Abstract
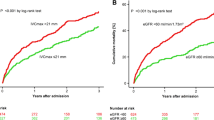
Congestion is a major determinant of clinical outcomes in heart failure (HF). We compared the acute hemodynamic effects of occlusion of the superior (SVC) versus the inferior vena cava (IVC) and tested a novel SVC occlusion system in swine models of HF. IVC occlusion acutely reduced left ventricular (LV) systolic and diastolic pressures, LV volumes, cardiac output (CO), and mean arterial pressure (MAP). SVC occlusion reduced LV diastolic pressure and volumes without affecting CO or MAP. The preCARDIA system is a balloon occlusion catheter and pump console which enables controlled delivery and removal of fluid into the occlusion balloon. At 6, 12, and 18 h, SVC therapy with the system provided a sustained reduction in cardiac filling pressures with stable CO and MAP. Intermittent SVC occlusion is a novel approach to reduce biventricular filling pressures in HF. The VENUS-HF trial will test the safety and feasibility of SVC therapy in HF.




Similar content being viewed by others
References
Benjamin, E. J., Muntner, P., Alonso, A., Bittencourt, M. S., Callaway, C. W., Carson, A. P., Chamberlain, A. M., Chang, A. R., Cheng, S., Das, S. R., Delling, F. N., Djousse, L., Elkind, M. S. V., Ferguson, J. F., Fornage, M., Jordan, L. C., Khan, S. S., Kissela, B. M., Knutson, K. L., Kwan, T. W., Lackland, D. T., Lewis, T. T., Lichtman, J. H., Longenecker, C. T., Loop, M. S., Lutsey, P. L., Martin, S. S., Matsushita, K., Moran, A. E., Mussolino, M. E., O'Flaherty, M., Pandey, A., Perak, A. M., Rosamond, W. D., Roth, G. A., Sampson, U. K. A., Satou, G. M., Schroeder, E. B., Shah, S. H., Spartano, N. L., Stokes, A., Tirschwell, D. L., Tsao, C. W., Turakhia, M. P., VanWagner, L. B., Wilkins, J. T., Wong, S. S., Virani, S. S., & American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation, 139, e56–e528. https://doi.org/10.1161/CIR.0000000000000659.
Cooper, L. B., Mentz, R. J., Stevens, S. R., et al. Hemodynamic predictors of heart failure morbidity and mortality: fluid or flow? Journal of Cardiac Failure, 22, 182–189.
Brinkley, D. M., Jr., Ho, K. K. L., Drazner, M. H., & Kociol, R. D. The prognostic value of the relationship between right atrial and pulmonary capillary wedge pressure in diverse cardiovascular conditions. American Heart Journal, 199, 31–36.
Holubarsch, C., Ruf, T., Goldstein, D. J., Ashton, R. C., Nickl, W., Pieske, B., Pioch, K., Lüdemann, J., Wiesner, S., Hasenfuss, G., Posival, H., Just, H., & Burkhoff, D. Existence of the Frank-Starling mechanism in the failing human heart. Investigations on the organ, tissue, and sarcomere levels. Circulation, 94, 683–689.
Kass, D. A., Yamazaki, T., Burkhoff, D., Maughan, W. L., & Sagawa, K. Determination of left ventricular end-systolic pressure-volume relationships by the conductance (volume) catheter technique. Circulation, 73, 586–595.
Kass, D. A., Midei, M., Graves, W., Brinker, J. A., & Maughan, W. L. Use of a conductance (volume) catheter and transient inferior vena caval occlusion for rapid determination of pressure-volume relationships in man. Catheterization and Cardiovascular Diagnosis, 15, 192–202.
Grodin, J. L., Carter, S., Bart, B. A., Goldsmith, S. R., Drazner, M. H., & Tang, W. H. W. Direct comparison of ultrafiltration to pharmacological decongestion in heart failure: a per-protocol analysis of CARRESS-HF. European Journal of Heart Failure, 20, 1148–1156. https://doi.org/10.1002/ejhf.1158.
Costanzo, M. R., Negoianu, D., Jaski, B. E., Bart, B. A., Heywood, J. T., Anand, I. S., Smelser, J. M., Kaneshige, A. M., Chomsky, D. B., Adler, E. D., Haas, G. J., Watts, J. A., Nabut, J. L., Schollmeyer, M. P., & Fonarow, G. C. Aquapheresis versus intravenous diuretics and hospitalizations for heart failure. JACC Heart Fail, 4, 95–105.
Mullens, W., Damman, K., Harjola, V. P., Mebazaa, A., Brunner-La Rocca, H. P., Martens, P., Testani, J. M., Tang, W. H. W., Orso, F., Rossignol, P., Metra, M., Filippatos, G., Seferovic, P. M., Ruschitzka, F., & Coats, A. J. The use of diuretics in heart failure with congestion – a position statement from the Heart Failure Association of the European Society of Cardiology. European Journal of Heart Failure, 21, 137–155. https://doi.org/10.1002/ejhf.1369.
Thormann, J., Kramer, W., Kindler, M., Kremer, P., & Schlepper, M. Determination of active components of amrinone by analysis of pressure-volume results; use of the conductance (volume) catheter technic and rapid load change by balloon occlusion of the inferior vena cava. Zeitschrift für Kardiologie, 76, 530–540.
Sharir, T., Feldman, M. D., Haber, H., Feldman, A. M., Marmor, A., Becker, L. C., & Kass, D. A. Ventricular systolic assessment in patients with dilated cardiomyopathy by preload-adjusted maximal power. Validation and noninvasive application. Circulation, 89, 2045–2053.
Ten Brinke, E. A., Klautz, R. J., Verwey, H. F., van der Wall, E. E., Dion, R. A., & Steendijk, P. Single-beat estimation of the left ventricular end-systolic pressure-volume relationship in patients with heart failure. Acta Physiologica (Oxford, England), 198, 37–46. https://doi.org/10.1111/j.1748-1716.2009.0x.
Kapur, N. K., Paruchuri, V., Urbano-Morales, J. A., Mackey, E. E., Daly, G. H., Qiao, X., Pandian, N., Perides, G., & Karas, R. H. Mechanically unloading the left ventricle before coronary reperfusion reduces left ventricular wall stress and myocardial infarct size. Circulation, 128, 328–336. https://doi.org/10.1161/CIRCULATIONAHA.112.000029.
Naeije, R., & Badagliacca, R. The overloaded right heart and ventricular interdependence. Cardiovascular Research, 113, 1474–1485.
Mullens, W., Abrahams, Z., Francis, G. S., Sokos, G., Taylor, D. O., Starling, R. C., Young, J. B., & Tang, W. H. Importance of venous congestion for worsening of renal function in advanced decompensated heart failure. Journal of the American College of Cardiology, 53, 589–596.
Metra, M., Cotter, G., Senger, S., Edwards, C., Cleland, J. G., Ponikowski, P., Cursack, G. C., Milo, O., Teerlink, J. R., Givertz, M. M., O'Connor, C. M., Dittrich, H. C., Bloomfield, D. M., Voors, A. A., & Davison, B. A. Prognostic significance of creatinine increases during an acute heart failure admission in patients with and without residual congestion: a post hoc analysis of the PROTECT data. Circulation. Heart Failure, 11, e004644.
Polsinelli, V. B., Sinha, A., & Shah, S. J. Visceral congestion in heart failure: right ventricular dysfunction, splanchnic hemodynamics, and the intestinal microenvironment. Current Heart Failure Reports, 14, 519–528.
Damman, K., & Testani, J. M. The kidney in heart failure: an update. European Heart Journal, 36, 1437–1444.
Kapur, N. K., Karas, R. H., Newman, S., Jorde, L., Chabrashvili, T., Annamalai, S., Esposito, M., Kimmelstiel, C. D., Lenihan, T., & Burkhoff, D. First-in-human experience with occlusion of the superior vena cava to reduce cardiac filling pressures in congestive heart failure. Catheterization and Cardiovascular Interventions, 93, 1205–1210. https://doi.org/10.1002/ccd.28326.
Funding
This work was supported by grants from the National Institutes of Health (RO1HL139785-01 and RO1HL133215-01) to N.K.K. and from MD Start Inc. to Tufts Medical Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study protocol was approved by the Institutional Animal Care and Use Committee (IACUC) at Tufts Medical Center. All experiments were performed according to the committee’s guidelines. No human studies were carried out by the authors for this article.
Conflict of Interest
NKK receives institutional grant support and consulting and speaker honoraria from Abiomed Inc., Abbott Inc., Boston Scientific Inc., Medtronic Inc., and MD Start. NKK, RHK, and DB have equity and receive consulting honoraria from Precardia. TL and JM are employees of MD Start and Precardia.
Additional information
Associate Editor Junjie Xiao oversaw the review of this article
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kapur, N.K., Reyelt, L., Crowley, P. et al. Intermittent Occlusion of the Superior Vena Cava Reduces Cardiac Filling Pressures in Preclinical Models of Heart Failure. J. of Cardiovasc. Trans. Res. 13, 151–157 (2020). https://doi.org/10.1007/s12265-019-09916-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12265-019-09916-y