Abstract
Despite remarkable advances in the knowledge of molecular biology and treatment, ovarian cancer remains the leading cause of death from gynecologic cancer. In the last decade, there have been important advances both in systemic and surgical treatment. However, there is no doubt that the incorporation of PARP inhibitors as maintenance after the response to platinum-based chemotherapy, first in recurrent disease and recently also in first line, will change the natural history of the disease.
The objective of this guide is to summarize the current evidence for the diagnosis, treatment, and follow-up of ovarian cancer, and to provide evidence-based recommendations for clinical practice.
Similar content being viewed by others
Introduction
Epithelial ovarian cancer (OC) remains the 5th cause of death in women and the first cause of death due to gynecological cancer. In the last two decades, we have assisted to achievements in the knowledge of molecular biology, surgical outcome, chemotherapy administration, and implementation of antiangiogenic therapy that have translated into clinically significant improvements in the time of disease control and overall survival in some cases. More recently, the incorporation of Poly ADP Ribose Polymerase (PARP) inhibitors as maintenance after response to platinum-based chemotherapy seems to start changing the natural history of the disease and the aim of decreasing the mortality is becoming a reality. This SEOM guideline is providing updated evidence-based recommendation for the current treatment of ovarian, primary peritoneal and fallopian tube cancer, globally considered as OC along the guideline.
Methodology
This guideline has been developed with the consensus of ten oncologists, with high expertise in OC treatment, from the cooperative group GEICO (Spanish Group for Investigation in Ovarian Cancer) and SEOM (Spanish Society of Medical Oncology). To assign a level and quality of evidence and a grade of recommendation to the different statements of this treatment guideline, the Infectious Diseases Society of America-US Public Health Service Grading System for Ranking Recommendations in Clinical Guidelines was used.
Diagnosis and staging
Early-stage OC is frequently associated to non-specific symptoms, but in late-stages ascites, abdominal disorders and/or pleural effusion are common. In women with symptoms suggestive of OC, physical examination, laboratory testing with CA 125 and pelvic ultrasonography are recommended at a first level [II, A]. High levels of HE4 identify malignancy with a similar sensitivity than CA 125, but with higher specificity. Both CA 125 and HE4 are included in the Risk Ovarian Malignancy Algorithm (ROMA), used for calculating the risk of malignancy of adnexal masses.
In patients with presumed OC, computed tomography (CT) imaging of the thorax, abdomen and pelvis will define the extent of the disease and provide information to plan treatment options [II, A]. Magnetic resonance imaging (MRI) and Positron Emission Tomography (PET)-CT are not included in the routine preoperative staging but could improve the accuracy of the evaluation of the advanced disease [II, B]. Laparoscopic surgery is a mainstay not only in staging of OC but also in pathological diagnosis [II, B]. FIGO 2014 is the staging system currently recommended [1] (Table 1).
Pathology and biomarkers
According to the WHO classification, there are five major subtypes of epithelial ovarian carcinoma: high-grade serous (HGSC), low-grade serous (LGSC), clear cell (CCC), endometrioid (EC), and mucinous (MC). The use of an immunohistochemical (IHC) panel including Wilms Tumor 1 (WT1), p53, progesterone receptor (PR), and Napsin A (NAPSA) has been suggested to assist in the diagnosis of cases in which the histological type is difficult to establish [2] [II, A]. The OC subtypes differ not only in IHC expression but also in molecular features (Table 2). Furthermore, in non-mucinous tumors, a study of germinal (and somatic if possible) BRCA mutation must be completed after pathological diagnosis due to its implications on hereditary counseling, prognostic information, and therapeutic strategy [I, A]. For therapeutic decisions, it would be desirable to have also information on tumor homologous recombination (HR) status [I, A].
Early stages
Surgery
The treatment for early-stage OC (stages I-II) consists of a staging surgery that includes hysterectomy with bilateral salpingo-oophorectomy, bilateral pelvic and para-aortic lymphadenectomy, omentectomy, random peritoneal biopsies, peritoneal washing, and careful inspection and palpation of all peritoneal surfaces, the serosa of the entire digestive tract and the bowel mesentery [II, A]. Lymph node dissection can safely be omitted in grade I mucinous tumors. Both open and laparoscopic approaches are acceptable as long as an experienced gynaecologic oncologist performs all the procedure [3] [II, A]. In patients referred to after incomplete surgery, a re-staging procedure should be offered [III, A].
Fertility-sparing surgery, based on a unilateral salpingo-oophorectomy and complete surgical staging can be safely offered to all stage IA, and IC1 low-grade ovarian carcinomas [II, A].
Adjuvant treatment
Adjuvant platinum-based chemotherapy after staging surgery is indicated in high-risk early stages (IA/B high grade, IC-IIA) [I, A]. The benefit is uncertain and should be discussed on individually in: Grade 1–2 EC stage IB/IC, MC with expansile invasion stage IB/IC, MC with infiltrative invasion stage IA, LGSC stage IB/IC, and CCC stage IA-IC1 [4].
The recommended regimen is paclitaxel-carboplatin, but single-agent carboplatin is also considered a reasonable option [I, A]. 6-cycle regimen is recommended in HGSC, but the optimal duration remains controversial in the rest of histologic subtypes, in which three cycles can be accepted [4] [I, A].
Advanced disease: front-line treatment
Cytoreductive surgery
Cytoreductive surgery plays a crucial role in the treatment of advanced OC (stages III and IV). The presence of visible residual disease after cytoreduction is a major prognostic factor with an important negative impact on survival. Thus, the goal must be to obtain a complete cytoreduction [II, A]. In this context surgical effort must be maximal and may include histerectomy, double anexectomy, omentectomy, extensive peritonectomy, bowel resection or excision of any enlarge nodes. Due to the recent results of Lion trial lymphadenectomy in primary completely debulked advanced OC with clinically negative lymph nodes is not further recommended [5] [I, A].
Several studies and meta-analysis suggest that the expertise of the surgeon is of utmost importance in the outcomes and thus the recommendation is that patients should be operated in highly experienced centers [6] [II, A].
Neoadjuvant chemotherapy
The EORTC55971 trial and the CHORUS trial showed a similar progression-free survival (PFS) and overall survival (OS) for patients with stage IIIC or IV disease receiving neoadjuvant chemotherapy (NACT) and interval debulking surgery (IDS) compared with primary debulking surgery (PDS). In spite of these non-inferiority results, these aforementioned trials have been criticized because of the median OS, mean operative time and low rates of optimal cytoreduction.
Therefore, both approaches (PDS or NACT followed by IDS) can be considered valid, although PDS remains as the preferred primary treatment when complete cytoreduction is feasible and patient is operable [4] [I, A].
Chemotherapy regimen and route of administration
Standard post-operative treatment in advanced OC consists of a combination of carboplatin (AUC 5–6) and paclitaxel (175 mg/m2) every 3 weeks for six cycles [I, A].
Incorporation of weekly chemotherapy into first-line treatment does not improve PFS or OS in the population of western countries [7]. Moreover, single agent carboplatin or weekly chemotherapy could have even worse outcomes in vulnerable elderly patients, as shown by EWOC-1 trial, so that 3-weekly regimen remains the standard for all OC populations [I, A].
Three large randomized studies (GOG 104, GOG 114, and GOG 172) and one meta-analysis have found clinically significant improvements in PFS and OS with intraperitoneal (IP) chemotherapy [8]. However, in the GOG 252 trial the duration of PFS was not significantly increased with either IP regimen when bevacizumab was incorporated in all arms, and IP cisplatin arm was associated to higher toxicity [9]. Therefore, and according to last ESMO-ESGO consensus, currently IP chemotherapy is not a standard of care [4] [III, A]. Nevertheless, it could still be considered in selected patients (stage III, < 1 cm residual disease) as long as bevacizumab is not used [I, B].
A randomized phase III trial evaluating hyperthermic intraperitoneal chemotherapy (HIPEC) after IDS showed a better OS for HIPEC arm. However, this trial has received significant methodological criticisms, so HIPEC cannot be considered a standard treatment and should not be offered out of clinical trials [4] [I, C].
Bevacizumab
Two large randomized studies (GOG 218 and ICON 7) have reported that bevacizumab added to the initial chemotherapy followed by a maintenance period improves PFS in comparison with standard chemotherapy alone [10, 11]. None of these trials showed an OS benefit in the overall study populations but post hoc subgroup analysis indicated statistically significant OS benefit in patients with stage IV disease in GOG 218 (18) and patients at high risk of progression (defined as FIGO stage III with > 1 cm residual disease after PDS or stage IV) in the ICON7 trial.
Bevacizumab (15 mg/kg or 7.5 mg/kg every 3 weeks for a maximum of 15 months) should be considered in addition to carboplatin and paclitaxel, and it is especially recommended in patients with stage III and residual disease or stage IV [I, A].
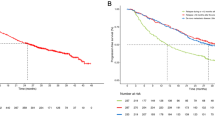
Maintenance treatment with PARP inhibitors
Four randomized phase III trials (SOLO-1, PRIMA, PAOLA-1 and VELIA) have shown that maintenance treatment with PARP inhibitors (PARPi) after response to front-line platinum-containing regimens increased significantly the median PFS in HGSOC [12,13,14,15]. Table 3 summarizes differences in the design between these trials and the results in the ITT and the different biomarker subgroup populations. All trials have shown a remarkable and unprecedented benefit in BRCAmut. In addition, PAOLA-1 and PRIMA demonstrated also a significant benefit in HR deficient (HRD) population. Finally, only PRIMA showed a benefit in the HR proficient (HRP) subgroup although of lesser magnitude. The benefit observed with PARPi is sustained along the follow-up as demonstrated by the impact on PFS2, as well as by the results after a 5-year follow-up of the SOLO-1 showing that almost 50% of patients remain progression-free in contrast to 21% in the control arm.
Based on these results, olaparib (with or without bevacizumab) or niraparib after partial or complete response to first-line platinum-based chemotherapy are highly effective in BRCA-mutated patients and strongly recommended [I, A].
According to PAOLA-1 and PRIMA results, niraparib or olaparib-bevacizumab are also highly recommended for patients with HRD tumors [I, A]. In the HRP subgroup maintenance with niraparib can also be considered although bevacizumab remains as a reasonable alternative [I, B].
Recurrent disease
Approximately, 80–85% of patients with advanced OC will relapse in the first 10 years after the diagnosis [16]. When planning treatment for recurrent disease, first considerations must be willingness of the patient to receive further therapy and performance status (PS). Next step is to decide if platinum might be the best option taking into account the following factors. Conversely, the traditional and arbitrary classification as platinum-sensitive and platinum-resistance has been abandoned during the Fifth Ovarian Cancer Consensus Conference (OCCC) of the GCIG and the ESMO-ESGO consensus [4, 17].
Factors to consider when selecting therapy
Depending on the tumour: Site and extension of the disease, histological subtype, BRCA mutation status.
Depending on the patient: Treatment-free interval. Platinum-free interval (TFIp) has classically been considered a predictive factor of response to platinum-rechallenge. Also TFInp (non-platinum) or TFIb (biological) should be considered as well as number of previous therapies, residual toxicity, patient preferences and comorbidities with special attention to geriatric population [17].
Surgery for relapsed ovarian cancer
The randomized Desktop III trial has shown a significant OS benefit of surgery at relapse among patients accomplishing AGO score. Therefore, surgery should be recommended for patients with TFIp > 6 months, no residual disease after first surgery, good PS (0–1), and absence or less than 500 ml of ascites [18] [I, A]. In addition, PET-CT could improve the selection of candidates for secondary cytoreduction [19] [II, B].
Systemic treatment when platinum might be the best option
A platinum-based combination (with paclitaxel, gemcitabine or pegylated liposomal doxorubicin -PLD-) is associated with a longer PFS and OS compared to single-agent platinum. None of these combinations can be considered superior in terms of efficacy; the doublet selection should be based on the toxicity profile.
A randomized phase III trial of bevacizumab combined with carboplatin-gemcitabine, in patients in first relapse who have not been treated with antiangiogenic therapy, has shown a benefit in response rate (RR) and PFS [20]. The combination of bevacizumab with carboplatin and paclitaxel in this setting has also shown improvement in PFS [21]. Recently, the combination carboplatin-PLD and bevacizumab have shown benefit in PFS and OS over carboplatin-gemcitabine and bevacizumab [22].
Three PARP inhibitors (olaparib [23] niraparib [24] and rucaparib [25]) have shown benefit in PFS as maintenance treatment after response to platinum based therapy in relapsed ovarian cancer. The magnitude of benefit is greater, but not limited, to patients with BRCA mutation. For BRCA-mutated patients maintenance treatment with olaparib improves PFS (HR 0.30) and OS (HR 0.74) with an improvement of 12.9 months in median OS vs placebo. Niraparib and rucaparib have also shown positive results in phase III trials, not only in BRCA-mutated patients but also in BRCA wild type (wt), regardless the status of HR.
Therefore, when platinum might be the best option both platinum-based combination with bevacizumab and platinum-based combination followed by PARPi are optimal options [I, A]. Based on the higher RR with the addition of bevacizumab, this option would be indicated for symptomatic patients, without BRCA mutation, who did not receive bevacizumab at first line. For the rest of patients, platinum-based combination followed by PARPi would be the preferred option [III, A]. For BRCA-mutated patients olaparib, niraparib or rucaparib can be used, and for BRCAwt patients niraparib or rucaparib are the available options [I, A].
If BRCA is mutated, monotherapy with rucaparib (not as maintenance) is also an alternative for patients with no previous PARPi treatment, who have been treated with two or more prior lines of platinum-based chemotherapy, and who are unable to tolerate further platinum-based chemotherapy [II, B].
In patients with TFIp > 6 months who cannot receive platinum-based therapy, or after previous use of PARPi and at least two platinum regimens, the combination trabectedin plus PLD could be an option [I, B].
Systemic treatment when platinum might not be the best option
Patients progressing on platinum-based therapy or after a short treatment-free interval of platinum are not considered eligible for re-challenge with platinum. This is an unmet medical need and when possible, patients should be included in clinical trials. Cytotoxic agents, such as weekly paclitaxel, PLD, gemcitabine and topotecan, have shown modest activity in phase III randomized trials, with an average RR of 10–15% and median OS in the range of 9–12 months. Accordingly, sequential cytotoxic single-agent therapy is the best palliative option and quality of life is the most important endpoint. Nevertheless, patients with poor PS could be considered only for best supportive care.
For patients who have not received prior bevacizumab, the addition of the latter to weekly paclitaxel, PLD, or topotecan has shown to improve PFS. The combination weekly paclitaxel and bevacizumab was especially active in Aurelia trial, being the preferred option when possible [26].
In summary, when platinum might not be not the best option single-drug therapy, or in combination with bevacizumab if not previously received, is recommended [I, A].
Follow-up
Table 4 summarized our recommendations for follow-up. Although performing a routine imaging is controversial we recommended to do it at least every 6 months. It is important to review any new symptom reported by the patient and to perform a physical examination in each visit.
References
Prat J, FIGO Committee on Gynecologic Oncology. Staging classification for cancer of the ovary, fallopian tube, and peritoneum. Int J Gynaecol Oncol. 2014;124:1–5.
Kobel M, Rahimi K, Rambau PF, Naugler C, Le Page C, Meunier L, et al. An immunohistochemical algorithm for ovarian carcinoma typing. Int J Gynecol Pathol. 2016;35:430–41.
Park HJ, Kim DW, Yim GW, et al. Staging laparoscopy for the management of early-stage ovarian cancer: a metaanalysis. Am J Obstet Gynecol. 2013;209(58):e1.
Colombo N, Sessa C, du Bois A, et al. ESMO-ESGO consensus conference recommendations on ovarian cancer: pathology and molecular biology, early and advanced stages, borderline tumours and recurrent disease. Ann Oncol. 2019;30:672–705.
Harter P, Sehouli J, Lorusso D, Reuss A, Vergote I, Marth C, et al. A randomized trial of lymphadenectomy in patients with advanced ovarian neoplasms. N Eng J Med. 2019;380:822–32.
du Bois A, Rochon J, Pfisterer J, Hoskins WJ. Variations in institutional infrastructure, physician specialization and experience, and outcome in ovarian cancer: a systematic review. Gynecol Oncol. 2009;112:422–36.
Clamp A, James E, McNeish I, et al. Weekly dose-dense chemotherapy in first-line epithelial ovarian, fallopian tube, or primary peritoneal carcinoma treatment (ICON8): primary progression free survival analysis results from a GCIG phase 3 randomised controlled trial. Lancet. 2019;394:2084–95.
Jaaback K, Johnson N, Lawrie TA. Intraperitoneal chemotherapy for the initial management of primary epithelial ovarian cancer. Cochrane Database Syst Rev. 2011; 11: CD005340. Update in: Cochrane Database Syst Rev. 2016; 1: CD005340.
Walker JL, Brady MF, Wenzel L, et al. Randomized trial of intravenous versus intraperitoneal chemotherapy plus bevacizumab in advanced ovarian carcinoma: an NRG Oncology/Gynecologic Oncology Group Study. J Clin Oncol. 2019;37:1380–90.
Burger RA, Brady MF, Bookman MA, et al. Incorporation of bevacizu-mab in the primary treatment of ovarian cancer. N Engl J Med. 2011;365:2473–83.
Perren TJ, Swart AM, Pfisterer J, et al. A phase 3 trial of bevacizumab in ovarian cancer. N Engl J Med. 2011;365:2484–96.
Moore K, Colombo N, Scambia G, et al. Maintenance Olaparib in patients with newly diagnosed advanced ovarian cancer. N Engl J Med. 2018;379:2495–505.
Ray Coquard I, Pautier P, Pignata S, et al. Olaparib plus bevacizumab as firstline maintenance in ovarian cancer. N Engl J Med. 2019;381:2416–28.
Gonzalez-Martín A, Pothuri B, Vergote I, et al. Niraparib in patients with newly diagnosed advanced ovarian cancer. N Engl J Med. 2019;381:2391–402.
Coleman RL, Fleming GF, Brady MF, et al. Veliparib with first line chemotherapy and as maintenance therapy in ovarian cancer. N Engl J Med. 2019;381:2403–15.
Narod S. Can advanced-stage ovarian cancer be cured? Nat Rev Clin Oncol. 2016;13:255–61.
Wilson MK, Pujade-Lauraine E, Aoki D, et al. Fifth ovarian cancer consensus conference of the gynecologic cancer intergroup: recurrent disease. Ann Oncol. 2017;28:727–32.
Du Bois A, Sehouli J, Vergote I, et al. Randomized phase III study to evaluate the impact of secondary cytoreductive surgery in recurrent ovarian cancer: Final analysis of AGO DESKTOP III/ENGOT-ov20. J Clin Oncol. 2020; 38 (suppl;abstr 6000).
Bristow RE, del Carmen MG, Pannu HK, et al. Clinically occult recurrent ovarian cancer: patient selection for secondary cytoreductive surgery using combined PET/CT. Gynecol Oncol. 2003;90:519–28.
Aghajanian C, Blank SV, Goff BA, et al. OCEANS: a randomized, double-blind, placebo-controlled phase III trial of chemotherapy with or without bevacizumab in patients with platinum-sensitive recurrent epithelial ovarian, primary peritoneal, or fallopian tube cancer. J Clin Oncol. 2012;30:2039–45.
Coleman RL, Brady MF, Herzog TJ, et al. Bevacizumab and paclitaxel-carboplatin chemotherapy and secondary cytoredutcion in recurrent, platinum-sensitive ovarian cancer (NRG Oncology/Gynecologic Oncology Group study GOG-0213): a multicentre, open-label, randomized, phase 3 trial. Lancet Oncol. 2017;18:779–91.
Pfisterer J, Shannon CM, Baumann K, AGO-OVAR 2.21/ENGOT-ov 18 Investigators, et al. Bevacizumab and platinum-based combinations for recurrent ovarian cancer: a randomised, open-label, phase 3 trial. Lancet Oncol. 2020;21:699–709.
Pujade-Lauraine E, Lederman J, Selle F, et al. Olaparib tablets as maintenance therapy in patients with platinum-sensitive, relapsed ovarian cancer and BRCA1/2 mutation (SOLO2/ENGOT-OV21): a double-blind, randomized, placebo-controlled, phase 3 trial. Lancet Oncol. 2017;18:1274–84.
Mirza MR, Monk BJ, Herrstedt J, et al. Niraparib maintenance therapy in platinum-sensitive, recurrent ovarian cancer. N Engl J Med. 2016;375:2154–64.
Coleman RL, Oza AM, Lorusso D, et al. Rucaparib maintenance treatment for recurrent ovarian carcinoma after response to platinum therapy (ARIEL3): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2017;390:1949–61.
Pujade-Lauraine E, Hilpert F, Weber B, et al. Bevacizumab combined with chemotherapy for platinum-resistant recurrent ovarian cancer: the AURELIA open-label randomized phase III trial. J Clin Oncol. 2014;32:1302–8.
Author information
Authors and Affiliations
Contributions
All authors have contributed equally to this manuscript.
Corresponding author
Ethics declarations
Conflict of interest
AR reports honoraria and advisory/consultancy (MSD, AstraZeneca, Roche, GSK, Clovis, PharmaMar, Lilly, Amgen), research grant/funding to his institution (Eisai, PharmaMar, Roche), travel/accommodation/expenses (AstraZeneca, Tesaro: A GSK Company, PharmaMar, Roche), and speakers bureau (MSD, AstraZeneca, Roche, GSK, Clovis, PharmaMar), outside the submitted work. EG has received advisory/consultancy honorarium from AstraZeneca-MSD, Clovis Oncology, GSK-Tesaro, PharmaMar, Roche; has received speaker bureau/expert testimony honorarium from AstraZeneca, PharmaMar, Roche, GSK; and has received travel/accommodation/expenses from Roche, TESARO: A GSK Company and Baxter. LM has received advisory/consultancy honorarium from AstraZeneca, Clovis Oncology, Genmab, GSK, Merck Sharp & Dohme, Novartis, Pfizer/Merck, PharmaMar, Roche; has received speaker bureau/expert testimony honorarium from AstraZeneca, PharmaMar, Roche, GSK, Roche; has received research grant/funding from TESARO: A GSK Company; and has received travel/accommodation/expenses from AstraZeneca, Novartis, Roche, TESARO: A GSK Company. CML reports honoraria and advisory/consultancy (AstraZeneca, Clovis Oncology, GSK, MSD, PharmaMar, Roche); travel/accommodation/expenses (AstraZeneca, Clovis Oncology, GSK, MSD, PharmaMar, Roche); and speakers bureau (AstraZeneca, Clovis Oncology, GSK, MSD, PharmaMar, Roche). JMG has served on Advisory for PharmaMar, GSK and Amgen; travel and accommodation from PharmaMar and GSK. JAPF declares advisory board: Roche, Astrazeneca, GSK, Clovis, Pharmamar, Abilify Pharma, Amgen; Travel/Expenses: Roche, Astrazeneca, Pfizer, GSK; Speaker: Roche, Astrazeneca, GSK, Clovis, Pharmamar, Novartis; Institutional support: GSK, Novartis. MQV reports honoraria and advisory/Consultancy from AstraZeneca, GSK, MerckSharp & Dohme, Novartis, PharmaMar, Roche, Bristol-Myers Squibb,Pierre Fabre; Travel/Accommodation/Expenses from AstraZeneca, Pharmamar, Roche, GSK, Merck Sharp&Dohme and speakers bureau AstraZeneca, GSK, MerckSharp & Dohme, Novartis, PharmaMar, Roche, Bristol-Myers Squibb, Pierre-fabre. MJR has served on advisory boards for MSD, AstraZeneca, Roche, GSK, Clovis, PharmaMar and received support for travel or accommodation from Roche, AstraZeneca, and PharmaMar. MPBG has served on Advisory boards for Roche, AstraZeneca, PharmaMar, Clovis Oncology, GSK, Merck Sharp & Dohme; has received speaker bureau honoraria from AstraZeneca, Roche, PharmaMar, GSK, Clovis Oncology, Merck Sharp & Dohme and received support for travel or accommodation from Roche, AstraZeneca, GSK and PharmaMar. AGM reports honoraria and advisory/Consultancy: Amgen, AstraZeneca, Clovis Oncology, Genmab, GSK, ImmunoGen, Merck Sharp & Dohme, Novartis, Oncoinvent, Pfizer/Merck, PharmaMar, Roche, Sotio; Speaker Bureau: AstraZeneca, PharmaMar, Roche, GSK; Research Grant/Funding: Roche, TESARO: A GSK Company and Travel/Accommodation/Expenses: AstraZeneca, Pharmamar Roche, TESARO: A GSK Company.
Ethical approval
The current manuscript has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
All authors are members of SEOM and GEICO (Grupo Español de Investigación en Cáncer de Ovario) and this manuscript is considered also as the GEICO Guideline on Ovarian Cancer.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Redondo, A., Guerra, E., Manso, L. et al. SEOM clinical guideline in ovarian cancer (2020). Clin Transl Oncol 23, 961–968 (2021). https://doi.org/10.1007/s12094-020-02545-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-020-02545-x