Abstract
Purpose
We compared the ability of 68Ga-FAPI PET//CT with 18FDG PET/CT imaging techniques to detect additional lesions in breast cancer patients that may affect further chemotherapy options.
Methods
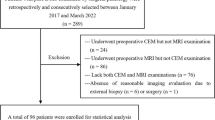
A total of 48 patients with breast cancer underwent concurrent 68Ga-FAPI-04 and 18FDG PET/CT regardless of whether they had received chemotherapy or not in the last month before imaging. Both modalities were compared according to various parameters: clinical/pathological features, number of lesions detected, activity uptake (SUVmax), and the effect on the evaluation of response to treatment in the post-chemotherapy group.
Results
This retrospective study included 48 patients with breast cancer (mean age 53.3 ± 11.7 years; IDC 89.6%; ILC 10.4%). In the comparison of both modalities, no statistical significance was obtained in terms of the pathological characteristics of the patients. More lesions were demonstrated in all categorized regions in 68Ga-FAPI PET/CT imaging with higher uptake values compared to 18FDG PET/CT in this study. In the treatment response evaluation of the post-chemotherapy group, 12 cases (12/24) who were evaluated as PMR, CMR, or SD according to 18FDG PET/CT results were later accepted as PD due to newly detected lesions in complementary 68Ga-FAPI PET/CT imaging and treatment of patients was managed accordingly by clinicians.
Conclusion
It was determined that 68Ga-FAPI PET/CT was superior to 18FDG PET/CT in terms of accuracy and it was thought that 68Ga-FAPI PET/CT could be utilized as an additional complementary imaging to 18FDG PET/CT. Moreover, 68Ga-FAPI PET/CT, with its significant theranostic potential, could become a key element in predicting the pathological response of breast cancer patients in further researches.



Similar content being viewed by others
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70:7–30.
Gradishar WJ, Moran MS, Abraham J et al. (2021) Breast Cancer, version 1.2021, NCCN clinical practice guidelines in oncology. https://www.nccn.org/. Available 15 Jan 2021.
Pharoah PDP, Sewell B, Fitzsimmons D, et al. Cost effectiveness of the NHS breast screening programme: life table model. BMJ. 2013. https://doi.org/10.1136/bmj.f2618.
Morton R, Sayma M, Sura MS. Economic analysis of the breast cancer screening program used by the UK NHS: should the program be maintained? Breast Cancer. 2017;9:217–25. https://doi.org/10.2147/BCTT.S123558.
Le Boulc’h M, Gilhodes J, Steinmeyer Z, Molière S, Mathelin C. Pretherapeutic imaging for axillary staging in breast cancer: a systematic review and meta-analysis of ultrasound, MRI and FDG PET. J Clin Med. 2021;10(7):1543. https://doi.org/10.3390/jcm10071543.
Ulaner GA, Jacene HA, Parihar AS, Groheux D. Evidence-based best practices: 18F-FDG PET staging of newly diagnosed breast cancer. Clin Nucl Med. 2021. https://doi.org/10.1097/RLU.0000000000003690.
Catanzariti F, Avendano D, Cicero G, et al. High-risk lesions of the breast: concurrent diagnostic tools and management recommendations. Insights Imaging. 2021;12:63. https://doi.org/10.1186/s13244-021-01005-6.
Kitajima K, Miyoshi Y. Present and future role of FDG-PET/CT imaging in the management of breast cancer. Jpn J Radiol. 2016;34:167–80.
Groheux D, Hindie E. Breast cancer: initial workup and staging with FDG PET/CT. Clin Transl Imaging. 2021;27:1–11. https://doi.org/10.1007/s40336-021-00426-z.
Kumar R, Chauhan A, Zhuang H, Chandra P, Schnall M, Alavi A. Clinicopathologic factors associated with false negative FDG-PET in primary breast cancer. Breast Cancer Res Treat. 2006;98:267–74.
Avril N, Rose CA, Schelling M, Dose J, Kuhn W, Bense S, et al. Breast imaging with positron emission tomography and fluorine-18 fluorodeoxyglucose: use and limitations. J Clin Oncol. 2000;18:3495–502.
Hirose Y, Kaida H, Ishibashi M, Kawahara A, Kobayashi M, Hayabuchi N. Glucose transporter expression of intraductal papilloma of the breast detected by fluorodeoxyglucose positron emission tomography. Jpn J Radiol. 2011;29:217–21.
Rufini V, Calcagni ML, Baum RP. Imaging of neuroendocrine tumours. Semin Nucl Med. 2006;36:228–47.
Dong R, Guo J, Zhang Z, Zhou Y, Hua Y. Polyphyllin I inhibits gastric cancer cell proliferation by downregulating the expression of fibroblast activation protein alpha (FAP) and hepatocyte growth factor (HGF) in cancer-associated fibroblasts. Biochem Biophys Res Commun. 2018;497(4):1129.
Ruan P, Tao Z, Tan A. Low expression of miR-30a-5p induced the proliferation and invasion of oral cancer via promoting the expression of FAP. Biosci Rep. 2018;38(1):BSR20171027.
Hamson EJ, Keane FM, Tholen S, Schilling O, Gorrell MD. Understanding fibroblast activation protein (FAP): substrates, activities, expression and targeting for cancer therapy. Proteom Clin Appl. 2014;8(5–6):454–63.
Gorrell MD, Park JE, Rawlings NL, Salvesen G, editors. Handbook of proteolytic enzymes. 3rd ed. San Diego: Elsevier; 2013. p. 3395–401.
Giesel F, Kratochwil C, Lindner T, et al. 68Ga-FAPI PET/CT: biodistribution and preliminary dosimetry estimate of 2 DOTA-containing FAP-targeting agents in patients with various cancers. J Nucl Med. 2019;60:386–92.
Kratochwil C, Flechsig P, Lindner T, Abderrahim L, Altmann A, Mier W, Adeberg S, Rathke H, Röhrich M, Winter H, Plinkert PK, Marme F, Lang M, Kauczor HU, Jäger D, Debus J, Haberkorn U, Giesel FL. 68Ga-FAPI PET/CT: tracer uptake in 28 different kinds of cancer. J Nucl Med. 2019;60(6):801–5.
Koerber SA, Staudinger F, Kratochwil C, Adeberg S, Haefner MF, Ungerechts G, Rathke H, Winter E, Lindner T, Syed M, Bhatti IA, Herfarth K, Choyke PL, Jaeger D, Haberkorn U, Debus J, Giesel FL. The role of 68Ga-FAPI PET/CT for patients with malignancies of the lower gastrointestinal tract: first clinical experience. J Nucl Med. 2020;61(9):1331–6. https://doi.org/10.2967/jnumed.119.237016.
Guo W, Pang Y, Yao L, Zhao L, Fan C, Ke J, Guo P, Hao B, Fu H, Xie C, Lin Q, Wu H, Sun L, Chen H. Imaging fibroblast activation protein in liver cancer: a single-center post hoc retrospective analysis to compare [68Ga]Ga-FAPI-04 PET/CT versus MRI and [18F]-FDG PET/CT. Eur J Nucl Med Mol Imaging. 2021;48(5):1604–17. https://doi.org/10.1007/s00259-020-05095-0.
Hyun OJ, Lodge MA, Wahl RL. Practical PERCIST: a simplified guide to PET response criteria in solid tumors 1.0. Radiology. 2016;280:576–84. https://doi.org/10.1148/radiol.2016142043.
Karnoub AE, Dash AB, Vo AP, Sullivan A, Brooks MW, Bell GW, Richardson AL, Polyak K, Tubo R, Weinberg RA. Mesenchymal stem cells within tumour stroma promote breast cancer metastasis. Nature. 2007;449:557–63.
Hwang RF, Moore T, Arumugam T, Ramachandran V, Amos KD, Rivera A, Ji B, Evans DB, Logsdon CD. Cancer-associated stromal fibroblasts promote pancreatic tumor progression. Cancer Res. 2008;68:918–26.
Muerkoster S, Wegehenkel K, Arlt A, Witt M, Sipos B, Kruse ML, Sebens T, Kloppel G, Kalthoff H, Folsch UR, et al. Tumor stroma interactions induce chemoresistance in pancreatic ductal carcinoma cells involving increased secretion and paracrine effects of nitric oxide and interleukin-1beta. Cancer Res. 2004;64:1331–7.
Shekhar MP, Santner S, Carolin KA, Tait L. Direct involvement of breast tumor fibroblasts in the modulation of tamoxifen sensitivity. Am J Pathol. 2007;170:1546–60.
Hasebe T, et al. Highly proliferative fibroblasts forming fibrotic focus govern metastasis of invasive ductal carcinoma of the breast. Mod Pathol. 2001;14(4):325–37.
Orimo A, et al. Stromal fibroblasts present in invasive human breast carcinomas promote tumor growth and angiogenesis through elevated SDF-1/CXCL12 secretion. Cell. 2005;121(3):335–48.
Stuelten CH, et al. Transient tumor-fibroblast interactions increase tumor cell malignancy by a TGF-Beta mediated mechanism in a mouse xenograft model of breast cancer. PLoS ONE. 2010;5(3):e9832.
Hu M, et al. Role of COX-2 in epithelial-stromal cell interactions and progression of ductal carcinoma in situ of the breast. Proc Natl Acad Sci USA. 2009;106(9):3372–7 (PubMed: 19218449).
Finak G, Bertos N, Pepin F, Sadekova S, Souleimanova M, Zhao H, Chen H, Omeroglu G, Meterissian S, Omeroglu A, et al. Stromal gene expression predicts clinical outcome in breast cancer. Nat Med. 2008;14:518–27.
Cirri P, Chiarugi P. Cancer associated fibroblasts: the dark side of the coin. Am J Cancer Res. 2011;1:482–97.
Ariga N, Sato E, Ohuchi N, Nagura H, Ohtani H. Stromal expression of fibroblast activation protein/seprase, a cell membrane serine proteinase and gelatinase, is associated with longer survival in patients with invasive ductal carcinoma of breast. Int J Cancer. 2001;95(1):67–72.
Henry LR, Lee HO, Lee JS, Klein-Szanto A, Watts P, Ross EA, Chen WT, Cheng JD. Clinical implications of fibroblast activation protein in patients with colon cancer. Clin Cancer Res. 2007;13(6):1736–41.
Cohen SJ, Alpaugh RK, Palazzo I, Meropol NJ, Rogatko A, Xu Z, Hoffman JP, Weiner LM, Cheng JD. Fibroblast activation protein and its relationship to clinical outcome in pancreatic adenocarcinoma. Pancreas. 2008;37(2):154–8.
Goscinski MA, Suo Z, Florenes VA, Vlatkovic L, Nesland JM, Giecksky KE. FAP-alpha and uPA show different expression patterns in premalignant and malignant esophageal lesions. Ultrastruct Pathol. 2008;32(3):89–96.
Kelly T, Kechelava S, Rozypal TL, West KW, Korourian S. Seprase, a membrane bound protease, is overexpressed by invasive ductal carcinoma cells of human breast cancers. Mod Pathol. 1998;11(9):855–63.
Okada K, Chen WT, Iwasa S, Jin X, Yamane T, Ooi A, Mitsumata M. Seprase, a membrane-type serine protease, has different expression patterns in intestinal- and diffuse-type gastric cancer. Oncology. 2003;65(4):363–70.
Jin X, Iwasa S, Okada K, Mitsumata M, Ooi A. Expression patterns of seprase, a membrane serine protease, in cervical carcinoma and cervical intraepithelial neoplasm. Anticancer Res. 2003;23(4):3195–8.
Dohi O, Ohtani H, Hatori M, Sato E, Hosaka M, Nagura H, Itoh E, Kokubun S. Histogenesis-specific expression of fibroblast activation protein and dipeptidylpeptidase-IV in human bone and soft tissue tumours. Histopathology. 2009;55(4):432–40.
Mentlein R, Hattermann K, Hemion C, Jungbluth AA, Held-Feindt J. Expression and role of the cell surface protease seprase/fibroblast activation protein alpha (FAP-alpha) in astroglial tumours. Biol Chem. 2011;392(3):199–207.
Taveira M. Comparison of 68Ga-FAPI versus 18F-FDG PET/CT for initial cancer staging. Radiol Imaging Cancer. 2021;3(2): e219007. https://doi.org/10.1148/rycan.2021219007.
Chen H, Zhao L, Ruan D, Pang Y, Hao B, Dai Y, Wu X, Guo W, Fan C, Wu J, Huang W, Lin Q, Sun L, Wu H. Usefulness of [68Ga]Ga-DOTA-FAPI-04 PET/CT in patients presenting with inconclusive [18F]FDG PET/CT findings. Eur J Nucl Med Mol Imaging. 2021;48(1):73–86. https://doi.org/10.1007/s00259-020-04940-6.
Aide N, Elie N, Blanc-Fournier C, Levy C, Salomon T, Lasnon C. Hormonal receptor immunochemistry heterogeneity and 18F-FDG metabolic heterogeneity: preliminary results of their relationship and prognostic value in luminal non-metastatic breast cancers. Front Oncol. 2021;12(10): 599050. https://doi.org/10.3389/fonc.2020.599050.
Kömek H, Can C, Güzel Y, Oruç Z, Gündoğan C, Yildirim ÖA, Kaplan İ, Erdur E, Yıldırım MS, Çakabay B. 68Ga-FAPI-04 PET/CT, a new step in breast cancer imaging: a comparative pilot study with the 18F-FDG PET/CT. Ann Nucl Med. 2021;35(6):744–52. https://doi.org/10.1007/s12149-021-01616-5.
Sarikaya I. Breast cancer and PET imaging. Nucl Med Rev Cent East Eur. 2021;24:16–26.
de Cremoux P, Biard L, Poirot B, Bertheau P, Teixeira L, Lehmann-Che J, Bouhidel FA, Merlet P, Espié M, Resche-Rigon M, Sotiriou C, Groheux D. 18FDG-PET/CT and molecular markers to predict response to neoadjuvant chemotherapy and outcome in HER2-negative advanced luminal breast cancers patients. Oncotarget. 2018;9(23):16343–53. https://doi.org/10.18632/oncotarget.24674.
Aogi K, Kadoya T, Sugawara Y, Kiyoto S, Shigematsu H, Masumoto N, Okada M. Utility of (18)F FDG-PET/CT for predicting prognosis of luminal-type breast cancer. Breast Cancer Res Treat. 2015;150(1):209–17. https://doi.org/10.1007/s10549-015-3303-9.
Chen H, Pang Y, Wu J, Zhao L, Hao B, Wu J, Wei J, Wu S, Zhao L, Luo Z, Lin X, Xie C, Sun L, Lin Q, Wu H. Comparison of [68Ga]Ga-DOTA-FAPI-04 and [18F] FDG PET/CT for the diagnosis of primary and metastatic lesions in patients with various types of cancer. Eur J Nucl Med Mol Imaging. 2020;47(8):1820–32. https://doi.org/10.1007/s00259-020-04769-z.
Gu B, Luo Z, He X, Wang J, Song S. 68Ga-FAPI and 18F-FDG PET/CT images in a patient with extrapulmonary tuberculosis mimicking malignant tumor. Clin Nucl Med. 2020;45(11):865–7. https://doi.org/10.1097/RLU.0000000000003279.
Sonni I, Lee-Felker S, Memarzadeh S, Quinn MM, Mona CE, Lückerath K, Czernin J, Calais J. 68Ga-FAPi-46 diffuse bilateral breast uptake in a patient with cervical cancer after hormonal stimulation. Eur J Nucl Med Mol Imaging. 2021;48(3):924–6. https://doi.org/10.1007/s00259-020-04947-z.
Wang LJ, Zhang Y, Wu HB. Intense diffuse uptake of 68Ga-FAPI-04 in the breasts found by PET/CT in a patient with advanced nasopharyngeal carcinoma. Clin Nucl Med. 2021;46(5):e293–5. https://doi.org/10.1097/RLU.0000000000003487.
Aroztegui APC, Vicente AMG, Ruiz SA, Bolton RCD, Rincon JO, Garzon JRG, de Arcocha Torres M, Garcia-Velloso MJ. 18F-FDG PET/CT in breast cancer: evidence-based recommendations in initial staging. Tumour Biol. 2017;39(10):1010428317728285. https://doi.org/10.1177/1010428317728285.
Tian F, Shen G, Deng Y, Diao W, Jia Z. The accuracy of 18F-FDG PET/CT in predicting the pathological response to neoadjuvant chemotherapy in patients with breast cancer: a meta-analysis and systematic review. Eur Radiol. 2017;27(11):4786–96. https://doi.org/10.1007/s00330-017-4831-y.
Keam B, Im SA, Koh Y, Han SW, Oh DY, Cho N, Kim JH, Han W, Kang KW, Moon WK, Kim TY, Park IA, Noh DY, Chung JK, Bang YJ. Early metabolic response using FDG PET/CT and molecular phenotypes of breast cancer treated with neoadjuvant chemotherapy. BMC Cancer. 2011;20(11):452. https://doi.org/10.1186/1471-2407-11-452.
Funding
No funding was received from any source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval and consent to participate
All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Elboga, U., Sahin, E., Kus, T. et al. Superiority of 68Ga-FAPI PET/CT scan in detecting additional lesions compared to 18FDG PET/CT scan in breast cancer. Ann Nucl Med 35, 1321–1331 (2021). https://doi.org/10.1007/s12149-021-01672-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-021-01672-x