Abstract
Background
Liver resection for hepatocellular carcinoma (HCC) patients with portal vein tumor thrombus (PVTT) offers a chance of cure, although survival is often limited. The actual 3-year survival and its associated prognostic factors have not been reported.
Methods
A nationwide database of HCC patients with PVTT who underwent liver resection with ‘curative’ intent was analyzed. The clinicopathologic characteristics, the perioperative, and survival outcomes for the actual long-term survivors were compared with the non-long-term survivors (patients who died within 3 years of surgery). Univariable and multivariable regression analyses were performed to identify predictive factors associated with long-term survival outcomes.
Results
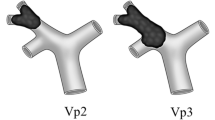
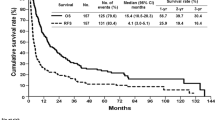
The study included 1590 patients with an actuarial 3-year survival of 16.6%, while the actual 3-year survival rate was 11.7%. There were 171 patients who survived for at least 3 years after surgery and 1290 who died within 3 years of surgery. Multivariable regression analysis revealed that total bilirubin > 17.1 μmol/l, AFP > 400 ng/ml, types of hepatectomy, extent of PVTT, intraoperative blood loss > 400 ml, tumor diameter > 5 cm, tumor encapsulation, R0 resection, liver cirrhosis, adjuvant TACE, postoperative early recurrence (< 1 year), and recurrence treatments were independent prognostic factors associated with actual long-term survival.
Conclusion
One in nine HCC patients with PVTT reached the long-term survival milestone of 3 years after resection. Major hepatectomy, controlling intraoperative blood loss, R0 resection, adjuvant TACE, and ‘curative’ treatment for initial recurrence should be considered for patients to achieve better long-term survival outcomes.



Similar content being viewed by others
References
European Association for the Study of the Liver. Electronic address eee, European Association for the study of the L. EASL clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2018;69(1):182–236.
Bruix J, Sherman M. American Association for the study of liver D. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53(3):1020–2.
Schoniger-Hekele M, Muller C, Kutilek M, Oesterreicher C, Ferenci P, Gangl A. Hepatocellular carcinoma in Central Europe: prognostic features and survival. Gut. 2001;48(1):103–9.
Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, Blanc JF, et al. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med. 2008;359(4):378–90.
Cheng AL, Kang YK, Chen Z, Tsao CJ, Qin S, Kim JS, et al. Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: a phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol. 2009;10(1):25–34.
Shi J, Lai E, Li N, Guo W, Xue J, Lau W, et al. A new classification for hepatocellular carcinoma with portal vein tumor thrombus. J Hepatobiliary Pancreat Sci. 2011;18(1):74–80.
Kokudo T, Hasegawa K, Matsuyama Y, Takayama T, Izumi N, Kadoya M, et al. Survival benefit of liver resection for hepatocellular carcinoma associated with portal vein invasion. J Hepatol. 2016;65(5):938–43.
Zhang XP, Gao YZ, Chen ZH, Chen MS, Li LQ, Wen TF, et al. An eastern hepatobiliary surgery hospital/portal vein tumor thrombus scoring system as an aid to decision making on hepatectomy for hepatocellular carcinoma patients with portal vein tumor thrombus: a multicenter study. Hepatology. 2019;69(5):2076–90.
Kamiyama T, Kakisaka T, Orimo T, Wakayama K. Hepatectomy for hepatocellular carcinoma with portal vein tumor thrombus. World J Hepatol. 2017;9(36):1296–304.
Sakamoto K, Nagano H. Surgical treatment for advanced hepatocellular carcinoma with portal vein tumor thrombus. Hepatol Res. 2017;47(10):957–62.
Chen XP, Qiu FZ, Wu ZD, Zhang ZW, Huang ZY, Chen YF, et al. Effects of location and extension of portal vein tumor thrombus on long-term outcomes of surgical treatment for hepatocellular carcinoma. Ann Surg Oncol. 2006;13(7):940–6.
Shi J, Lai E, Li N, Guo W, Xue J, Lau W, et al. Surgical treatment of hepatocellular carcinoma with portal vein tumor thrombus. Ann Surg Oncol. 2010;17(8):2073–80.
Peng ZW, Guo RP, Zhang YJ, Lin XJ, Chen MS, Lau WY. Hepatic resection versus transcatheter arterial chemoembolization for the treatment of hepatocellular carcinoma with portal vein tumor thrombus. Cancer. 2012;118(19):4725–36.
Strasberg SM, Phillips C. Use and dissemination of the brisbane 2000 nomenclature of liver anatomy and resections. Ann Surg. 2013;257(3):377–82.
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien–Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–96.
Wang K, Guo WX, Chen MS, Mao YL, Sun BC, Shi J, et al. Multimodality treatment for hepatocellular carcinoma with portal vein tumor thrombus. Medicine. 2016;95(11):e3015.
Liu PH, Lee YH, Hsia CY, Hsu CY, Huang YH, Chiou YY, et al. Surgical resection versus transarterial chemoembolization for hepatocellular carcinoma with portal vein tumor thrombosis: a propensity score analysis. Ann Surg Oncol. 2014;21(6):1825–33.
Zheng N, Wei X, Zhang D, Chai W, Che M, Wang J, et al. Hepatic resection or transarterial chemoembolization for hepatocellular carcinoma with portal vein tumor thrombus. Medicine (Baltimore). 2016;95(26):e3959.
Hiraoka A, Michitaka K, Kumada T, Izumi N, Kadoya M, Kokudo N, et al. Validation and potential of albumin-bilirubin grade and prognostication in a nationwide survey of 46,681 hepatocellular carcinoma patients in japan: the need for a more detailed evaluation of hepatic function. Liver Cancer. 2017;6(4):325–36.
Pesi B, Giudici F, Moraldi L, Montesi G, Romagnoli S, Pinelli F, et al. Hepatocellular carcinoma on cirrhosis complicated with tumoral thrombi extended to the right atrium: results in three cases treated with major hepatectomy and thrombectomy under hypothermic cardiocirculatory arrest and literature review. World J Surg Oncol. 2016;14:83.
Katz SC, Shia J, Liau KH, Gonen M, Ruo L, Jarnagin WR, et al. Operative blood loss independently predicts recurrence and survival after resection of hepatocellular carcinoma. Ann Surg. 2009;249(4):617–23.
Zhang XP, Gao YZ, Chen ZH, Wang K, Cheng YQ, Guo WX, et al. In-hospital mortality after surgical resection in hepatocellular carcinoma patients with portal vein tumor thrombus. J Cancer. 2019;10(1):72–80.
Yoshida Y, Kanematsu T, Matsumata T, Takenaka K, Sugimachi K. Surgical margin and recurrence after resection of hepatocellular carcinoma in patients with cirrhosis. Further evaluation of limited hepatic resection. Ann Surg. 1989;209(3):297–301.
Goh BK, Chow PK, Teo JY, Wong JS, Chan CY, Cheow PC, et al. Number of nodules, child-pugh status, margin positivity, and microvascular invasion, but not tumor size, are prognostic factors of survival after liver resection for multifocal hepatocellular carcinoma. J Gastrointest Surg. 2014;18(8):1477–85.
Sun JJ, Wang K, Zhang CZ, Guo WX, Shi J, Cong WM, et al. Postoperative adjuvant transcatheter arterial chemoembolization after R0 hepatectomy improves outcomes of patients who have hepatocellular carcinoma with microvascular invasion. Ann Surg Oncol. 2016;23(4):1344–51.
Zhang XP, Liu YC, Chen ZH, Sun JX, Wang K, Chai ZT, et al. Postoperative adjuvant transarterial chemoembolization improves outcomes of hepatocellular carcinoma associated with hepatic vein invasion: a propensity score matching analysis. Ann Surg Oncol. 2019;26(5):1465–73.
Chen ZH, Zhang XP, Zhou TF, Wang K, Wang H, Chai ZT, et al. Adjuvant transarterial chemoembolization improves survival outcomes in hepatocellular carcinoma with microvascular invasion: a systematic review and meta-analysis. Eur J Surg Oncol. 2019;45(11):2188–96.
Poon RT. Differentiating early and late recurrences after resection of HCC in cirrhotic patients: implications on surveillance, prevention, and treatment strategies. Ann Surg Oncol. 2009;16(4):792–4.
Zhang XP, Chen ZH, Zhou TF, Li LQ, Chen MS, Wen TF, et al. A nomogram to predict early postoperative recurrence of hepatocellular carcinoma with portal vein tumour thrombus after R0 liver resection: a large-scale, multicenter study. Eur J Surg Oncol. 2019;45(9):1644–51.
Brown ZJ, Greten TF, Heinrich B. Adjuvant treatment of hepatocellular carcinoma: prospect of immunotherapy. Hepatology. 2019;70(4):1437–42.
Funding
This study was supported by the Key Project of Natural Science Foundation of China (No: 81730097); the National Key Basic Research Programme ‘973 project’ (No: 2015CB554000); the National Natural Science Foundation of China (No: 81602523); the Shanghai Municipal Health Bureau (No: SHDC12015106); and the Shanghai Science and Technology Committee (No: 134119a0200).
Author information
Authors and Affiliations
Contributions
Shu-Qun Cheng, Wan Yee Lau, Zhen-Hua Chen, Xiu-Ping Zhang, Yu-Gang Lu, and Meng-Chao Wu contributed to conception and design, Shu-Qun Cheng contributed to financial support, Le-Qun Li, Min-Shan Chen,Tian-Fu Wen, Wei-Dong Jia, Dong Zhou, Jing Li, Ding-Hua Yang, Zuo-Jun Zhen, Yi-Jun Xia, Rui-Fang Fan, Yang-Qing Huang, Yu Zhang, Xiao-Jing Wu, Yi-Ren Hu, Yu-Fu Tang, Jian-Hua Lin, Fan Zhang, Cheng-Qian Zhong, Wei-Xing Guo, and Jie Shi contributed to provision of study materials or patients, Zhen-Hua Chen, Xiu-Ping Zhang, and Yu-Gang Lu contributed to collection and assembly of data, Zhen-Hua Chen, Xiu-Ping Zhang, and Yu-Gang Lu contributed to data analysis and interpretation, Zhen-Hua Chen, and Wan Yee Lau wrote the manuscript, all authors approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
No potential conflicts of interest were disclosed.
Ethical approval
This study was approved by the Institutional Ethics Committee of the Eastern Hepatobiliary Surgery Hospital, the Sun Yat-sen University Cancer Centre, the Affiliated Tumor Hospital of Guangxi Medical University, the West China Hospital, the Affiliated Provincial Hospital of Anhui Medical University, Fujian Provincial Cancer Hospital, Xinqiao Hospital, the Affiliated Southern Hospital of Southern Medical University, the Foshan First People’s Hospital, the Inner Mongolia People’s Hospital, the No.940 Hospital of Joint Logistics Support Force, the Shanghai Public Health Center, the Sichuan Provincial People’s Hospital, the First People’s Hospital of Xuzhou, the Wenzhou People’s Hospital, the General Hospital of Northern War Zone, the Second Affiliated Hospital of Wenzhou Medical University, the Affiliated Hospital of Binzhou Medical College, and the LongYan First Hospital Affiliated to Fujian Medical University.
Informed consent
Informed consent was obtained from the patients for their data to be used for research purposes.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chen, ZH., Zhang, XP., Lu, YG. et al. Actual long-term survival in HCC patients with portal vein tumor thrombus after liver resection: a nationwide study. Hepatol Int 14, 754–764 (2020). https://doi.org/10.1007/s12072-020-10032-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-020-10032-2