and imaging patients early from the onset of symptoms increases the diagnostic pick-up rate given that some abnormalities as myocardial edema/inflammation may be reversible and resolve with time. Use of T2-weighted images for assessment of myocardial edema and scanning the patients within 2 weeks from the onset of symptom increases the diagnostic pick up rate [30••].
The non-invasive imaging diagnosis of myocarditis and myocardial inflammation always represented a diagnostic challenge because diagnosis is based on indirect signs like myocardial swelling, wall motion abnormality, and pericardial effusion, particularly with echocardiography [31]. Endomyocardial biopsy (EMB) still represents the gold standard for the diagnosis of myocarditis. Recently, several studies have validated CMR against EMB [18, 32••, 33], suggesting that CMR can have a promising role in the diagnostic pathway of these patients [34–39].
EMB is an invasive procedure and not widely available and has several limitations including low sensitivity and specificity due to sampling errors. This has fostered the increasing interest on the role of CMR in these patients. A recent Expert Position Statement of the European Society of Cardiology (ESC) confirms the important diagnostic role of CMR in patients with suspected myocarditis [40••]. Whilst CMR cannot replace EMB, there is agreement that it can be offered in clinically stable patients prior to EMB. CMR-guided EMB, i.e. obtaining the biopsy specimen from the LGE scar, can improve the diagnostic rate of the disease, as demonstrated by Mahrholdt et al. [41].
Recently, a consensus paper has defined the recommendations on the use of CMR in myocarditis [42] which led the establishment of the “Lake Louise criteria” diagnostic criteria. In particular, the CMR findings are consistent with the diagnosis of myocarditis if two of three sequences demonstrating myocardial edema, hyperemia, and fibrosis are positive.
Novel parametric mapping techniques like, native T1 mapping, extracellular volumes of distribution (ECV) and T2 mapping, currently mainly used for research, have recently shown promising results in the diagnostic assessment of myocarditis [43••]. Recent studies by Ferreira and Piechnik et al. [44••, 45••] demonstrated that native T1 mapping has a superior diagnostic role compared to conventional T2-weighted imaging, and an equivalent performance to LGE. Native T1 mapping can also display the typical non-ischemic patterns in acute myocarditis, without the need for gadolinium contrast agents [46••]. Radunski et al. recently demonstrated the utility of ECV quantification, as a measure of interstitial fibrosis in both acute and subacute, severe myocarditis [47••]. They compared the diagnostic performance of T2, T1, and ECV as novel quantitative tissue markers compared to the Lake Louise criteria. ECV quantification together with LGE imaging significantly improved the diagnostic accuracy of CMR compared with the Lake Louise criteria [47••].
Embolic MI/MI with Spontaneous Recanalisation
Acute MI with unobstructed coronary artery is a common clinical situation and is the second most common etiology in this cohort of patients (5–29 %) [16–18, 19••, 20•, 21••, 22•, 23•, 24•, 25•]. Several different patho-physiological mechanisms have been proposed to explain this phenomenon, e.g. rupture or erosion of a vulnerable plaque (causing transitory occlusion that resolves spontaneously, without leaving any residual visible intracoronary lesion), and distal vessels or small-caliber side branches disease. Other mechanisms including distal embolisation, coronary vasospasm, inflammation, or coronary dissections are rarely associated. Myocardial infarction can be diagnosed on CMR by identifying either a subendocardial or transmural LGE pattern in a typical coronary artery territory [29]. CMR can provide information on whether the myocardial infarction is acute/sub-acute orchronic. Acute ischaemic myocardial injury leads to myocardial edema, which can be delineated with T2-weighted imaging. Establishing the diagnosis in the presence of MI with unobstructed coronary arteries is very important, particularly so that appropriate management can be tailored. This can represent a plaque event or an extra-coronary embolic event. Review of coronary angiogram and coronary plaques, and excluding other sources of emboli (for example: exclude a patent foramen ovale as a potential contributor to a paradoxical embolic MI) often follows this diagnosis by CMR.
Patients with acute MI need long-term clinical follow-up and secondary atherosclerotic prevention treatment. In addition, CMR can provide further valuable prognostic information in this setting, including myocardial wall motion, global function, perfusion, and viability.
Cardiomyopathy
Cardiomyopathy is the third common cause of suspected ACS with unobstructed coronary arteries. According to literature TCM is the most frequent and occurs in 10–15 % of this patients group [16–18, 19••, 20•, 21••, 22•, 23•, 24•, 25•]. Occasionally, dilated cardiomyopathy or hypertrophic cardiomyopathy may also present with chest pain with unobstructed coronaries.
TCM or stress cardiomyopathy is a subtype of MI with unobstructed coronary artery, and defined by the characteristic wall motion abnormality that is, by definition, reversible and transient. The condition usually has a favorable prognosis compared to the other conditions. It is often, but not always, provoked by an emotional stress or respiratory distress. Several mechanisms have been hypothesized for TCM, including plaque disruption, multivessel spasm, baroreflex abnormalities, and catecholamine toxicity. It remains unclear whether TCM occurs due to one or multiple mechanisms in individual patients.
TCM is characterized by mid-cavity to apical regional wall motion abnormalities (“apical ballooning”) with sparing of the left ventricular basal segments. This can be identified by LV angiogram, as well as transthoracic echocardiography. The added diagnostic value of CMR is in its (1) high spatial resolution, 3D image acquisition, and (2) non-invasive myocardial tissue characterization. The former results in a clear detection of cardiac chambers and endocardial contours, whilst the latter allows the detection of myocardial edema (markedly present in TCM) and myocardial scarring (usually absent in TCM) [48••]. Typically, T2-weighted sequences are used to image myocardial edema and it commonly identifies the presence of circumferential and transmural myocardial edema of the apical to mid-cavity myocardium matching with the regional wall motion abnormalities [49••]. Since myocardial edema is a transient phenomenon, it is advisable that CMR imaging is carried out within the first few weeks from the acute presentation. Myocardial edema resolves in 2–3 months without any myocardial scarring and with complete functional recovery [49••]. A few studies have shown the presence of subtle late gadolinium enhancement in TCM [50•], but experimental data shows that delayed washout of gadolinium may be caused by increased interstitial water content such that associated with transient myocardial edema [51]. The subtle changes are called myocardial edema-related LGE and they do not represent myocardial necrosis. The distribution of myocardial edema matching the wall motion abnormalities with no or subtle LGE helps in distinguishing TCM from myocardial infarction and myocarditis.
Risk Stratification with CMR in ACS with Unobstructed Coronaries
ACS with unobstructed coronary arteries is a common clinical entity encountered in day-to-day clinical practice. The mean age of presentation is usually lower than ACS with obstructed coronaries [52•]. Except for cigarette smoking [53], the common risk factors for CAD such as hypertension, diabetes mellitus, and hyperlipidemia are less present than in the obstructed coronary artery group [54]. ACS with unobstructed coronaries poses a clinical dilemma, as the underlying diagnosis is variable and often unclear. Accurate diagnosis is not only important for initiation of appropriate treatment, but may also have long-term implications for the patient. Contrary to popular belief, the 1-year mortality in the overall group was shown to be non-negligible in a recent systematic review [15••]. Diagnosis is crucial as a completely normal CMR scan is associated with a good prognosis as demonstrated by the study by Chopard et al. [21••]. CMR and its unique non-invasive myocardial tissue characterization do not just have a diagnostic role but it has a potential role in risk stratification.
Risk Stratification in Myocarditis
Clinical presentation of myocarditis can be varied ranging from benign disease with preserved cardiac function to more aggressive form associated with severe LV/RV dysfunction (like giant cell myocarditis). Recent literature on myocarditis delineates its possible malignant side. Myocarditis was the third leading cause of sudden death after hypertrophic cardiomyopathy and congenital/atherosclerotic coronary artery disease, as demonstrated in a clinical case series of sudden deaths in young competitive athletes [55]. Myocarditis is responsible for 5 to 20 % of sudden deaths as demonstrated in the autopsy studies of young adults [56]. It may also resolve spontaneously without specific treatment in patients presenting with mild symptoms and minimal ventricular dysfunction [40••]. In up to 30 % of cases, biopsy-proven myocarditis can progress to DCM and is associated with a poor prognosis [40••]. CMR with its superior tissue characterization property can delineate the severity of myocarditis, thereby guiding in the management and in risk stratification. A recent study by Grun et al. has shown the presence of LGE is the best independent predictor of all-cause mortality and of cardiac mortality in 222 consecutive patients with biopsy proven viral myocarditis [57••]. LGE performed better than the traditional markers like LV ejection fraction, LV end diastolic volume, and NYHA symptom class. Moreover, normal CMR in patients with clinically suspected myocarditis, is associated with a good prognosis independent of their clinical symptoms and other findings [58••]. Thus CMR may help to distinguish a benign from malignant form of myocarditis. Prompt CMR diagnosis of an aggressive myocarditis may led to in initiation of appropriate therapy like immunosuppressants, early referral for myocardial biopsy or help in MR guided biopsy. Response to immunosuppressive therapy has been reported mainly in chronic virus-negative forms, in giant cell myocarditis, and in active myocarditis defined as autoimmune (e.g. virus-negative and autoantibody positive) [40••].
Risk Stratification in MI
CMR can also help in risk stratification in MI. In addition to help achieving the diagnosis, the better tissue characterization properties allow accurate assessment of infarct size (LGE) and myocardial salvage. The area of myocardial edema delineated by T2-weighted CMR corresponds to the myocardial area at risk (AAR). The presence and extent of myocardial salvage can also be derived with CMR by subtracting the infarcted area from the AAR [59]. There is increasing data on the prognostic value of CMR-derived infarct size and myocardial salvage [60, 61•]. Microvascular obstruction (MVO), characterized by hypoenhanced core within myocardial infarction scar (hyperenhancement) on rest first-pass perfusion or LGE imaging, can occasionally be demonstrated. The presence and extent of MVO after AMI is associated with adverse LV remodeling and poor clinical outcome [62–64], and myocardial segments with MVO at presentation are more likely to develop wall thinning and fail to demonstrate functional recovery [65]. Nijveldt et al. confirmed that MVO in LGE proved a more powerful predictor of global and regional functional recovery than the transmural extent of infarction.
CMR can potentially diagnose the complications of MI. CMR is superior to echocardiography for the identification of ventricular thrombi, particularly when they are small and apical. They are easily identifiable early after contrast administration when both the cavity and the myocardium still appear bright, whilst the thrombus appears hypointense (lack of contrast uptake given that it is avascular) [66, 67]. CMR is also able to detect other complications of MI including ventricular aneurysm, pseudoaneurysm, papillary muscle infarction with subsequent mitral regurgitation, etc.
Risk Stratification in TCM
Although TCM is usually considered to be a benign reversible condition, its arrhythmic risk is increasingly recognized. There are promising new CMR analyses which may help to risk stratify the patients with potential higher arrhythmic risk [68••].
Deep T-wave inversion and QTc interval prolongation on ECG may be observed in TCM [69•, 70]. Malignant arrhythmias including torsades de pointes (TdP) caused by repolarization abnormalities and QTc prolongation, can be seen in up to 8 % of cases [71••]. In one meta-analysis, sudden cardiac death (SCD) after TCM has been reported in 1.1 % during the index episode, with a further 0.5 % of patients suffering a SCD weeks to months later [72••]. The study primarily looked at the relationship between TCM and ventricular arrhythmias, reviewing a total 816 published cases. VF was reported in 15 cases (prevalence of 1.8 %) and VT was reported in 18 (2.2 %) [72••].
The T-wave inversion and QT interval prolongation in typical TCM is thought to be caused by an intra-cardiac gradient (apico-basal) of myocardial edema which, in turn, gives rise to regional dispersion of action potential durations [73]. A study by Perazzolo Marra et al. looked at the ECG and CMR findings in 20 consecutive TCM patients. A linear correlation of the apical-basal ratio of T2-weighted signal intensity with ECG repolarization indices such as negative T-wave magnitude, sum of the amplitudes of negative T-waves, and maximum corrected QT interval has been shown [49••]. Interestingly, the repolarization changes were unrelated to either late gadolinium enhancement or quantitative cine parameters. Hence, the T2-weighted signal intensity gradient can be potentially used as a marker of malignant arrhythmia.
CMR can also provide additional information on the presence of LV apical thrombus, valvular abnormalities, and LV outflow tract obstruction. Some of these findings are also directly linked to adverse prognosis.
Conclusion
In the context of ACS with unobstructed coronary arteries, CMR has a potentially important diagnostic role, especially in distinguishing ischemic from non-ischemic causes, thereby guiding management. CMR can also potentially help in risk stratification or prognostication in this cohort. Hence, it should be strongly considered in all patients presenting with troponin-positive chest pain with unobstructed coronaries aiming at achieving a final diagnosis. However, this is yet to be translated into routine clinical practice, particular within institutions, which do not have readily access to CMR.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Halkin A, Stone GW, Grines CL, Cox DA, Stuckey TD, Garcia E, et al. Outcomes of Patients Consented But Not Randomized in a Trial of Primary Percutaneous Coronary Intervention in Acute Myocardial Infarction (The CADILLAC Registry). Am J Cardiol. 2005;96(12):1649–55. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16360352.
Berger JS, Elliott L, Gallup D, Roe M, Granger CB, Armstrong PW, et al. Sex differences in mortality following acute coronary syndromes. JAMA. 2009;302(8):874–82.
Hochman JS, Tamis JE, Thompson TD, Weaver WD, White HD, Van de Werf F, et al. Sex, clinical presentation, and outcome in patients with acute coronary syndromes. Global Use of Strategies to Open Occluded Coronary Arteries in Acute Coronary Syndromes IIb Investigators. N Engl J Med. 1999;341(4):226–32. Available from: http://www.ncbi.nlm.nih.gov/pubmed/10413734.
Anand SS, Xie CC, Mehta S, Franzosi MG, Joyner C, Chrolavicius S, et al. Differences in the management and prognosis of women and men who suffer from acute coronary syndromes. J Am Coll Cardiol. 2005;46(10):1845–51. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16286169.
Clayton TC, Pocock SJ, Henderson RA, Poole-Wilson PA, Shaw TRD, Knight R, et al. Do men benefit more than women from an interventional strategy in patients with unstable angina or non-ST-elevation myocardial infarction? The impact of gender in the RITA 3 trial. Eur Heart J. 2004;25(18):1641–50. Available from: http://www.ncbi.nlm.nih.gov/pubmed/15351164.
Glaser R, Herrmann HC, Murphy SA, Demopoulos LA, DiBattiste PM, Cannon CP, et al. Benefit of an early invasive management strategy in women with acute coronary syndromes. JAMA. 2002;288(24):3124–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12495392.
Mega JL, Hochman JS, Scirica BM, Murphy SA, Sloan S, McCabe CH, et al. Clinical features and outcomes of women with unstable ischemic heart disease: observations from metabolic efficiency with ranolazine for less ischemia in non-ST-elevation acute coronary syndromes-thrombolysis in myocardial infarction 36 (MERLIN-TIMI 36). Circulation. 2010;121(16):1809–17. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20385930.
Gehrie ER, Reynolds HR, Chen AY, Neelon BH, Roe MT, Gibler WB, et al. Characterization and outcomes of women and men with non-ST-segment elevation myocardial infarction and nonobstructive coronary artery disease: results from the Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes with Early Implementation of the ACC/AHA Guidelines (CRUSADE) quality improvement initiative. Am Heart J. 2009;158(4):688–94.
Maddox TM, Ho PM, Roe M, Dai D, Tsai TT, Rumsfeld JS. Utilization of secondary prevention therapies in patients with nonobstructive coronary artery disease identified during cardiac catheterization: insights from the National Cardiovascular Data Registry Cath-PCI Registry. Circ Cardiovasc Qual Outcomes. 2010;3(6):632–41.
Dey S, Flather MD, Devlin G, Brieger D, Gurfinkel EP, Steg PG, et al. Sex-related differences in the presentation, treatment and outcomes among patients with acute coronary syndromes: the Global Registry of Acute Coronary Events. Heart. 2009;95(1):20–6.
Diver DJ, Bier JD, Ferreira PE, Sharaf BL, McCabe C, Thompson B, et al. Clinical and arteriographic characterization of patients with unstable angina without critical coronary arterial narrowing (from the TIMI-IIIA Trial). Am J Cardiol. 1994;74(6):531–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/8074033.
Roe MT, Harrington RA, Prosper DM, Pieper KS, Bhatt DL, Lincoff AM, et al. Clinical and therapeutic profile of patients presenting with acute coronary syndromes who do not have significant coronary artery disease.The Platelet Glycoprotein IIb/IIIa in Unstable Angina: Receptor Suppression Using Integrilin Therapy (PURSUIT) Trial. Circulation. 2000;102(10):1101–6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/10973837.
Bugiardini R, Manfrini O, De Ferrari GM. Unanswered questions for management of acute coronary syndrome: risk stratification of patients with minimal disease or normal findings on coronary angiography. Arch Intern Med. 2006;166(13):1391–5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16832004.
Alfredsson J, Lindbäck J, Wallentin L, Swahn E. Similar outcome with an invasive strategy in men and women with non-ST-elevation acute coronary syndromes: from the Swedish Web-System for Enhancement and Development of Evidence-Based Care in Heart Disease Evaluated According to Recommended Therapies (SW. Eur Heart J. 2011;32(24):3128–36. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21911338. Patients with NSTE ACS, reflecting real-life management, women and men had similar and better outcome associated with an invasive strategy.
Pasupathy S, Air T, Dreyer RP, Tavella R, Beltrame JF. Systematic review of patients presenting with suspected myocardial infarction and nonobstructive coronary arteries. Circulation. 2015;131(10):861–70. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25587100 . Myocardial infarction with non-obstructive coronary arteries can have multiple potential causes that require evaluation so that directed therapies may improve its guarded prognosis.
Assomull RG, Lyne JC, Keenan N, Gulati A, Bunce NH, Davies SW, et al. The role of cardiovascular magnetic resonance in patients presenting with chest pain, raised troponin, and unobstructed coronary arteries. Eur Heart J. 2007;28(10):1242–9.
Laraudogoitia Zaldumbide E, Pérez-David E, Larena JA, Velasco del Castillo S, Rumoroso Cuevas JR, Onaindía JJ, et al. The value of cardiac magnetic resonance in patients with acute coronary syndrome and normal coronary arteries. Rev Esp Cardiol. 2009;62(9):976–83.
Baccouche H, Mahrholdt H, Meinhardt G, Merher R, Voehringer M, Hill S, et al. Diagnostic synergy of non-invasive cardiovascular magnetic resonance and invasive endomyocardial biopsy in troponin-positive patients without coronary artery disease. Eur Heart J. 2009;30(23):2869–79. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19696191.
Leurent G, Langella B, Fougerou C, Lentz P-A, Larralde A, Bedossa M, et al. Diagnostic contributions of cardiac magnetic resonance imaging in patients presenting with elevated troponin, acute chest pain syndrome and unobstructed coronary arteries. Arch Cardiovasc Dis. 2011;104(3):161–70. CMR can diagnose the underlying etiology in nearly 90% of patients presenting with acute chest pain, elevated serum troponin and unobstructed coronary arteries.
Monney PA, Sekhri N, Burchell T, Knight C, Davies C, Deaner A, et al. Acute myocarditis presenting as acute coronary syndrome: role of early cardiac magnetic resonance in its diagnosis. Heart. 2011;97(16):1312–8. In suspected myocarditis, CMR scanning should be performed within 14 days. Myocarditis should not be regarded as benign, even when EF is preserved.
Chopard R, Jehl J, Dutheil J, Genon VD, Seronde MF, Kastler B, et al. Evolution of acute coronary syndrome with normal coronary arteries and normal cardiac magnetic resonance imaging. Arch Cardiovasc Dis. 2011;104(10):509–17. CMR is an useful tool for the management of ACS presenting with normal coronary angiography, and helps to ascertain the diagnosis and adapt treatment in a large proportion of cases. Patients with no abnormalities identified by CMR have an excellent prognosis.
Gerbaud E, Harcaut E, Coste P, Erickson M, Lederlin M, Labèque JN, et al. Cardiac magnetic resonance imaging for the diagnosis of patients presenting with chest pain, raised troponin, and unobstructed coronary arteries. Int J Cardiovasc Imaging. 2012;28(4):783–94. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21538065 . In patients with troponin-positive ACS and unobstructed coronary arteries, early CMR has important diagnostic and therapeutic implications. However its association with occurrence of MACE during mid term follow-up was not obvious.
Mahmoudi M, Harden S, Abid N, Peebles C, Nicholas Z, Jones T, et al. Troponin-positive chest pain with unobstructed coronary arteries: definitive differential diagnosis using cardiac MRI. Br J Radiol. 2012;85(1016):e461–6. CMR is a useful tool for establishing NSTEMI, and can make an important contribution to the long-term management strategy of patients presenting with troponin positive ACs and unobstructed coronaries.
Collste O, Sörensson P, Frick M, Agewall S, Daniel M, Henareh L, et al. Myocardial infarction with normal coronary arteries is common and associated with normal findings on cardiovascular magnetic resonance imaging: results from the Stockholm Myocardial Infarction with Normal Coronaries study. J Intern Med. 2013;273(2):189–96. In consecutive series of patients with ACS and unobstructed coronaries, CMR imaging helped to differentiate between myocarditis, myocardial necrosis and normal myocardium. The incidence of ACS and unobstructed coronaries was higher than previously reported.
Kawecki D, Morawiec B, Monney P, Pellaton C, Wojciechowska C, Jojko J, et al. Diagnostic contribution of cardiac magnetic resonance in patients with acute coronary syndrome and culprit-free angiograms. Med Sci Monit. 2015;21:171–80. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=4345916&tool=pmcentrez&rendertype=abstract . Evaluation of patients with ACS and unobstructed coronaries should be complemented by a CMR, if available, as the initial work-up with non-CMR tests leads to a significant proportion of misdiagnosed AMI.
Kramer CM, Barkhausen J, Flamm SD, Kim RJ, Nagel E. Standardized cardiovascular magnetic resonance (CMR) protocols 2013 update. J Cardiovasc Magn Reson. 2013;15(1):91. Available from: http://jcmr-online.com/content/15/1/91 . This document is an update to the 2008 publication of the SCMR Board of Trustees Task Force on Standardized Protocols to simplify the patient-based approach to clinical CMR.
Abdel-Aty H, Zagrosek A, Schulz-Menger J, Taylor AJ, Messroghli D, Kumar A, et al. Delayed enhancement and T2-weighted cardiovascular magnetic resonance imaging differentiate acute from chronic myocardial infarction. Circulation. 2004;109(20):2411–6. Available from: http://circ.ahajournals.org/content/109/20/2411.abstract?ijkey=1cb4d2bfe52998b203b210da6eb905e48dfe435d&keytype2=tf_ipsecsha.
McAlindon EJ, Pufulete M, Harris JM, Lawton CB, Moon JC, Manghat N, et al. Measurement of Myocardium at Risk with Cardiovascular MR: Comparison of Techniques for Edema Imaging. Radiology. 2014. 131980. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25333474. CMR sequences to detect and quantify infarct myocardial edema are not interchangeable; T2 mapping is the most reproducible method, followed by EGE, ACUT2E, and T2-weighted STIR.
Kim RJ, Fieno DS, Parrish TB, Harris K, Chen EL, Simonetti O, et al. Relationship of MRI delayed contrast enhancement to irreversible injury, infarct age, and contractile function. Circulation. 1999;100(19):1992–2002. Available from: http://www.ncbi.nlm.nih.gov/pubmed/10556226.
Ghosh Dastidar A, Singhal P, Rodrigues JC, Ahmed N, Palazzuoli A, Townsend M, et al. Improved diagnostic role of CMR in acute coronary syndromes and unobstructed coronary arteries: the importance of time-to-CMR. J Cardiovasc Magn Reson. BioMed Central. 2015. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4328297/?report=reader. The diagnostic value of CMR in patients with troponin positive ACS and unobstructed coronaries improves significantly when carried out within 2 weeks from acute presentation.
Felker GM, Boehmer JP, Hruban RH, Hutchins GM, Kasper EK, Baughman KL, et al. Echocardiographic findings in fulminant and acute myocarditis. J Am Coll Cardiol. 2000;36(1):227–32. Available from: http://www.ncbi.nlm.nih.gov/pubmed/10898439.
Lurz P, Eitel I, Adam J, Steiner J, Grothoff M, Desch S, et al. Diagnostic performance of CMR imaging compared with EMB in patients with suspected myocarditis. J Am Coll Cardiol. 2012;5(5):513–24. Available from: http://imaging.onlinejacc.org/article.aspx?articleid=1208414 . The study underline the usefulness of CMR in patients with suspected acute myocarditis against gold standard end0-myocardial biopsy.
Gutberlet M, Spors B, Thoma T, Bertram H, Denecke T, Felix R, et al. Suspected chronic myocarditis at cardiac MR: diagnostic accuracy and association with immunohistologically detected inflammation and viral persistence. Radiology. 2008;246(2):401–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18180335.
Mahrholdt H, Wagner A, Deluigi CC, Kispert E, Hager S, Meinhardt G, et al. Presentation, patterns of myocardial damage, and clinical course of viral myocarditis. Circulation. 2006;114(15):1581–90. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17015795.
Abdel-Aty H, Boyé P, Zagrosek A, Wassmuth R, Kumar A, Messroghli D, et al. Diagnostic performance of cardiovascular magnetic resonance in patients with suspected acute myocarditis: comparison of different approaches. J Am Coll Cardiol. 2005;45(11):1815–22. Available from: http://www.ncbi.nlm.nih.gov/pubmed/15936612.
Friedrich MG, Strohm O, Schulz-Menger J, Marciniak H, Luft FC, Dietz R. Contrast media-enhanced magnetic resonance imaging visualizes myocardial changes in the course of viral myocarditis. Circulation. 1998;97(18):1802–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/9603535.
Yilmaz A, Mahrholdt H, Athanasiadis A, Vogelsberg H, Meinhardt G, Voehringer M, et al. Coronary vasospasm as the underlying cause for chest pain in patients with PVB19 myocarditis. Heart. 2008;94(11):1456–63. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18230640.
Laissy J-P, Messin B, Varenne O, Iung B, Karila-Cohen D, Schouman-Claeys E, et al. MRI of acute myocarditis: a comprehensive approach based on various imaging sequences. Chest. 2002;122(5):1638–48. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12426265.
Laissy J-P, Hyafil F, Feldman LJ, Juliard J-M, Schouman-Claeys E, Steg PG, et al. Differentiating acute myocardial infarction from myocarditis: diagnostic value of early- and delayed-perfusion cardiac MR imaging. Radiology. 2005;237(1):75–82. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16126925.
Caforio ALP, Pankuweit S, Arbustini E, Basso C, Gimeno-Blanes J, Felix SB, et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2013;34(33):2636–48. 2648a – 2648d. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23824828 . This position statement of the ESC Working Group on Myocardial and Pericardial Diseases an expert consensus group reviews the current knowledge on clinical presentation, diagnosis and treatment of myocarditis, and proposes new diagnostic criteria for clinically suspected myocarditis.
Mahrholdt H, Goedecke C, Wagner A, Meinhardt G, Athanasiadis A, Vogelsberg H, et al. Cardiovascular magnetic resonance assessment of human myocarditis: a comparison to histology and molecular pathology. Circulation. 2004;109(10):1250–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/14993139.
Friedrich MG, Sechtem U, Schulz-Menger J, Holmvang G, Alakija P, Cooper LT, et al. Cardiovascular magnetic resonance in myocarditis: a JACC White Paper. J Am Coll Cardiol. 2009;53(17):1475–87. Available from: http://content.onlinejacc.org/article.aspx?articleid=1139645.
Greulich S, Ferreira VM, Dall’Armellina E, Mahrholdt H. Myocardial inflammation-are we there yet? Curr Cardiovasc Imaging Rep. 8(3):6. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=4330458&tool=pmcentrez&rendertype=abstract. This review discusses the different approaches for CMR assessment of myocardial inflammation including EGE, T2-weighted imaging, LGE, the newer mapping proton relaxation techniques (T1 pre-contrast, T1 post-contrast, T2 mapping), and the hybrid PET/MRI technique.
Ferreira VM, Piechnik SK, Dall’Armellina E, Karamitsos TD, Francis JM, Ntusi N, et al. T(1) mapping for the diagnosis of acute myocarditis using CMR: comparison to T2-weighted and late gadolinium enhanced imaging. JACC Cardiovasc Imaging. 2013;6(10):1048–58. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24011774 . Native T1 mapping is a novel criterion for the detection of acute myocarditis showed excellent and superior diagnostic performance compared with T2W-CMR. It also has a higher sensitivity compared with T2W and LGE techniques.
Piechnik SK, Ferreira VM, Lewandowski AJ, Ntusi NAB, Banerjee R, Holloway C, et al. Normal variation of magnetic resonance T1 relaxation times in the human population at 1.5 T using ShMOLLI. J Cardiovasc Magn Reson. 2013;15:13. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3610210&tool=pmcentrez&rendertype=abstract . The study assessed the variability of myocardial T1 relaxation times in the normal human population estimated with recently proposed Shortened Modified Look-Locker Inversion recovery (ShMOLLI) T1 mapping technique.
Ferreira VM, Piechnik SK, Dall’Armellina E, Karamitsos TD, Francis JM, Ntusi N, et al. Native T1-mapping detects the location, extent and patterns of acute myocarditis without the need for gadolinium contrast agents. J Cardiovasc Magn Reson. 2014;16:36. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=4041901&tool=pmcentrez&rendertype=abstract . Native T1-mapping can display the typical non-ischemic patterns in acute myocarditis, similar to LGE imaging but without the need for contrast agents.
Radunski UK, Lund GK, Stehning C, Schnackenburg B, Bohnen S, Adam G, et al. CMR in patients with severe myocarditis: diagnostic value of quantitative tissue markers including extracellular volume imaging. JACC Cardiovasc Imaging. 2014;7(7):667–75. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24954462 . In patients with clinical evidence for subacute, severe myocarditis, ECV quantification with LGE imaging significantly improved the diagnostic accuracy of CMR compared with standard Lake-Louise criteria.
Eitel I, von Knobelsdorff-Brenkenhoff F, Bernhardt P, Carbone I, Muellerleile K, Aldrovandi A, et al. Clinical characteristics and cardiovascular magnetic resonance findings in stress (takotsubo) cardiomyopathy. JAMA. 2011;306(3):277–86. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21771988 . Cardiovascular magnetic resonance imaging at the time of initial clinical presentation may provide relevant functional and tissue information that might aid in the establishment of the diagnosis of Stress Cardiomyopathy.
Perazzolo Marra M, Zorzi A, Corbetti F, De Lazzari M, Migliore F, Tona F, et al. Apicobasal gradient of left ventricular myocardial edema underlies transient T-wave inversion and QT interval prolongation (Wellens’ ECG pattern) in Tako-Tsubo cardiomyopathy. Heart Rhythm. 2013;10(1):70–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22975421 . The study showed that the ischemic-like Wellens’ ECG pattern in TakoTsubo Cardiomyopathy coincides and quantitatively correlates with the apicobasal gradient of myocardial edema as evidenced by using CMR.
Avegliano G, Huguet M, Costabel JP, Ronderos R, Bijnens B, Kuschnir P, et al. Morphologic pattern of late gadolinium enhancement in Takotsubo cardiomyopathy detected by early cardiovascular magnetic resonance. Clin Cardiol. 2011;34(3):178–82. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21400545 . Early CMR in TCM demonstrates a special morphological pattern of late gadolinium uptake that correspond to localized edema in the affected area, suggesting diffuse microcirculation damage rather than epicardial vessel involvement.
Inoue S, Murakami Y, Ochiai K, Kitamura J, Ishibashi Y, Kawamitsu H, et al. The contributory role of interstitial water in Gd-DTPA-enhanced MRI in myocardial infarction. J Magn Reson Imaging. 1999;9(2):215–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/10077016.
Agewall S, Eurenius L, Hofman-Bang C, Malmqvist K, Frick M, Jernberg T, et al. Myocardial infarction with angiographically normal coronary arteries. Atherosclerosis. 2011;219(1):10–4. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21601856 . Review article on myocardial infarction with angiographically normal coronary arteries.
Kardasz I, De Caterina R. Myocardial infarction with normal coronary arteries: a conundrum with multiple aetiologies and variable prognosis: an update. J Intern Med. 2007;261(4):330–48. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17391108.
Larsen AI, Galbraith PD, Ghali WA, Norris CM, Graham MM, Knudtson ML. Characteristics and outcomes of patients with acute myocardial infarction and angiographically normal coronary arteries. Am J Cardiol. 2005;95(2):261–3. Available from: http://www.ncbi.nlm.nih.gov/pubmed/15642564.
Maron BJ, Doerer JJ, Haas TS, Tierney DM, Mueller FO. Sudden deaths in young competitive athletes: analysis of 1866 deaths in the United States, 1980–2006. Circulation. 2009;119(8):1085–92. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19221222.
Doolan A, Langlois N, Semsarian C. Causes of sudden cardiac death in young Australians. Med J Aust. 2004;180(3):110–2. Available from: http://www.ncbi.nlm.nih.gov/pubmed/14748671.
Grün S, Schumm J, Greulich S, Wagner A, Schneider S, Bruder O, et al. Long-term follow-up of biopsy-proven viral myocarditis: predictors of mortality and incomplete recovery. J Am Coll Cardiol. 2012;59(18):1604–15. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22365425 . Prognostic role of LGE in patients with biopsy-proven viral myocarditis: Presence of LGE is the best independent predictor of all-cause mortality and of cardiac mortality.
Schumm J, Greulich S, Wagner A, Grün S, Ong P, Bentz K, et al. Cardiovascular magnetic resonance risk stratification in patients with clinically suspected myocarditis. J Cardiovasc Magn Reson. 2014;16:14. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3913958&tool=pmcentrez&rendertype=abstract . In clinically suspected myocarditis, patients with normal CMR have an excellent prognosis independent of their clinical symptoms and other findings.
Pennell D. Myocardial salvage: retrospection, resolution, and radio waves. Circulation. 2006;113(15):1821–3. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16618830.
Hombach V, Merkle N, Bernhard P, Rasche V, Rottbauer W. Prognostic significance of cardiac magnetic resonance imaging: Update 2010. Cardiol J. 2010;17(6):549–57. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21154256.
Eitel I, Desch S, de Waha S, Fuernau G, Gutberlet M, Schuler G, et al. Long-term prognostic value of myocardial salvage assessed by cardiovascular magnetic resonance in acute reperfused myocardial infarction. Heart. 2011;97(24):2038–45. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21990384 . Myocardial salvage index assessed by CMR predicts long-term clinical outcome in acute reperfused STEMI.
Hombach V, Grebe O, Merkle N, Waldenmaier S, Höher M, Kochs M, et al. Sequelae of acute myocardial infarction regarding cardiac structure and function and their prognostic significance as assessed by magnetic resonance imaging. Eur Heart J. 2005;26(6):549–57. Available from: http://eurheartj.oxfordjournals.org/content/26/6/549.abstract?ijkey=7545b91a94802e21b51b3a38c881f16d7ffb6795&keytype2=tf_ipsecsha.
Wu KC, Zerhouni EA, Judd RM, Lugo-Olivieri CH, Barouch LA, Schulman SP, et al. Prognostic significance of microvascular obstruction by magnetic resonance imaging in patients with acute myocardial infarction. Circulation. 1998;97(8):765–72. Available from: http://circ.ahajournals.org/content/97/8/765.abstract?ijkey=fde7d1413eb82a7c4c60be24ea8bf3fe8c4312cf&keytype2=tf_ipsecsha.
Taylor AJ, Al-Saadi N, Abdel-Aty H, Schulz-Menger J, Messroghli DR, Friedrich MG. Detection of acutely impaired microvascular reperfusion after infarct angioplasty with magnetic resonance imaging. Circulation. 2004;109(17):2080–5. Available from: http://circ.ahajournals.org/content/109/17/2080.abstract?ijkey=370a5241207a2dcb78c0a42731a8a98e5e7560cf&keytype2=tf_ipsecsha.
Baks T, van Geuns R-J, Biagini E, Wielopolski P, Mollet NR, Cademartiri F, et al. Effects of primary angioplasty for acute myocardial infarction on early and late infarct size and left ventricular wall characteristics. J Am Coll Cardiol. 2006;47(1):40–4. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16386662.
Mollet NR, Dymarkowski S, Volders W, Wathiong J, Herbots L, Rademakers FE, et al. Visualization of ventricular thrombi with contrast-enhanced magnetic resonance imaging in patients with ischemic heart disease. Circulation. 2002;106(23):2873–6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12460863.
Weinsaft JW, Kim HW, Shah DJ, Klem I, Crowley AL, Brosnan R, et al. Detection of left ventricular thrombus by delayed-enhancement cardiovascular magnetic resonance prevalence and markers in patients with systolic dysfunction. J Am Coll Cardiol. 2008;52(2):148–57. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18598895.
Ghosh Dastidar A, Frontera A, Palazzuoli A, Bucciarelli-Ducci C. TakoTsubo cardiomyopathy: unravelling the malignant consequences of a benign disease with cardiac magnetic resonance. Heart Fail Rev. 2015;(in press). Review of current literature on malignant side of TakoTsubo cardiomyopathy and the role of CMR in risk stratification.
Dastidar AG, Frontera A, Petersen M. A case of malignant arrhythmia in Takotsubo Cardiomyopathy. J Electrocardiol. 2014. Available from: http://www.jecgonline.com/article/S0022-0736(14)00074-0/abstract. A case of Takotsubo cardiomyopathy presenting with polymorphic VT and explanation of the pathophysiology of QTc prolongation and repolarisation abnormalities associated with the condition.
Kurisu S, Inoue I, Kawagoe T, Ishihara M, Shimatani Y, Nakamura S, et al. Time course of electrocardiographic changes in patients with tako-tsubo syndrome: comparison with acute myocardial infarction with minimal enzymatic release. Circ J. 2004;68(1):77–81. Available from: http://www.ncbi.nlm.nih.gov/pubmed/14695470.
Madias C, Fitzgibbons TP, Alsheikh-Ali AA, Bouchard JL, Kalsmith B, Garlitski AC, et al. Acquired long QT syndrome from stress cardiomyopathy is associated with ventricular arrhythmias and torsades de pointes. Heart Rhythm. 2011;8(4):555–61. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21146632 TCM can be associated with life-threatening ventricular arrhythmia in over 8% of cases. It is a recognized cause of acquired long QT syndrome.
Syed FF, Asirvatham SJ, Francis J. Arrhythmia occurrence with takotsubo cardiomyopathy: a literature review. Europace. 2011;13(6):780–8. Available from: http://europace.oxfordjournals.org/content/13/6/780. A literature review on arrhythmia occurrence with takotsubo cardiomyopathy.
Furushima H, Chinushi M, Sanada A, Aizawa Y. Ventricular repolarization gradients in a patient with takotsubo cardiomyopathy. Europace. 2008;10(9):1112–5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18567569.
Acknowledgments
This work was supported by the Bristol NIHR Cardiovascular Biomedical Research Unit at the Bristol Heart Institute. The views expressed are those of the authors and not necessarily those of the National Health Service, National Institute for Health Research, or Department of Health.
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
AG Dastidar, JCL Rodrigues, N Ahmed, A Baritussio, and C Bucciarelli-Ducci all declare no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Cardiac Magnetic Resonance
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made.
The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this licence, visit https://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dastidar, A.G., Rodrigues, J.C.L., Ahmed, N. et al. The Role of Cardiac MRI in Patients with Troponin-Positive Chest Pain and Unobstructed Coronary Arteries. Curr Cardiovasc Imaging Rep 8, 28 (2015). https://doi.org/10.1007/s12410-015-9345-x
Published:
DOI: https://doi.org/10.1007/s12410-015-9345-x